Bukhar State Medical Institute named after Abu Ali ibn Sino. Abu Ali ibn Sino, Bukhara, Uzbekistan
- Osteosynthesis of the tibia
- Benefits of Tibial Osteosynthesis Surgery
- The topicality of the problem
- Material and methods.
- Prevention of complications depending on the degree of amputation (disarticulation) of the lower limbs
- keywords
- COMMON APPROACHES TO SELECTION OF LIMBS SHORTENING LEVEL
- Methods of treatment for obliteration of atherosclerosis of the arteries of the lower limbs:
- Conservative treatment
- Surgical treatment of atherosclerosis of the lower arteries, vessels
- Reconstructive surgery:
- Symptomatic interventions:
- Indications and contraindications for amputation of the lower limbs
- Classification of lower limb amputation
- To be accepted into our practice you need:
- Frequently asked Questions.
- 'Make your feet young again your feet.'
- Frequently Asked Questions
- useful information
- Anesthesia in bunion surgery
- How to properly take a stress x-ray of the foot
- How you can benefit from a personal consultation with me
- indications
- advantages and disadvantages
- Slide 14Using a Yusevich plaster splint allows:
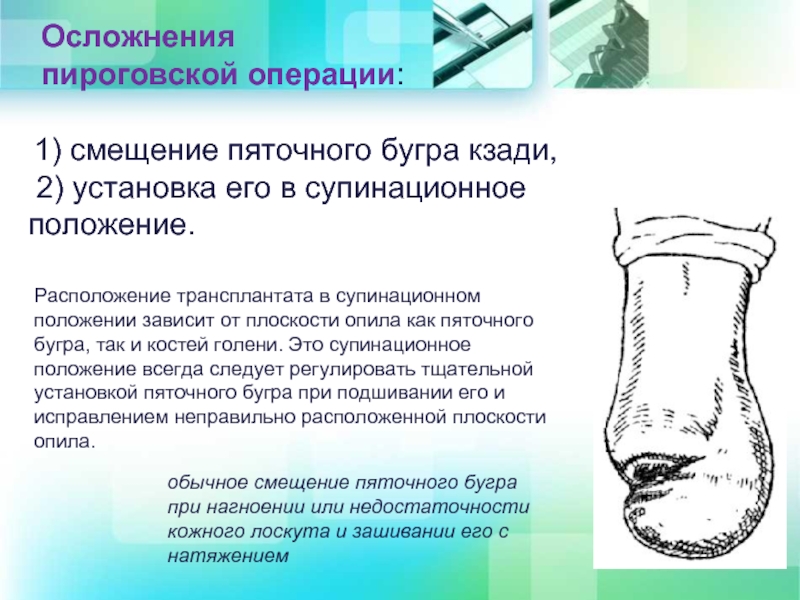
- Slide 15 1) Posterior displacement of the calcaneal bone, 2) Posterior positioning of the calcaneal tuberosity.
Osteosynthesis of the tibia
Osteosynthesis of the lower leg bone is a surgical procedure performed to reduce (return to place) and reliably fix bone fragments resulting from trauma to the tibia or fibula. The main goal of the procedure is to optimize the physiological conditions for the bones to grow together in their correct anatomical position. Such a radical intervention as tibial osteosynthesis is not recommended for all patients with fractures, but only for those for whom conservative measures have failed or are inadvisable due to the diagnostic findings (inability to perform anastomosis in a plaster cast).
Surgeons can use skeletal structures or use only single fixation options to fuse bone fragments as correctly as possible. The choice of specific devices depends on the size of the injury, the type of injury and location of the fracture, age, and additional medical conditions.

Benefits of Tibial Osteosynthesis Surgery
The main advantage of such an intervention is that it creates the conditions for the fastest possible complete healing of a fracture of the tibia. This is possible because two conditions are met. The first is that all bone fragments are fixed firmly and precisely. The second is the early restoration of tissue function with improved blood supply and accelerated regeneration. Through the use of various constructions, the bones are firmly connected to each other and the mobility of the limb is maintained.
These operations are performed for complicated fractures when both bones are damaged at the same time. In addition, osteosynthesis of the left or right tibia may be recommended if the ankle joint area is affected, if the fractures are displaced and the surrounding tissues are damaged.
The topicality of the problem
Unfortunately, in recent decades, the number of diabetic foot syndrome patients with symptoms of critical lower limb ischemia (CLIN) has increased [1-3]. The development of critical ischemia is a sign of complete circulatory decompensation, which occurs in 30-42 % of patients with severe diabetic foot syndrome (DM) [3-5]. The predicted mortality rate in AS patients with CINC increases from 25 % during the initial development of AS to 60-70 % [6-8]. The incidence of high amputations due to SDS in developed countries is between 0.06 and 3.86 cases per 10,000 diabetics [9-12].
To date, reconstructive surgery is the only effective treatment for SDS patients with CINCs. However, in practice, revascularization of the arterial bed of the lower limbs is only possible in 35-50 % of patients. This is due to the questionable success of isolated surgical revascularization in patients with multilevel type and predominantly distal location of arterial involvement (3, 6, 9, 13-17). At the same time, operations that enable the preservation of the knee joint (lower leg amputations) are welcomed, which significantly improves the quality of life of patients in the postoperative phase [5, 9, 12]. The use of less traumatic operations at the tibial level in AS with CINC is an urgent problem in modern operative surgery.
The aim of the study. – To evaluate the effectiveness of an improved lower leg amputation technique for diabetic foot syndrome with critical lower extremity ischemia.
Material and methods.
We analyzed the outcomes of lower limb amputations in 82 patients with AS and CINC treated in the Bariatric Surgery Department of Bukhara Regional Multi-Speciality Medical Center between 2007 and 2019. 54 (65.8 %) of the patients were men and 28 (24.2 %) were women. The age of the patients ranged from 38 to 85 years. Most patients had significant impairment of physical functions.
All patients were divided into two groups according to the surgical technique on the lower leg: 1. the (control) group consisted of 40 patients who underwent myoplastic amputation of the lower limb according to the Mitish-Svetukhin method; 2. the (main) group consisted of 42 patients who underwent myoplastic amputation of the lower extremity using the improved (technically simplified) method.
The indications for amputation were: occlusion of the main arteries of the lower extremity with decompensation of lateral blood flow and extensive purulent-necrotic process in the foot, extensive wet gangrene extending to the lower third of the tibia, complete dry gangrene of the foot, presence of anaerobic infection (clostridial or non-clostridial), critical ischemia of the lower limbs not medically correctable, spread of the local purulent-necrotic process on the foot beyond the two anatomical areas with signs of the development of systemic inflammatory syndrome (SIRS).
The publications highlight the results of a new method of surgical intervention (Myoplastic amputation according to Mitish-Svetukhin) at the tibial level in SDS with CINC. This amputation method (applied to a control group of patients) leads to a dramatic reduction in the frequency of postoperative complications in the area of the amputated stump and creates favorable conditions for prosthetics (the knee joint is preserved). However, the technical execution of this operation is time-consuming (the lambdoid muscle is cut in order to then extrude into the tunnel created between the tibia and the posterior musculo-fascial flap). The long duration of surgery for severe CINC is associated with the risk of infection of the surgical site and the development of purulent complications. For this reason, attempts have been made to improve the operation method to eliminate the above-mentioned inconveniences.
Prevention of complications depending on the degree of amputation (disarticulation) of the lower limbs
In the second half of the last century, the level of stump care was standardized, with the principle of achieving the greatest possible functionality of the stump prosthesis system. Modern developments in surgical techniques and in prosthetic and orthopedic equipment have made the previously developed schemes obsolete. However, the most typical complications and the resulting limitation of prosthesis functionality can still be observed today. This article presents the possible variants of complications associated with the degree of stump shortening, the ways to prevent and eliminate them, as well as an overall assessment of the impact of stump length on statodynamic function at different levels.
keywords
Introduction. The restoration of the function of the upper and lower limbs in post-amputation defects from an orthopedic perspective (for the upper limb - maximum functionality, for the lower limb - maximum possible support and locomotion) is still a current topic today. From the point of view of the support ability of the stump, the resistance of the stump to unnatural loads, the range of motion of the joints, the strength of the individual muscle groups of the stump, the strength, control and muscular endurance of the entire prosthetic stump, the neighboring stump and the trunk, the degree depends the reproduction of the biomechanics of the prosthetic gait depends entirely on the length of the shortened segment [1, 2]. However, there are difficulties with amputations of the lower limbs: When resecting individual 'problematic' levels, a number of conditions must be met in order to achieve success. Otherwise, the likelihood of a poor-functioning, 'non-functional' stump and thus multiple/repeated surgical interventions is high [1, 3].
COMMON APPROACHES TO SELECTION OF LIMBS SHORTENING LEVEL
The unification of the procedure for selecting the level of amputation began in the 19th century. Previously, the amount of limb shortening was determined solely by the tissue change. The 'amputation level' refers to the length of the bone segment to be shortened. Various proposals have emerged at different times in the medical community to facilitate subsequent prosthesis and the use of a prosthesis depending on the level of limb shortening [4].
Currently, all amputation schemes proposed to date are considered irrelevant and should not be used in practice. However, there are still 2 main directions in recommending amputation heights:
- Given modern surgical and prosthetic possibilities, the choice of amputation height (disarticulation) must follow the principle established by NI Pirogov: 'Amputation as low as possible';
- The choice of amputation level should be as favorable as possible for early prosthetics.
Methods of treatment for obliteration of atherosclerosis of the arteries of the lower limbs:
Conservative treatment
In the early stages of obliterating atherosclerosis of the arteries of the lower limbs, conservative treatment is indicated, which must be comprehensive; all unfavorable factors causing vasospasm must be excluded. The prerequisite for successful treatment is quitting smoking (!). Physical activity is of great importance. Patients with intermittent claudication should walk for 30-45 minutes daily - this promotes the development of small arteries, leads to an increase in muscle strength and increases the distance covered without pain.
If pain and tension occur in the leg muscles, the patient should stop and resume walking once these sensations subside. Cycling or swimming is often much better tolerated than walking (but does not replace it). High blood pressure, cholesterol and blood sugar in diabetics are corrected. Medications are used to reduce the tension of small blood vessels, increase the elasticity of red blood cells, and prevent blood clots from forming in the blood vessels. Physiotherapeutic and balneological treatments as well as hyperbaric oxygen supply are also used.
Surgical treatment of atherosclerosis of the lower arteries, vessels
Reconstructive surgery:
- Endovascular treatment methods using X-rays. Under X-ray control, we can use special long, thin instruments to reach the affected vessel (vascular segment) in the lower extremities via a small puncture in the femoral artery (rarely also other arteries). Modern technical possibilities allow us to expand the section of the vessel from the inside with a special balloon and, if necessary, to insert a thin metal framework (stent) to prevent renewed stenosis.

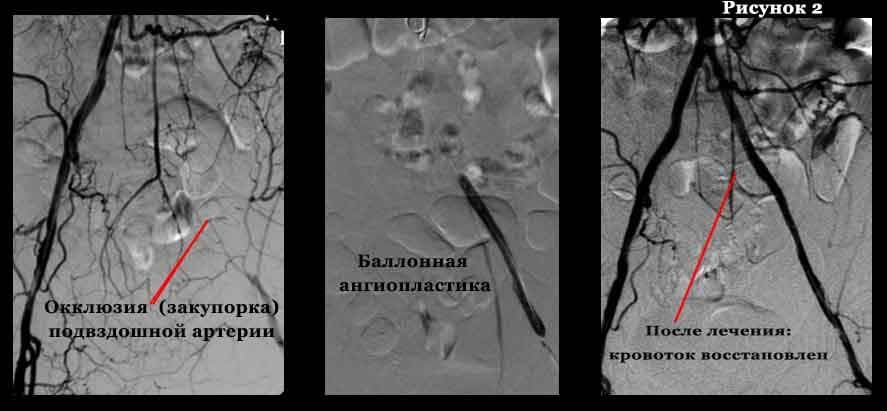
- Open surgical procedures. In patients with a vascular occlusion of no more than 7-9 cm, the inner modified layer of the artery with atherosclerotic plaques and blood clots is removed (endarterectomy). If the occlusion is more extensive and there are significant calcium deposits in the artery wall, a bypass (shunt) or resection of a section of the artery and replacement with a plastic prosthesis or a biomaterial (prosthesis) is indicated.
Symptomatic interventions:
- Sympathectomy (Sectioning the plexus of nerves responsible for the contraction (narrowing) of the arteries) is carried out in the case of recurrent artery occlusions and as an adjunct to reconstructive surgery. This procedure improves blood flow to the limbs by dilating small arteries.
- Revascularization osteotomy is also a complementary procedure that improves blood circulation by stimulating the formation of new small vessels in the lower limbs after bone damage.
- Arterialization of the venous bed is rarely used today because it is technically demanding and the long-term results are not as good as with the techniques described above.
Please apply online and we will contact you as soon as possible to answer any questions.
Indications and contraindications for amputation of the lower limbs
Serious traumatic injuries related to:
- tearing of the leg and crushing of the bony structures;
- damage to a large blood vessel;
- Bruising or severe damage to soft tissues without the ability to repair their integrity.
- Damage to a peripheral artery with development of severe ischemia;
- Atherosclerotic lesion.
- Extensive infectious lesions;
- Malignant neoplasm of malignant etiology;
- Deep frostbite and burns characterized by deep necrosis.
If a patient comes to the hospital in a state of post-traumatic shock, they should not undergo surgery. He must be brought out of this state before any intervention can be carried out. The time for appropriate manipulation is limited to four hours.
Classification of lower limb amputation
There are three types of amputations, depending on the reasons and circumstances in which they are performed:
- Primary amputation – performed for the first time because the leg has lost its vitality;
- Secondary amputation – performed for the first time due to ineffective treatment or the occurrence of serious complications;
- Reamputation – performed after a first, second or third amputation due to failure or poor condition of the limb.
Depending on the extent of the amputation, the following degrees of amputation are distinguished:
- Amputation of the fingers of the lower limbs.. It is indicated in cases of trophic ulcers and its timing allows the remainder of the limb to be saved. The surgeon cuts along the joint line at the junction of the phalanx with the foot;
- Amputation of the foot. If the gangrene lesion affects the entire foot, it is removed in its entirety, usually using the Sharpe method. The surgeon makes an incision along the metatarsal bone and separates the soft tissues using the two-flap method;
- Amputation of the tibia of the lower extremity. If the disease has progressed to the point where the shinbone is affected or there is a severe circulatory disorder, it is removed. During the operation, the surgeon applies fascia and skin flaps;
- Amputation of the lower limbs at the thigh. If severe shin damage or a severe circulatory disorder is diagnosed, the lower extremity is separated from the thigh. Using the Gritti-Albrecht technique, the surgeon creates a non-functional stump.
To be accepted into our practice you need:
- An initial consultation, for which you can make an appointment, or you can send photos and recordings of your feet by post to [email protected].
- If you have decided to undergo surgery, you can immediately make an appointment, ask your questions and make an appointment by calling +7-926-961-71-96.
- The next step is a comprehensive preoperative examination. You can have all the necessary examinations and tests carried out in our clinic within a few hours or bring everything you need with you to the practice.
- On the agreed day you will come to the clinic for your procedure. The receptionist welcomes you, completes all the formalities, introduces you to the clinic and you go to your room. There will then be a discussion with the surgeon and the anesthesiologist. On the day of the procedure you should not eat anything and drink only a little water. It is advisable to remove any nail jewelry such as nail polish, rhinestones, etc. and perform thorough foot skin hygiene.
- After the operation, you will be looked after by an anesthesiologist for a short time and then return to your room.
- Depending on the extent of the surgery, you will need to stay in the hospital between 1 and 4 days to apply bandages and receive appropriate pain management. You may walk in special shoes for the first 24 hours after surgery.
You can be observed and treated in our clinic or at another clinic that may be more conveniently located. Equally important are the removal of the stitches 14 days after the operation and x-rays 6 weeks after the operation. From the 3rd week onwards, physiotherapy is carried out to develop the range of motion of the operated fingers and physiotherapy to reduce pain and swelling.
Frequently asked Questions.
Surgery is usually suggested when conservative treatment has failed. If orthopedic shoes and insoles, silicone pads, physiotherapy and therapeutic exercises do not have the desired effect, surgical correction of the deformity should be considered. Conservative measures cannot eliminate bunion and first toe valgus deviation, but they can slow the progression of the deformity and reduce pain.
After a rehabilitation period, high-heeled shoes can be worn occasionally. Permanent surgery is not advisable because it will put too much stress on the forefoot, which will lead to recurrence of the deformity and progression of osteoarthritis of the 1st foot. It is not advisable to operate on the bone for cosmetic reasons because if there is no pain before the operation There may be pain after the operation due to scarring at the surgical site. Wearing high-heeled shoes and narrow-toed shoes increases the risk of the deformity recurring in the future.
'Make your feet young again
Her feet.'
Today there are modern, safe and effective treatments to help you restore the health of your feet. Some of them are completely free, others are very affordable. Unfortunately, many older people don't know this.
Therefore, for the lovely ladies of the older generation, I have launched a new unique campaign called 'Rejuvenate Your Feet'.
I invite you to my practice for a FREE consultation where I will examine your feet.
I will also tell you what modern, safe and effective treatments are available for your situation and how you can get them for free or at the lowest cost. We will talk to you about all the options available and choose the one that suits you best.
1. Any person over the age of 55 is eligible to participate.
2. You can apply with any foot and ankle problem.
3. The campaign runs from August 1st to September 30th, 2019.
4. You can come to the consultation in person in St. Petersburg at Yaroslavsky Prospect 66, Building 1, or get advice online.
Call your mothers, grandmothers, relatives, friends - anyone who can benefit from my counseling. Tell as many people as possible, share on your social networks.
Mature age is a good time to enjoy life. So don't let pain and discomfort in your feet affect your quality of life. Let's get your feet back in shape together so that walking becomes one of your favorite activities again.
If you would like to know more about the Rejuvenate Your Feet campaign, send an SMS to WhatsApp +79219651182
or call us 8 (812) 336-60-22
Frequently Asked Questions
The operation itself is no different. In all the operations I perform, I use state-of-the-art medical equipment, the best imported implants, high-quality consumables, the necessary medications and regional anesthesia (a type of local anesthesia - two injections are given into the foot). There are only two differences in free surgery: 1. If you want to operate on both feet at the same time, you have to carry out the operation on two different days. The other foot can only be operated on after 2 weeks. 2. If you have a quota, you will not receive follow-up care. Aftercare is always included in the price of the operations I pay for. This way I can monitor how you are feeling, how your bone is healing and how your joint has regained mobility. This way I can prevent possible postoperative complications. This always leads to excellent results and satisfied patients. Post-operative care can be purchased separately.
useful information
I will inform you about the treatment process. What you need to pay attention to.
How to get the best result.
How you can make your feet healthy and beautiful again and maintain your quality of life for many years to come.
Anesthesia in bunion surgery
I am often asked two questions: - What anesthesia is used for bunion removal - Can I choose general anesthesia to be unconscious during the operation.
In this video, I give in-depth answers to these two must-watch questions
How to properly take a stress x-ray of the foot
In order to properly assess a forefoot deformity (hallux valgus), a stress x-ray is required, which means the patient must be standing at the time of the image.
We recommend the First Diagnostic Center at Calle Siqueirosa 10.
How you can benefit from a personal consultation with me
I am often asked why it is better to come for a consultation before the operation. Finally, you can send in your scans, chat on social media, and then head straight to the operating table. I have been performing surgeries for 18 years and have noticed a few things
indications
The indications for surgery are traumatic lesions, but also tumors, bone inflammation, tuberculosis, etc.
The Syme operation was already known at the time the method was introduced. Syme ), in which the same skin incisions were made as in the Pyrogov operation. However, in 1852, NI Pirogov suggested closing the saw cut on the amputated tibia with a saw cut on the heel bone. The proposed amputation method was a great discovery of its time, as it became the basis of all bone plastic methods: Gritty, Sabaneev, Weir.
advantages and disadvantages
The biggest disadvantage of the operation is the stress on the Achilles tendon. In addition, the base of the stump is different than that usually assumed, which can lead to skin ulcers.
Nonetheless, Pirogov's operation gave a tremendous boost to the development of bone grafting techniques. Pirogov defines the meaning of a historically significant operation in the following words:
'My operation has nothing to fear from the competition. Their dignity lies not in the method of amputation, but in osteoplasty. An important principle which he proves beyond doubt is that a piece of one bone, in conjunction with the soft tissues, is attached to the other and serves to elongate the penis and render it functional.'
Slide 14Using a Yusevich plaster splint allows:
to achieve adequate fixation of the transplant;
After 48 hours, without disturbing the fixation of the graft;
3) to take a control x-ray of the profile not through the plaster;
4) for a favorable postoperative course without changing the plaster splint, use a circular cast on days 21-25 and put a plug on the end of the stump to avoid shortening.
Dia 15
1) Posterior displacement of the calcaneal bone,
2) Posterior positioning of the calcaneal tuberosity.
Conventional displacement of the calcaneal tuberosity in sclerosis or insufficiency of the skin flap and stretching of the skin flap
The position of the graft in supination depends on the plane of fillet of both the calcaneal tubercle and the tibia. This supination position must always be corrected by carefully positioning the calcaneal tubercle during suturing and correcting the misaligned fillet plane.
- The reamputation is.
- Indications for amputation.
- Life after a leg amputation.
- The toe formation.
- Limb amputation.
- blunt.
- traumatic amputation.
- Metatarsal amputation.
