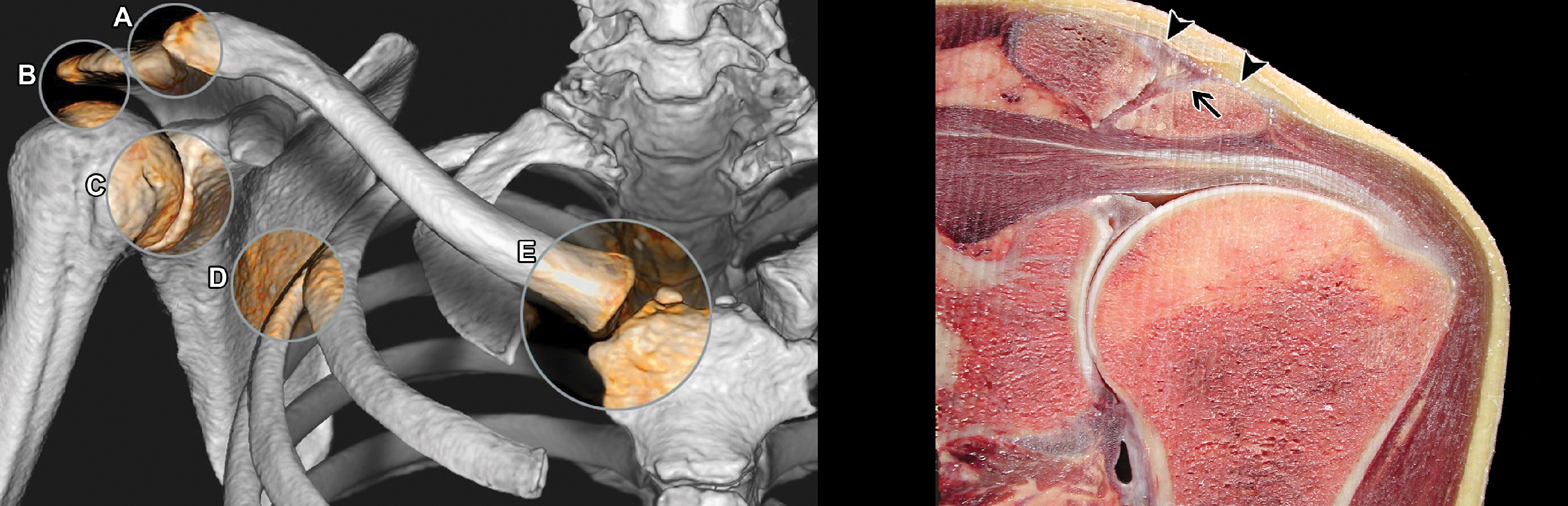
The NSPS is the most important component of passive stabilization of the anterior humeral head. Tendon rupture at the anterior edge of the socket is the most common injury causing anterior traumatic shoulder instability. An NSPS tendon rupture can also occur on the shoulder side.

- Ultrasound of the shoulder joint (lecture at Diagnostrum)
- Shoulder joint during ultrasound examination
- What is supination and pronation?
- But what about pronation and supination of the arms?
- biomechanics of the shoulder
- Static structures and mechanoreceptors
- Exercise phase in rehabilitation
- Therapeutic exercises after a shoulder fracture
- LFC in the first phase of a humerus fracture
- Therapy of humerus fractures in the second phase
- Subacromial space
- Scapulothoracic joint
- AXIAL VIEW OF THE SHOULDER JOINT
- X-RAYS OF THE SHOULDER SHOULD BE TAKEN IN DIRECT BACK PROJECTION.
- Deltoid muscle
- shoulder rotator cuff
- rotation
- Application in bodybuilding
Ultrasound of the shoulder joint (lecture at Diagnostrum)
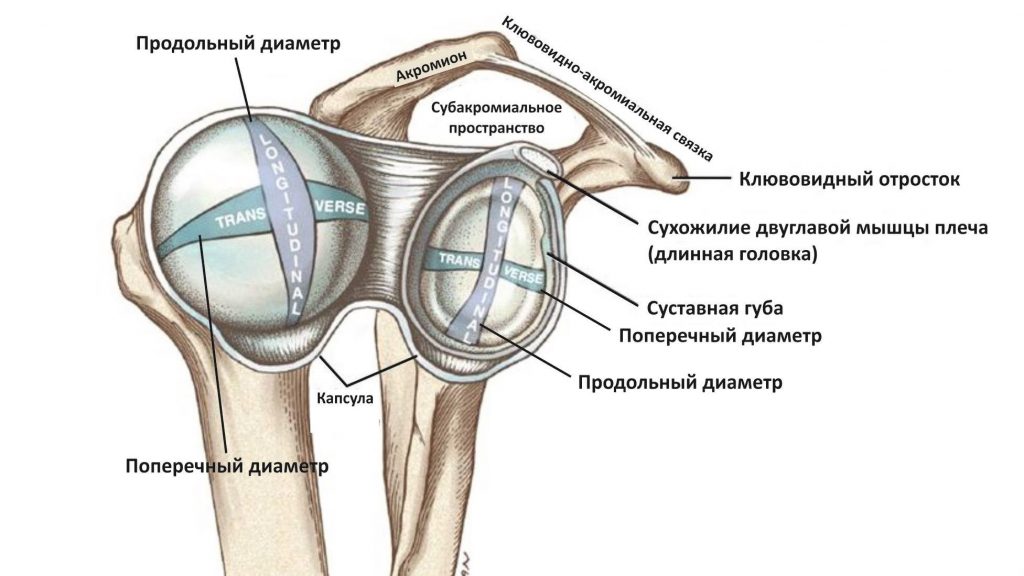
The shoulder joint is formed by the head of the humerus and the articular surface of the scapula (glenoid); The acromioclavicular joint connects the shoulder blade to the collarbone and the shoulder to the ribcage.
Due to the shallow shoulder socket and the relatively large spherical humeral head, the glenoid joint is very mobile and most susceptible to dislocation.
The glenoid is twice as deep in the superior-basal part as in the anterior-basal part, which means that the humeral head can be displaced anteriorly much more easily.
The head of the humerus is held in the joint by a static stabilizer, the fibrous membrane, and a dynamic stabilizer, the rotator cuff and shoulder girdle muscles.
The synovial membrane increases the contact area between the humeral head and the acetabulum and provides an attachment point for the glenohumeral ligaments and the tendon of the long head of the biceps brachii muscle.
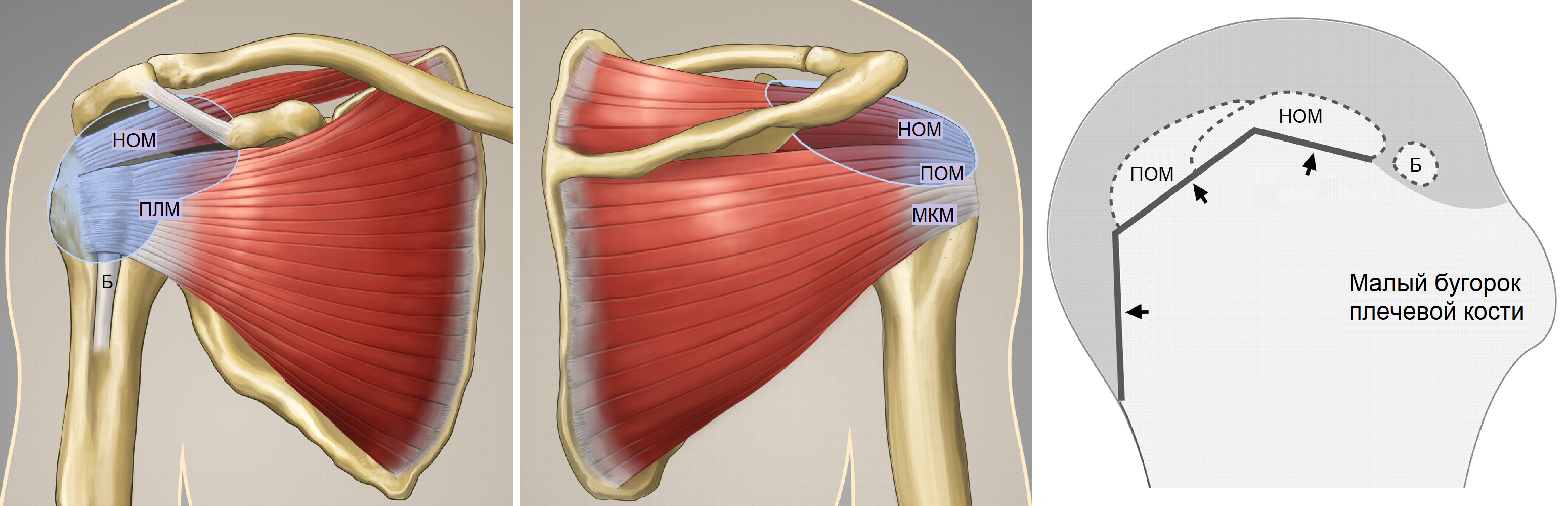
The scapula, scapula, scapula, and the small circular muscle begin at the scapula and attach to the head of the humerus to form the rotator cuff of the glenohumeral joint.
A NOTICE!!! A linear transducer of 6-18 mHz is suitable for examining the shoulder joint, with the tracer always oriented cranially or to the right.
Shoulder joint during ultrasound examination
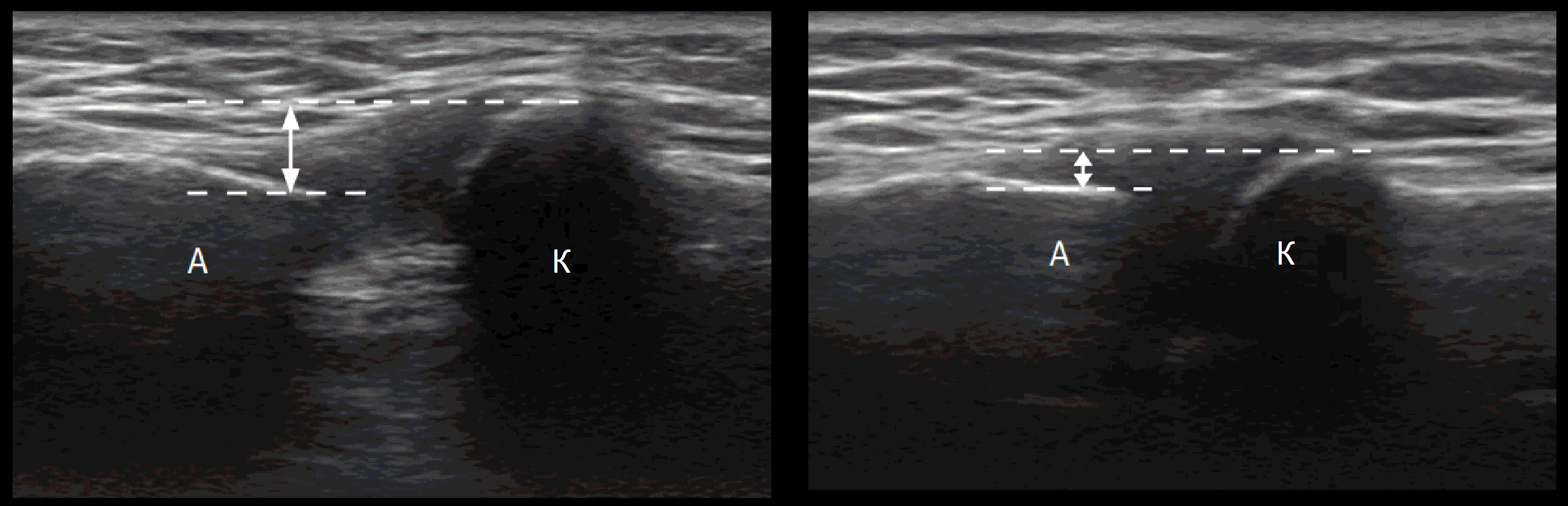
It is advisable to begin the ultrasound examination of the shoulder complex at the acromioclavicular joint; this joint is flat and has an intra-articular fibrocartilage disc that is destroyed by the age of 40.
The patient sits, hand on knee, palm up; we move the probe along the clavicle, the AC joint looks like a hypoechoic V-zone between the outer end of the clavicle and the acromion.
Ultrasound is used to assess the expansion of the AC joint on the healthy side and determine horizontal alignment; when the AC ligament is completely torn, the acromion moves downward.
Dynamic examination can detect instability: from a neutral position, the hand is placed on the opposite shoulder and minimal changes (up to 1 mm) in the healthy AC joint are noted.

What is supination and pronation?
To understand what we are talking about here, it is necessary to know the terms supination and pronation. They are often used in books and articles about training.
supination – is the outward rotational movement of a limb or part of a limb. For example, supinating a hand flexed 90 degrees at the elbow rotates the hand from a downward palm to an upward palm. In the drawing this is marked by the number 1.
It doesn't matter how much the hand is bent at the elbow. Rotation in the direction indicated by arrow 1 is always supination.
pronation – is the opposite of supination, a rotational movement that is directed inwards. If you hold a handful of coins in your hand and then decide to supinate them, you need to pronate.
The use of the terms pronation and supination in relation to the hand is more or less well known. They are particularly popular on bodybuilding forums for training biceps and forearm muscles.
But what about pronation and supination of the arms?
You hear about this much less often. And not without reason.
This photo shows an athlete supinating the shoulder joint.
biomechanics of the shoulder
The shoulder area is known to be one of the most difficult areas to assess and rehabilitate. Because of the numerous joints involved in shoulder movement, the term 'shoulder complex' is appropriate. For effective rehabilitation of shoulder injuries, it is necessary to understand the functional anatomy underlying the biomechanics of the shoulder complex.
The shoulder complex consists of 3 physiological joints and a 'mobile' joint:
When assessing the shoulder joint, the contribution of the sternoclavicular and riboclavicular joints should also be considered.
The LHS is the only point of attachment of the upper limbs to the axial skeleton. The LGS involves sliding movement of the scapula along the trunk and no bony fixation. The LGS is of particular interest in understanding the mechanism of injury to the shoulder joint because it is osteologically predisposed to instability.
The shoulder-scapula joint is formed by the head of the humerus (convex surface) and the socket of the scapula (concave surface). Due to the relatively large surface area of the humeral head relative to the acetabulum, this joint has limited bone congruence and is therefore highly dependent on the surrounding soft tissues to support the structure.
Furthermore, it was calculated that only 25 % of the surface of the humeral head articulates with the shoulder joint socket. The surrounding passive structures (labrum, joint capsule and ligaments) as well as the active structures (muscles and associated tendons) work together to maintain the dynamic stability of the PLS.
- Rotation (flexion and extension).
- Sliding down (during adduction).
- Gliding upwards (with adduction).
- Backward slide (during internal rotation).
- Gliding forward (during external rotation).
Static structures and mechanoreceptors
In addition to the intricate network of ligamentous structures that connect neighboring bones, the importance of the surrounding musculature cannot be overstated. Active muscle contractions are essential for maintaining stability of the shoulder complex.
The muscles of the shoulder complex can be divided into global shoulder motors and finely tuned stabilizers of the individual joints. Larger muscles such as trapezius, scapulae, pectoralis major, deltoid, serratus, dorsiflexion, rhomboid, circular major, biceps, pectoralis minor and triceps are involved in various shoulder movements. They provide the gross movements of the upper quadrant.
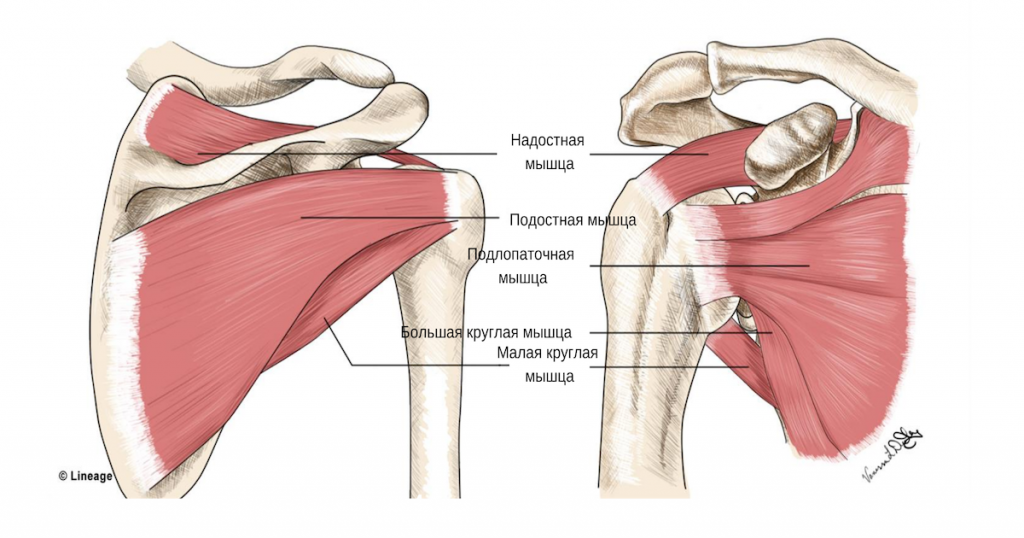
The stabilizing muscles of the PLS: the supraspinatus muscle, the scapularis muscle, the scapularis muscle and the lever muscle belong to the category of rotator cuff muscles and are attached to the head of the humerus in the articular fossa. Together, they act as dynamic stabilizers of the PLS joint by maintaining the central position of the humeral head within the articular fossa under both static and dynamic conditions. It is thought that the tendons of the rotator cuff muscles are connected to the ligaments and synovial membrane, so contractions of these muscles can provide additional stabilization of the PLS by strengthening the static structures during movement.
Synchronized contractions of the rotator cuff muscles center the humeral head during movement. This avoids physical damage to the tissue (located primarily anterior and superior to the PLS) that is associated with shoulder injury and pain. As previously mentioned, due to their anatomical location in the subacromial space, the rotator cuff tendons are particularly susceptible to compression, abnormal friction, and ultimately entrapment during active activities. Correct positioning of the humeral head is important for correct PPS movements and daily activities.
Exercise phase in rehabilitation
Seven to eight weeks after the fracture of the humerus, the patient regains full function of the injured shoulder and upper extremity under the supervision of the rehabilitation department of Yusupov Hospital. Other physical exercises are aimed at strengthening muscles and restoring full range of motion. LFC should be performed 3 to 4 times per day. The patient is given a series of exercises, each of which should be repeated 10-12 times.
The therapeutic exercises in this phase of recovery from a shoulder fracture consist of the following exercises:
- Raising the shoulder in front of the patient from a standing position;
- Abduction, adduction, rotation, pronation and supination of the upper extremity;
- handstands and push-ups;
- Overhanging on a pole or wall bars;
- Manipulations with dumbbells up to a maximum weight of 5 kg and with medballs.
Stretching exercises such as placing a gymnastic bar or towel behind your back or walking up and down a wall with your toes are also effective. These manipulations will help you regain full shoulder mobility in all directions.
With a proper rehabilitation program, it takes 2 to 3 months for a patient with a shoulder fracture to fully recover. Only after this time do rehabilitation therapists recommend exercises to develop stretching, physical strength and endurance.
Therapeutic exercises after a shoulder fracture
Therapeutic exercises after a shoulder fracture begin 10-14 days after the plaster cast is applied. Patients initially perform passive exercises, followed by active exercises with a further increase in workload. The goals of physical therapy after a shoulder fracture are as follows:
The rehabilitation doctor puts together an individual exercise program for each patient. To begin, the patient performs the following exercises:
- Rocking the upper extremity back and forth in the shoulder joint with muscle relaxation, flexing the trunk towards the injured shoulder;
- clenching and stretching of fingers;
- Flexion and extension of the elbow joints by grasping the lower third of the forearm of the injured limb with the healthy hand.
At the end of the second week, the physiotherapist recommends making small rocking movements from side to side and small circles with the extended arm. On the fifteenth day, exercises are performed that prepare the arm to raise it horizontally: the amplitude of the swinging movements of the straight arm is increased, the limb is rocked from side to side, and the injured arm is briefly pushed with the healthy arm . There are a variety of therapeutic exercises for broken shoulder joints. You can find videos about this on the Internet. Rehabilitation doctors at Yusupov Hospital do not recommend performing these exercises without consulting a specialist.
The patient can slightly tilt the upper body towards the injured shoulder, throw the arm behind the back, bend it at the elbow and gradually increase the amplitude. Slowly raise your elbows to relieve pressure on your deltoids by supporting your upper body with your palms. Rotating the shoulder joint while tilting the upper body towards the painful limb (the arm hanging freely with the elbow extended) is also effective. The elbow can be retracted to a horizontal position with the healthy limb supporting the lower third of the forearm of the injured arm. For this exercise, the injured arm must be bent at the elbow at an acute angle.
LFC in the first phase of a humerus fracture
- Anatomical humerus neck (intra-articular fracture);
- surgical humeral neck (extra-articular fracture);
- Diaphysis (main part) of the humerus;
- the distal part near the elbow.
Fractures of the surgical humerus neck are particularly dangerous. They can cause damage to the neurovascular bundle and paresis of the limb. In the initial phase of treatment, the choice of physiotherapeutic methods after a surgical humeral neck fracture depends on the type and severity of the injury and the immobilization method chosen. The greatest amount of movement with a Y bandage and a minimum of movement, consisting primarily of static muscle tension and the sending of mental impulses, is used with a thoraco-radial bandage. In strictly transverse diaphyseal humerus fractures, which are reduced with an internal pin, and in displaced humerus fractures, in which the fracture is reduced in the joint, the physiotherapist does not include the fracture resting on the broken hand in physiotherapy.
After removal of immobilization and until complete rehabilitation, the physical therapy exercises for humeral fractures and surgical humeral neck fractures are almost identical. The subtleties of the differences can only be understood by specialists. In the first phase of rehabilitation, the patient's arm can be fixed with a bandage. The injured limb is bent to the side. Then the injured arm is freed from the bandage with the help of the healthy arm and moved to the side.
Immediately after immobilizing the fracture of the humerus, the following exercises can be performed:
- Perform arm swings (rock back and forth);
- Make a fist and relax your fingers;
- flexion of the elbow;
- Abduction of the elbow;
- Perform forward bend with shoulders raised;
- Make circular movements with your arms.
Therapy of humerus fractures in the second phase
The second phase of functional recovery lasts 3-6 weeks. This is confirmed on x-rays at Yusupov Hospital by the formation of bone marrow at the fracture site. The goal of rehabilitation in the second phase is to restore the previous range of passive and active movements. The range of exercises is expanded, but the starting position remains the same. The patient is offered the following series of exercises:
- Extend the upper limbs forward so that they are parallel to the ground;
- Extend your arms to the sides from the starting position;
- Raise your arms to horizontal;
- Lower your arms horizontally and support them with your other hand;
- Bring your fingers together and perform an arm swing up and down.
- Swing your arms from side to side until they are horizontal.
The patient can move both arms bent at the elbow to the side, move the elbows in a circular motion and move the elbows backwards. From a standing position, with arms thrown back and forth, forward and backward swings are carried out. Swings along the body should be performed with the arms bent. Rotation of the upper limbs around the longitudinal axis.
Water applications are particularly useful at this time. Rehabilitation therapists recommend that the patient in the pelvis perform various movements of the limbs, chest and freestyle exercises, as well as crossing the arms in front of the chest and pulling the arms back. Staying in the water puts additional strain on the muscles and is painless at the same time. Training in water improves blood circulation and increases the effectiveness of training.
Subacromial space
It is a space bounded externally by the deep surface of the deltoid muscle, internally by the acromioclavicular joint, above and in front by the lower part of the acromion and the craniocervical ligament, and below by the external surface of the supraspinatus tendon. The subscapularis space is completely occupied by synovial tissue, and there is slippage between the inferior bony surface of the acromion and the supraspinatus tendon. In the subargrade capsule (bursa), calcium salts are deposited in the tendons and muscles of the shoulder girdle. The subscapularis, together with the subscapularis capsule, forms a gliding space located near the base of the club ligament of the shoulder.
Prolonged immobilization of the shoulder, elbow or trunk after an injury or operation has a detrimental effect: the gliding space of the infraspinatus cannot play its role in movement.
At the level of the anterior subacromial space, there is a potential mechanical conflict between the superior tendon of the shoulder rotation muscle and the cranioclavicular arch. This conflict occurs when the shoulder is elevated laterally between 90˚ – 120˚.
Scapulothoracic joint
The acromioclavicular joint is a false joint; it has no cartilage. It is composed of two sliding planes. The movements can be carried out completely and in all levels.
The musculotendinous elements of the rotator muscle of the shoulder and the subclavian space are covered by a superficial muscular layer, which consists of three fibers of the deltoid, namely the anterior, middle and posterior, which insert, respectively, at the level of the clavicle, the acromion and the axis of the scapula and in a common tendon, which is a V-shaped deltoid muscle on the outside of the shoulder.
The trapezius muscle forms a true inclusion aponeurosis with the deltoid muscle at the upper and anterior level of the clavicobrachial joint, which can tear in the shoulder joint.
AXIAL VIEW OF THE SHOULDER JOINT
Purpose of the image. The purpose of the recording is to display the shoulder joint in a plane that is perpendicular to the frontal plane in which direct rear projection images are taken. The axial view makes it possible to determine the direction of displacement of the humeral head in dislocated shoulder joints and the nature of fragment displacement in proximal humeral fractures.
Positioning the patient for imaging. Two options are suggested: 1. The patient sits on the edge of the table. The arm is moved laterally as far as possible into the horizontal plane, bent at the elbow joint, in the pronation position (wrist pointing downwards) and placed on the table or on a stand (Fig. 315). The 18X24 cm cassette is placed on the table level below the shoulder joint and the patient supports himself on it with his armpits. The X-ray beam is directed obliquely onto the projection of the clavicle joint perpendicular to the cassette. 2.
.png)
The patient lies on his back. The arm is stretched as far as possible in the horizontal plane, with an extension of 40-50° being sufficient. The head is turned to the opposite side. The 18X24 cm cassette is placed at the shoulder with its longer edge perpendicular to the plane of the table, with the shorter edge of the cassette resting on the patient's neck. The X-ray beam is directed horizontally at the center of the armpit and perpendicular to the cassette (Fig. 316).
The same positioning is done when the patient is in an upright position (Fig. 317). The cassette can be moved slightly backwards, which is not possible in the horizontal position of the patient, and the center of the cassette is aligned with the humeral head.
The picture is revealing. The image shows the humeral head, the edges of the glenoid socket and the coracoid and club processes.
The edges are the lesser tuberosity of the humerus, the anterior surface of the humeral diaphysis and the posterior surface of the forearm diaphysis (Fig. 318, 319).
X-RAYS OF THE SHOULDER SHOULD BE TAKEN IN DIRECT BACK PROJECTION.
Image mapping. This position is used in trauma cases to determine the type and condition of the fracture, but also to visualize the structure of the humerus in various diseases (arthrosis, tumors, etc.).
Positioning the patient for the x-ray. The patient sits sideways on the table.
The outstretched arm lies on the table or on supports. The hand is in supination position (palm up). The axis of the arm is parallel to the plane of the table. A cassette measuring 18X24 or 24X30 cm is placed under the arm, depending on the patient's height.
The edge of the cassette is in the armpit. The X-ray beam is directed vertically at the center of the cassette (Fig. 324).
.png)
An image in this projection can also be recorded with the patient in the horizontal supine position. The arm is extended along the torso, the hand is in a supinating position. The position of the cassette and the orientation of the X-ray beam are identical.
Value of the image information. A posterior shoulder x-ray shows the medial and lateral borders of the humerus. The lateral edge is rough and sometimes has a bulge at the insertion site of the deltoid.
The medial margin is smooth. The medullary cavity and the cortical substance are well differentiated in the diaphysis (Figs. 325, 326).
.png)
The distal metaphysis of the humerus has a special structure; Here the bone bars form arcuate, concave downward curves. The image should include the distal metaphysis of the humerus so that the proximal and distal ends as well as the medial and lateral surfaces of the imaged humerus can be identified.
Deltoid muscle
The deltoid muscle has a triangular shape with a downward-pointing tip. This muscle consists of three bundles, each of which is responsible for moving the arm in different directions. There are three parts of the deltoid: the clavicle muscle, the acromion muscle and the scapula muscle. Starting from a broad tendon above the shoulder joint, the three bundles of the deltoid muscle converge to form a single tendon that attaches to the humerus. Good deltoid development affects the width of the shoulders, although their bony skeleton can be quite fragile. All three parts of the deltoid can contract independently

Front bundle The front bundle attaches to the collarbone and lifts the shoulder forward (arm flexion), lateral bundle (lateral) bundle attaches to the shoulder roof (acromion) of the shoulder blade and lifts the arm laterally (arm extension). Posterior bundle (posterior bundle) of the deltoid attaches to the shoulder blade and pulls the arm backwards (shoulder extension).

shoulder rotator cuff
The rotator cuff is a group of four muscles that form a protective cover around the shoulder joint. Although these muscles are not very visible, they are very important for shoulder stability and strength. All four muscles begin at the shoulder blade and attach to the humerus bone by running around the shoulder joint.

The muscles of the trunk (the The humerus muscle is largely covered by the trapezius muscle, but since it is quite thin in this area, it does not completely cover the outline of the supraspinatus muscle. The biceps brachii (Epiceps) muscle is located in the suprascapular fossa of the shoulder blade, attaches to the large humerus and is responsible for the external movements of the upper limbs.

The subscapularis muscle (lower soleus) begins on the posterior surface of the shoulder blade and attaches to the humerus. Small circular muscle The small circular muscle is a synergist of the scapula deltoid and the scapularis muscles. The subscapularis and small circular muscles are located behind the joint. They lift the shoulder to the side and pull it back, externally rotating the shoulder (supination).
Subdorsal muscle Expansive, thick, triangular shaped. It takes up almost the entire costal surface of the scapula. It is located in front of the joint and rotates the shoulder inward (pronation) while bringing the shoulder closer to the torso.
rotation
Rotation is another type of movement; it means 'turning'. It occurs not only in the limbs of the human body, but also in some of its components, such as: B. the vertebrae. Pronation and supination can be considered partial rotation. The range of motion of the upper and lower limbs is very different, this is important to keep in mind.
The rotator muscles (pronators and supinators) are small, they are not taken into account when building overall muscle mass. But they need to be taught to athletes, and coaches need to explain to beginners the importance of antagonists in building body composition.
Application in bodybuilding
The use of pronation and supination is very popular in bodybuilding, for example it is important when lifting dumbbells. When working with free weights, the athlete can use different muscle groups. The pronators and supinators should be stressed evenly. Visually speaking, these are the muscles of the forearm and lower leg. If this is not the case, the bodybuilder will spread his arms when walking and the legs will be ridiculously 'thrown out'.
The pronators and supinators of the arms act as antagonists and can both ruin and improve posture. That's why a bodybuilder needs to tense both the chest muscles and the back muscles. Sometimes an athlete's shoulders are hunched forward, indicating that the rhomboid and soleus muscles are tense, while the pectoralis major muscle is severely tense. This can lead to numbness in the fingers and pain at the attachment points of the pectoralis major muscle.
Read more:- pronation and supination.
- Pronation and supination in anatomy.
- What is pronation and supination?.
- shoulder supinators.
- These are the pronator muscles.
- pronation.
- How to determine the type of pronation.
- Pronation of the shoulders - what is it?.
