These injuries are usually combined with leg fractures and ligament injuries.
- Fracture of the posterior calcaneal process. Tibial myopathosis in dancers
- symptoms of the disease
- Physical overexertion
- Injury
- SYMPTOMS
- DIAGNOSIS OF POSTERIOR IMMPINGEMENT
- Symptoms of a foot fracture (navicular bone)
- Symptoms of a metatarsal fracture
- Lisfranc joint dislocation
- synovitis
- Loose bodies in the ankle joint
- Stages of aseptic necrosis
- diagnosis
- What is the prognosis?
- Sign 8 – 'Bleeding from the surface of the nevus'.
- Sign 9 – 'Hair loss on the surface of the nevus'.
- contraindications
- How is the investigation carried out?
Fracture of the posterior calcaneal process. Tibial myopathosis in dancers
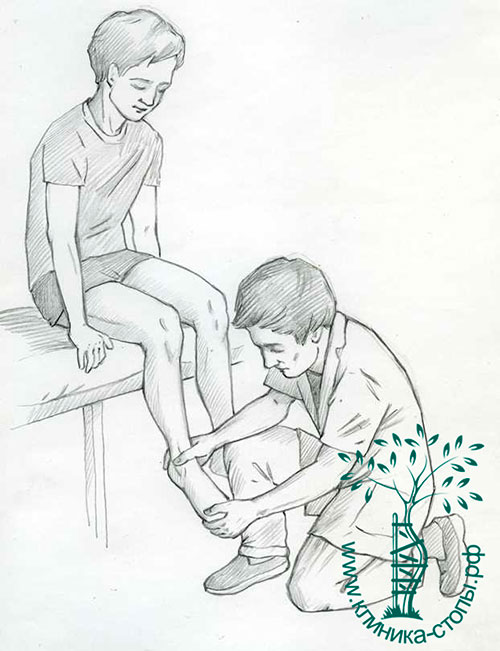
The fracture of the posterior talar process occurs more often in athletes and ballet dancers during a variety of movements with non-physiological foot position and high physical stress when the posterior talar process contacts the posterior edge of the tibia. This process is permanently traumatized, relocated and sometimes detached. There is pain when placing the foot on the toes, a feeling of locking in the ankle joint, and pain on palpation on the posterior surface of the ankle joint in front of the heel tendon.
Further observation of the ballet dancers reveals ankle locks and intermittent pain, which limits the ability to work and improve performance. X-ray examination shows that the posterior process is separated from the talus. An x-ray of the healthy leg should also be taken to differentiate the tear from the complementary talar bone, which is usually symmetrical on both the affected and healthy leg.
Treatment of a torn posterior process of the talus in ballet dancers is purely surgical – removal of the torn fragment. This prevents the development of deforming osteoarthritis of the ankle and allows the ballet dancer to quickly return to the stage without compromising her professional abilities.
Due to the high and irrational load on the lower leg muscles during dance, ballet dancers often experience painful muscle problems. All of these muscle changes and diseases are called myopathoses.
A distinction must be made between simple focal myopathosis, fascial focal myopathosis and infectious myopathosis.
Simple focal myopathosis is a disorder of coordination between antagonistic and synergistic muscles in general. It manifests itself as a temporary muscle spasm, which quickly passes under the influence of overwork, negative emotions, poor organization of work processes, lack of warm-up before a performance and cooling down. Myopathosis occurs particularly often during the first performance because there is great excitement about the result of a new game. This leads to a certain fidgetiness, the movements are still carried out insecurely due to a strong stereotype that has not yet been developed.
symptoms of the disease
The following symptoms may indicate a heel bone fracture:
- Pain in the back of the foot.
- Limited mobility of the foot. The movement is accompanied by increased pain, and the patient has difficulty stepping on the foot.
- Swelling of the tissue. The greater the injury to the blood vessels, the greater the swelling and possibly a bruise with a bluish tint to the skin.
- In an open fracture, there is a wound in the foot and bone fragments may be visible.
- The fracture is often combined with joint dislocations and fractures of other bones of the foot.
- When inflammation occurs, there is a temperature reaction, increased local pain, and a throbbing character.
The most common cause of the disease is trauma to the foot. The mechanism of injury is a sprain or impact on the sole. Often, such injuries occur to drivers during an accident, especially motorcyclists, due to the foot resting on the pedal. But also when falling in icy areas.
Physical overexertion
Ankle-hindfoot syndrome, caused by strenuous physical exertion, occurs primarily in ballet dancers and runners. The forced flexion of the sole of the foot, e.g. B. when running on an incline, leads to constant compression of the rear ankle joint; the same flexion seen in ballet positions such as 'en pointe' and 'demi-pointe' causes compression of the posterior ankle joint.

In both cases, the anatomical formations between the heel bone and the posterior surface of the tibia may be subjected to excessive pressure. With regular exercise, mobility and range of motion gradually increase and the distance between the heel bone and the back edge of the shinbone decreases.
This creates the conditions for compression of normal but also pathological anatomical structures that can be located in this area: os trigonum, hypertrophied posterior process of the talus, thickened posterior joint capsule of the ankle joint, scar tissue or calcification of the joint capsule after trauma, loose joint bodies in the posterior area of the ankle joint or osteophytes at the posterior edge of the tibia.
Injury
Forced flexion of the soleus causes compression between the tibia and heel of the posterior process of the talus. If this compression is strong enough, it can cause a fracture. Compression of the posterior capsule of the ankle joint can lead to its thickening and calcification.
In such cases, post-traumatic calcifications can usually also be found in the back part of the joint. Excessive flexion of the sole can occur in car or motorcycle accidents or in certain sports such as soccer.
SYMPTOMS
Posterior ankle impingement syndrome is a pain syndrome. The pain is limited to the back of the ankle. It usually occurs when the foot is flexed rapidly. In some patients, rapid dorsiflexion is also painful. This is because this position places tension on the ankle capsule and ligaments of the ankle, which are attached to the posterior humerus.
DIAGNOSIS OF POSTERIOR IMMPINGEMENT
The diagnosis is based on the medical history, direct medical examination and radiological findings.
During the examination, pain is usually noted when palpating the posterior part of the talus.
Also, a series of special provocation tests are carried out, during which rapid plantar flexion of the ankle joint is performed in different positions of the foot. If the tests are positive and there is pain on palpation, a diagnostic joint block with a local anesthetic solution may be indicated.
Symptoms of a foot fracture (navicular bone)
It can be caused by violent trauma from a severe foreign body or from compression. Less commonly, an indirect injury occurs due to active, excessive flexion of the sole of the foot. These fractures usually occur in combination with injuries to the elbow, and possibly also with a fracture of the sphenoid bone. The fracture of the navicular bone begins to move inward and backward. There will be slight swelling and pain. Walking is painful for the injured person, but the injury does not limit movement. Symptoms include palpable protrusion – a displacement of the fragment at the site of injury – and a typical preference for walking only on the heel. The diagnosis is clarified by a radiological examination.
The symptoms of this type of foot fracture are difficult to diagnose and are similar to an injury to the navicular bone. The difference may be that the pain occurs on the outside of the foot with a navicular bone injury and on the inside of the foot with a sphenoid bone fracture. In addition, it is necessary to distinguish between a sesamoid fracture and visually visible fragments of the cuboid and sphenoid on the x-ray.
Symptoms of a metatarsal fracture
This is the most common fracture of the foot, with the 1st and 4th. Multifractures, that is, injuries to all metatarsal bones, can be diagnosed in the event of direct trauma (car accident, fall with a heavy object). Symptoms of a foot fracture depend on the severity of the injury and include numerous swelling, severe pain, and inability to walk. X-rays are taken from two sides - oblique pronation at 50° and dorsiflexion and plantar flexion.
As with a metatarsal fracture, the phalanges of the toes are damaged in a straight line. The proximal phalanges break most often, the distal phalanges break less often. The rarest case is a fracture of the metatarsal bone of the foot. The symptoms of a broken foot are typical of small fractures, the pain is tolerable and swelling is minimal. The diagnosis is confirmed by an x-ray.
The symptoms of a foot fracture are very diverse and can be differentiated through a thorough examination by a surgeon, an X-ray examination and, of course, timely consultation with a doctor.
Lisfranc joint dislocation
Caused by a fall from a great height or by strong pressure, e.g. B. by being trapped with a wheel.
The most common dislocations are dorsal and lateral, slightly less often plantar or medial.
Lisfranc joint dislocations can be complete, where all bones are affected, or isolated. However, in this case they are often associated with fractures.
During the treatment, the foot is fixed and a strong forefoot pull is carried out.
The bones are then aligned manually. Sometimes a wire is inserted for comfort, and in complicated cases an Ilizarov brace or arthrodesis is performed.
synovitis
Synovitis is an inflammation of the soft tissues that line the ankle joint (synovitis), which is often manifested by pain, swelling and restricted movement. It can occur as a result of acute trauma, arthritis (rheumatoid arthritis), overuse or osteoarthritis.
If conservative treatment does not relieve the symptoms, the inflamed joint mucosa is surgically removed using arthroscopy.

Loose bodies in the ankle joint
Articular cartilage or scar tissue caused by an injury to the ankle joint can become detached in the joint capsule. In this case one speaks of loose bodies or loosening. They can also occur in the so-called synovial chondromatosis, when the joint lining detaches for unknown reasons. This loosening can cause cracking and locking of the joint, accompanied by pain, swelling and restricted movement.
Loose bodies are identified with X-rays or CT scans and sometimes just MRI.
Arthroscopy of the ankle joint is used to find and remove the loose body.
Stages of aseptic necrosis
The following stages are distinguished, which are characterized by rapid progression and a high degree of severity of the disease:
- Stage 1 – minor changes in bone structure;
- Stage 2 – small cracks appear in the bone head;
- Stage 3 – the cartilage atrophies and the hip socket is affected;
- Stage 4 – active necrotic process.
In the initial stages, practically no changes are visible. There is just a gradual increase in pain. If treatment is delayed, major surgery may be necessary.
diagnosis
If such a pathology is suspected, an X-ray or CT scan is ordered, sometimes an MRI. While the first option may not reveal the problem, a three-dimensional image makes it easier for the orthopedist to identify the problem.
Such pathologies are treated using conservative and surgical methods. The former are aimed more at slowing down the destructive processes and reducing pain sensations.
- Conservative treatment includes taking non-steroidal anti-inflammatory drugs, special physiotherapy and physical therapy, and the use of orthoses.
- Surgical treatment – varies depending on the situation. Chondroplasty (replacing part of the thigh bone or an artificial implant) or tunneling the damaged area (drilling a hole) may be performed.
- In particularly advanced cases, the ankle bone is removed. After the operation, a full rehabilitation period of approximately six months is required.
There is also a special diet for aseptic necrosis. No artificial oils should be consumed and it is advisable to avoid egg yolks and fatty meats. Foods containing omega-3 acids, magnesium, phosphorus and calcium should be included in the diet.
What is the prognosis?
If osteosclerosis of the hip bone or other parts of the body is accompanied by congenital anomalies of the musculoskeletal system, regular prophylaxis is necessary to lead a normal life. In the early stages of discovery, the prognosis for a favorable outcome is high. If the disease remains untreated for a long time, it can lead to disability and therefore premature death.
Osteosclerosis can be prevented through a healthy diet and weight control. An appropriate sleep and wake cycle is important. Increased physical activity and the wearing of special orthoses and bandages are required. If an inflammatory reaction or infection develops, it is important to see a doctor in a timely manner and receive treatment.
Sign 8 – 'Bleeding from the surface of the nevus'.
Yes, in fact one of the most common features of melanoma is spontaneous bleeding without prior trauma to the nevus. This alone would cause any oncologist to seriously question the benignity of the nevus.

However, in my practice I came across a rather rare type of skin cancer - pyogenetic granuloma. These formations appear very quickly and bleed, but are 100 % benign:

Sign 9 – 'Hair loss on the surface of the nevus'.
This may indicate that the nevus has become malignant. If the mole is 5 mm or larger and several hairs have disappeared from its surface at the same time and are unlikely to reappear. If the same mole has begun to grow and has increased in size twice within two months, these are already two warning signs at once, and such a mole should be immediately examined by an oncologist.
I should also point out that in my experience. once I saw a melanoma whose surface was covered with hair.

However, there are many moles that do not have a hairy surface and are completely benign. Many people also panic when a single hair grows out of a mole and suddenly falls out. Please don't despair - it should appear again in 2-3 weeks at the latest.

I wrote this article about birthmark hair
contraindications
There are no absolute contraindications to digital radiography.
- Pregnancy – exposure to radiation can have adverse effects on the developing child.
- Situation in which the patient requires urgent treatment.
- Severe agitation or mental illness that makes it impossible to remain calm while using the X-ray machine.
- Age under 14 years.
In these cases, the doctor decides whether an X-ray examination is necessary. He may prescribe another diagnostic method or perform the X-ray with additional precautions. To minimize the learning effect, a lead apron is used that covers the genital area for adults and the entire body for children.
How is the investigation carried out?
No preparation is required for an ankle x-ray. As a rule, an X-ray of the ankle joint is taken in two projections: straight and lateral. The straight x-ray is taken with or without rotation of the foot. The picture shows the tibia, ankle, talus and ankle. In the lateral projection, the patient lies on his side with the healthy leg bent at the knee and drawn toward his stomach. The pictures show the shinbone, the ankle joint, the ankle bone, the heel bone and the ankle joint. In some cases, the doctor recommends taking a power flexion x-ray to assess the condition of the ligaments. If necessary, the examination is carried out under local anesthesia.
The evaluation is carried out by comparing the recording with a normal reference recording. Size, shape, bone structure, height and arch angle as well as other criteria are determined.
Normal results or detected abnormalities are recorded in a report, which serves as the basis for a final diagnosis.
You can apply by selecting a department in your city
Read more:- Anatomy of the heel bone x-ray.
- back foot.
- What is the part of the leg below the thigh called?.
- tibia and fibula.
- Structure of the human ankle.
- The lateral ankle is.
- Photo of the ankle.
- The ankle bruise is where the picture is taken.
