The anterior cruciate ligament is responsible for the dynamic stability of the knee joint by preventing nonphysiological anterior displacement of the tibia and supporting the external condyles of the tibia. More than half of the knee's stability is provided by the ACL. For this reason, it is called the primary stabilizer of the knee – without it, the joint cannot function properly. It is located in the middle part of the ankle joint and overlaps with the x-shaped posterior cruciate ligament, which is why both structural elements have the same name. The following will specifically address the ACL and its post-traumatic reconstructive and plastic correction.
- Tear of the collateral ligament in the knee
- symptoms
- Anatomical features of the knee joint and ACL
- collateral ligaments
- cruciate ligaments
- Degree of ACL damage
- Symptoms of sprains and tears
- Diagnosis of shoulder ligament injuries
- Possible complications
- Diagnosis of ligament injuries
- General principles of treatment
- Conservative treatment
- AdobeStock_422305936-1.jpg
- Treatment
- Rehabilitation after injury
- Ligamentoplasty
- rehabilitation
- forecast
- Contraindications for surgery
- Rehabilitation after surgery
Tear of the collateral ligament in the knee
Collateral ligament injury is one of the most common knee injuries, occurring more frequently in young, active people as a result of sports or household chores. Collateral ligament tears are caused by short-term but increased loads on the knee joint: jumps, sharp turns, falls, severe bruises, unnatural bending of the limb.
Depending on the extent and location of the damage, a distinction is made between complete and partial tears of the inner and outer collateral ligaments of the knee joint. A complete tear is characterized by a separation of the ligament into two parts or a separation of the tissue from the attachment site. With a partial tear, the fibers tear, which is often confused with a sprain.
Depending on the cause, ligament tears can have the following causes
- Traumatic – when the cause is increased pressure on the joint;
- degenerative – when the damage is caused by changes in the joint structure due to degenerative changes, disease or age-related factors.
symptoms
Damage to the collateral ligaments of the knee joint is accompanied by characteristic symptoms:
- Severe, sudden pain that later occurs even at rest;
- swelling of the soft tissues around the knee, spreading to adjacent areas;
- Local subcutaneous effusions;
- tenderness when touched;
- Difficulty moving the joint.
In some cases, the torn fibers are accompanied by an external deformation of the knee contour, and sometimes a characteristic crunch or click is heard when trying to move.
Anatomical features of the knee joint and ACL
The tibia and femur form the knee joint along with the kneecap, which is located in the front (upper) part of the joint and also serves as a protective element.
The femur and shinbone are connected by four very strong ligaments that stabilize and support the function of the joint.
collateral ligaments
The collateral ligaments are located on the sides of the joint, with the lateral variant of the collateral ligament running on the periphery and the medial variant on the inside of the joint. The primary function of the collateral ligaments is to control lateral movement and prevent pathological changes in the normal position of the bone.
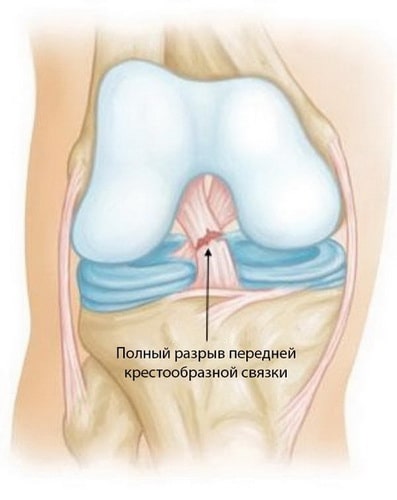
cruciate ligaments
The cruciate ligaments are located at the front and back of the joint and connect them together, preventing the femur and shinbone from moving in different directions.
The anterior cruciate ligament (ACL), which consists of at least two stabilizing bundles, is located diagonally in the middle of the knee joint. One of the bundles is responsible for stabilizing the rotation of the joint, the other for blocking unwanted movements of the hip.

The knee joint is made up of 4 components: ligaments, meniscus, bones and tendons.
Degree of ACL damage
Almost 50 % of ACL injuries are directly related to injuries to other parts of the joint - various ligaments, articular cartilage and meniscus.
It is customary to classify the injuries into the following grades:
- Grade 1 – the mildest form, characterized by a slight displacement of the ligament while maintaining its stabilizing function;
- Grade 2 – with this level of injury, also known as a partial tear, the ligament is severely stretched and loses its stabilizing function;
- Grade 3 – complete rupture of the ligament with separation of the ligament into two fragments and, consequently, loss of stability of the knee joint.
Partial cracks are very rare, while complete cracks are the vast majority.
Symptoms of sprains and tears
The following symptoms are commonly observed with shoulder ligament injuries:
- Shooting pain in the shoulder when the arms are moved up or to the side;
- Swelling in the injured area – usually several hours after the injury;
- Increased temperature in the swollen area;
- bruising and swelling;
- limited mobility in the shoulder.
In the event of an injury, the child may move the joint unnaturally, which is also a symptom of a sprain or torn ligament.
Pain syndrome is the main symptom that occurs immediately after the injury. Over time, the pain may progress to numbness or dizziness.
First aid if a tear or sprain is suspected is to stabilize the injured limb and apply a cold compress. If the pain is severe, a painkiller may be given. Don't forget to take the injured limb to the hospital.
It is not advisable to treat joint ligament injuries yourself - this can be dangerous for the injured arm and lead to negative consequences.
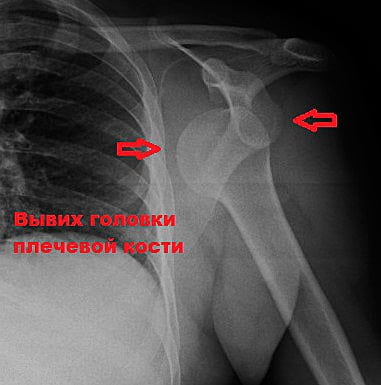
Diagnosis of shoulder ligament injuries
To properly diagnose the injury, the doctor must know the symptoms, timing, and circumstances of the injury. For a thorough examination, it is important to determine the nature of the pain to determine the extent of the ligament injury. The specialist may also ask about previous injuries and how they were treated.
By examining the patient, the specialist will determine:
To rule out sprains, fractures, breaks, and other mechanical injuries, an X-ray examination of the patient may be ordered. This is done if the doctor suspects that the shoulder ligaments are damaged.
Other diagnostic methods are usually:
- Arthroscopy – minimal surgical manipulation using special equipment;
- Ultrasound – examination using ultrasound waves;
- MRI – representation of the joint using a magnetic field.
Only a specialist can correctly assess the type and extent of a shoulder ligament injury. In addition, the symptoms of a dislocation are similar to other possible shoulder injuries, so it is sometimes difficult to determine which injury the victim has suffered.
Possible complications
Without medical treatment or self-treatment, even minor injuries to the elbow joint can lead to the following consequences
- Osteoarthritis – damage to the articular cartilage;
- nerve damage in the forearm or shoulder;
- Permanent restriction of mobility, etc.
Any complication complicates treatment of the underlying injury, and the effects of the above-mentioned conditions are long-lasting. It is therefore strongly recommended to consult a doctor at the first signs that indicate a ligament injury in the elbow.
Diagnosis of ligament injuries
To accurately diagnose a ligament injury and prescribe effective treatment, a surgeon, traumatologist, rheumatologist or neurologist can be consulted.
The doctor must first determine the circumstances and time of the injury. He or she will then take a history of your symptoms, the nature of your pain, and any previous injuries. The specialist will then assess the following
- the functionality and mobility of the elbow joint;
- the extent of the swelling
- the deformation of the joint;
- the presence or absence of bleeding on the skin.
During diagnosis, the doctor may perform examinations of the elbow joint to determine which ligament was damaged. Among additional examinations to diagnose the patient, the doctor may recommend the following.
- X-ray – helps rule out dislocations and fractures;
- MRI – to assess the extent of soft tissue damage;
- Arthroscopy – determines the presence of damaged ligaments, etc.
Various methods are also used to assess the damage described by the patient. This includes examining using a scale or scoring.
For a more accurate diagnosis of the damage, specialists may also recommend a general urine test and a biochemical blood test. The data from these tests may indicate joint disease. A urinalysis will be ordered if a serious injury is suspected.
General principles of treatment
Treatment strategies for ligament injuries depend on the severity of the injury. If the ligaments in the shoulder joint are partially torn, doctors recommend conservative treatment. This treatment usually helps the affected person regain their full ability to work. If there is a complete rupture, surgery is required.
Conservative treatment
This includes temporary lifestyle adjustments, medications and physical therapy treatments. Treatment can only be prescribed by a doctor after an examination. Before arriving at the hospital, experts advise patients to cool the injured shoulder with ice and fix the injured limb with a bandage or an improvised device.
How long does it take for a torn shoulder ligament to heal? If there are no complications, the affected person will fully recover within 2-3 weeks.
| method | Specific applications | action |
| Dry cooling | Ice should be wrapped in a clean, dry cloth before placing on the shoulder. The ice packs should be applied 4 times a day for 2 to 3 days. | The cold has a pain-relieving effect and helps reduce soft tissue swelling. |
| Immobilization of the limb | In the first few days after the injury, it is necessary to limit movement of the affected arm. During this time, the shoulder is often covered with a Deso bandage or a stiffening bandage. | Immobilizing the shoulder allows the torn connective tissue fibers to heal. |
| Administering painkillers and anti-inflammatory medications | To treat severe shoulder pain, medications from the NSAID group (diclofenac, ketoprofen, ibuprofen, meloxicam) are used. They are administered in the form of tablets or intramuscular injections. | NSAIDs relieve pain, fight tendonitis and other inflammatory diseases of the shoulder. |
| Physiotherapeutic treatments | Used in combination with other treatments for shoulder ligament tears. The most commonly used physiotherapy treatments are UHF and magnetic therapy. They do not require removal of the bandage and do not impair the immobilization of the joint. | They accelerate the regeneration of the damaged tissue, which allows the damaged ligaments to heal quickly. |
| therapeutic exercises | Are determined during rehabilitation, 1-2 weeks after the injury. A rehabilitation specialist or orthopedist/traumatologist selects a complex of exercises. | They help restore full function and normal mobility to the shoulder. |
AdobeStock_422305936-1.jpg

AdobeStock_422305936-1.jpg
Based on the clinical examination (anamnesis, complaints, examination and palpation of the joint), the doctor makes an initial assessment of the location and severity of the knee injury. For a reliable diagnosis, imaging procedures are used to display the structures and tissue of the knee using various techniques:
Visualizing the severity and location of the injury allows the doctor to choose the best treatment and rehabilitation measure.
Treatment
Once a knee ligament tear has been diagnosed, multidisciplinary treatment is recommended. Treatment consists of conservative and surgical approaches.
Conservative therapy is carried out with:
- drug treatment (anti-inflammatory drugs, diuretics to reduce swelling, cartilage protectors);
- Immobilization (immobilization of the joint);
- mandatory reduction of functional load on the limb.
For grade 1 injuries, only conservative treatment is usually given.
In the event of a complete rupture, surgical intervention is indicated. The aim is to restore the anatomical integrity of the joint structures and subsequently restore functionality. Various techniques are used in surgical treatment:
- Microsurgical reconstruction with suturing of the lesion using microinstruments and an endoscope.
- Autotransplantation – the damaged ligament is replaced with connective tissue fibers derived from other areas of the body.
- Allograft – a synthetic, durable material is used for the replacement, which has low reactogenicity and does not trigger a reaction from the immune system.
The choice of surgical technique depends on the type and severity of the knee injury and ligament tear. Treatment is always selected individually for each patient.
Rehabilitation after injury
Rehabilitation after this injury is not quick and can typically take 3 to 6 months. The pressure on the injured joint must be carefully controlled so as not to disrupt the fusion process.
Rehabilitation includes special exercises and rehabilitation exercises. Passive movements are the first step to training the joint. Active exercise is only allowed 6 weeks after the operation. Physiotherapy is prescribed to relieve swelling and pain after surgery.
Please apply online and we will contact you shortly to answer any questions you may have.
Ligamentoplasty
The cruciate ligaments are under constant tension, so sutures are ineffective in restoring their integrity. Only in Segunda fractures is bone integrity restored by fixation of the detached fragment. Reconstruction involves the use of an autograft, that is, the use of the patient's own tissue. In most cases this is the tendon of the semitendinosus muscle. The success rate of such operations is high. After rehabilitation, functionality is restored. However, plastic surgery is not necessary in every case.
Their need arises from:
- Intra-articular defect analysis results, no obvious effects of inflammation in the joint with extensive fibrosis and adhesions;
- Presence of knee instability, other functional knee disorders;
- sporting activity (willingness to return to sport with certain expected high-intensity loads).
Plastic surgery is not performed immediately, but rather some time after the injury. However, the operation should not be delayed for too long as the instability causes micro-damage to the articular cartilage, which can lead to osteoarthritis. An important prerequisite for surgery is the absence of internal inflammation. Preparation for surgery includes conservative treatment. This is followed by plastic surgery for autotransplantation. The rehabilitation period after such an operation is very important, and following the recommendations of the rehabilitation doctor has a significant impact on the recovery process.
rehabilitation
After arthroscopic surgery, the patient can go home on the day of the operation. It is recommended to ice the knee for a day and fix it with an orthosis. The patient will then perform exercises that are gradually increased. The therapeutic exercises are a series of exercises that are developed individually for each patient. At the beginning, the exercises are carried out during an outpatient hospital stay, then independently at home. Mechanical therapy – exercises on simulators are carried out at a later stage of rehabilitation. Physiotherapy treatments such as electromyostimulation, magnetic therapy and electrophoresis can also be very helpful. Recovery from arthroscopic surgery is quicker and easier than from open knee surgery.
forecast
After treatment and rehabilitation, the vast majority of patients can regain full limb function and athletes can resume training. However, the process is not quick and takes an average of six months. It is important to follow the specialist's advice and not cause new injuries.
This patient sustained an anterior cruciate ligament and collateral ligament injury 2.5 months ago. This video shows him conservatively treating an anterior cruciate ligament injury. Subjectively the knee is stable, but we still use various rehabilitation means such as a thread.
Contraindications for surgery
Although cruciate ligament plasty is one of the most popular techniques due to its high effectiveness and minimal invasiveness, it cannot be performed on every patient. Fortunately, there are not many contraindications:
- Pronounced contractures of the joint;
- Local skin infections, inflammations, purulent abscesses, ulcers;
- Severe abnormalities of the heart, respiratory system, veins and vessels in the legs;
- Any chronic illness that has become acute;
- Allergy to the drugs used for anesthesia.
If a transplant of autologous tendons of the quadriceps femoris or patellar ligaments is proposed and the patient has problems with the musculotendinous elements of the flexor and extensor apparatus, this procedure cannot be performed. However, he may be offered one of two alternatives: an allograft or implantation of the Legamis system. Of course, this only applies if the clinic offers such services.
Rehabilitation after surgery
After sacral ligament plasty, you will only have to walk on crutches without supporting your leg for about 1 month. You must immobilize the operated leg for about the same amount of time with a plaster cast, an orthosis or with orthoses that are rigidly fixed in a completely upright position. During this time, strain on the joint should be avoided. Painkillers and anti-inflammatory drugs are prescribed early on. As a rule, a special antibiotic is injected for several days.

Isometric exercises for BMSF shortening, ankle flexion and extension, prone positioning, and limb holding are performed for 2 weeks, starting approximately on the third day. In addition, the patient undergoes physiotherapy: magnetic therapy, UHF, electromyostimulation, etc. After about four weeks, the load on the leg is gradually increased and a transition occurs from crutches to a cane and then to walking without aids. In this phase, the rigid orthosis is replaced by a semi-rigid orthosis, preferably a frame model.

Therapeutic exercises and complex physiotherapy treatments must be carried out in a rehabilitation center under the supervision of a rehabilitation therapist for at least eight weeks. During this time, full knee mobility must be achieved and a normal gait established. This is achieved with the help of a special, non-rigid knee pad. A return to a normal life without restrictions is only possible after the replacement ligament has been permanently strengthened. With arthroscopic procedures, the final recovery of the cruciate ligament in the knee occurs at the earliest after 3 months, sometimes only after six months.
Video of rehabilitation protocol after knee arthroscopy:
Read more:- The ankle bruise is where the picture is taken.
- picture of the right foot.
- Femoral collateral ligament.
- Rupture of the medial collateral ligament.
- Pronation of the shoulders - what is it?.
- Collateral ligament rupture.
- Dislocation of a bone in a joint.
- tibial ligaments.
