During transport to the treatment facility:

- Treatment of herpes zoster in adults
- How does the herpes simplex virus get into the body and how does it make itself felt?
- species
- Symptoms of Keller's disease
- What is gout in women's feet?
- How to treat gout in Moscow?
- Diagnosis.
- treatment of osteophytes
- Ponseti on YouTube
- cost of treatment
- side effects.
- overdose
- Factors affecting wound healing
- treatment of lacerations
- solutions
- povidone iodine
- Chlorhexidine Bigluconate
- hydrogen peroxide
- Heptral®. Instructions for use
- instructions
- composition
- Description
- indications
- contraindications
- Use during pregnancy and lactation
- Why is there an indentation under my toenail?
- How is onycholysis treated?
Treatment of herpes zoster in adults
Herpes, or shingles as it is also known, is one of the most misunderstood viral diseases for the average person. It is often confused with other forms of shingles (pinky, ringworm, psoriasis shingles) caused by fungal infections of the skin and various autoimmune processes. In shingles, herpes simplex virus type 3, varicella zoster, causes clinical symptoms and skin lesions. This virus also causes the well-known chickenpox. So one and the same virus causes two diseases at the same time? But how is that possible? We want to find out! When a person first comes into contact with varicella zoster, the most common virus is chickenpox. They usually appear in childhood, but in rare cases they can also appear in adults. Read on to learn what happens if the virus breaks out a second time. You will also learn how to find a cure for herpes simplex.
- How does the herpes virus get into the body and how does it make itself felt?
- Herpes zoster: symptoms and treatment
- How to treat hemorrhagic herpes, gangrenous herpes zoster and other forms
- Possible consequences of not treating herpes labialis
- Diagnosis and proper treatment of herpes zoster in adults
- The back: treatment with folk remedies
- Dorsal: treatment, medication and therapy
- VIFERON – antiviral drug used to treat herpes zoster
- How to use ointment for herpes simplex
Everyone knows that herpes viruses never leave the body, and varicella zoster is no exception. It penetrates nerve cell clusters, 'hibernates' and often stays with us forever without showing itself. However, if the virus is exposed to external factors, it can still wake up and cause shingles. Contact with a person who has chickenpox can also lead to the development of hemiplegia. This happens when a person, most often an elderly person with weakened immunity, comes into contact with a sick child. The very name of the virus is interesting: 'varicella' is commonly referred to as chickenpox, while 'zoster', meaning 'belt', is associated with impetigo because of the rash that characterizes the disease, appearing on the lower back and abdomen .
How does the herpes simplex virus get into the body and how does it make itself felt?
In most cases, the first infection with the virus that causes OH occurs in childhood, when a child contracts chickenpox through airborne droplets. After recovery, the virus persists for a long time in the peripheral nerve plexuses, the spinal ganglia (limited collections of neurons), and the cerebral ganglia. Immunodeficiency states can lead to reactivation of the virus when the natural defenses are weakened and the disease has a chance to become fully active.
The main factors that can trigger a GI are.
- age-related changes in the body – according to statistics, the disease most often occurs in people over 50 years of age;
- autoimmune diseases and cancer, including diabetes, radiation and chemotherapy, and conditions following major trauma;
- Pregnancy and the resulting increased load on the body;
- HIV infection – nearly 25 % of those infected with HIV have OH, which is eight times the average for middle-aged and elderly patients;
- Organ transplants, which require immunosuppressive drugs to artificially suppress immunity to prevent organ rejection; and
- the recurrence of chronic diseases of the cardiovascular system, kidneys, liver and lungs;
- Prolonged treatment with antibiotics, cytostatics, glucocorticosteroids;
- Frequent stress, insufficient rest, excessive physical exertion, hypothermia or overheating of the body.
species
In the pathogenesis of osteochondropathy, the following stages are usually distinguished:
- Ischemic damage - associated with impaired oxygen and nutrient delivery;
- Infarction - foci of osteochondral necrosis appear as a result of a critical circulatory disorder;
- Necrosis – at this stage, the area of necrosis increases in size;
- Subchondral fracture with joint surface collapse – the integrity of the bone is compromised in the subchondral area;
- Resorption and remodeling – the phagocytic system lyses necrotic fragments and partial structural repair occurs.
There are four types of Freiberg-Keller pathology:
- Type I is a transient lesion that does not show deformation of the articular surfaces of the metatarsal head - treatment in this case is limited to conservative methods;
- In type II, a pronounced ischemic lesion leads to an extrusion fracture in the proximal part of the metatarsal head, without cartilage involvement, but with the development of periarticular bone hypertrophy (surgical treatment is indicated at this stage);
- Type III pathology is characterized by severe damage to the cartilage covering the metatarsal head and severe proliferative and degenerative changes in the metatarsophalangeal joint – treatment of this type (at this stage conservative treatment is completely ineffective, so surgery is performed to restore the anatomy of the articulating ends of the bones - they must correctly reproduce their shape);
- Type IV is a rare variant in which multiple metatarsal heads are affected simultaneously (treatment is surgical and must match the specific stage of the lesion for each metatarsal head).
Symptoms of Keller's disease
The first symptoms of Keller's disease include pain in the affected metatarsophalangeal joint, which occurs when walking, especially when walking barefoot. Patients report feeling like walking on stones or 'lumps in the toe'. The progression of the pathological process leads to increasing pain and reduced mobility in the affected joint. The area around the metatarsophalangeal joint of the big toe deforms, causing swelling and a characteristic crunching sound when the joint surfaces are moved. In later stages, hammer toe deformity of the toe occurs and its supportive function is compromised.
The cutaneous manifestations appear in the form of pathologic keratoses and hard calluses on both the plantar and dorsal surfaces of the affected joint as a result of pathologic conflict with the components of the footwear.
What is gout in women's feet?
Under the influence of provocative factors in women, the natural processes of excretion and entry of uric acid into the body are disrupted, and the levels of urea in the blood increase significantly. This is due to insufficient production of estrogens, which begins in women with menopause. Therefore, gout most often occurs in women over 50 years of age with acute lack of sex hormones and disorders of the endocrine system. The main symptoms are:
- tofu formation (accumulation of urate in the joint tissues);
- nephrolithiasis (accumulation of urate in the kidneys with subsequent formation of calculi);
- Gouty (uric) nephropathy.
How to treat gout in Moscow?
The rheumatologists at the Yusupov Hospital know how to treat gout in the legs. In the fight against acute arthritis, the doctors of the Yusupov hospital use several pharmacological groups at once:
- Nonsteroidal anti-inflammatory drugs (such as ibuprofen, indomethacin, diclofenac);
- Uric acid-lowering drugs (Anturan, Butadione, Cetazone);
- Corticosteroids (prednisolone, dexamethasone, triamcinolone).
Gout injections in the legs are used to relieve pain. The choice of drug depends on the patient's condition and his pain threshold, which the doctor directly determines.
As an additional treatment for gout, rheumatologists recommend applying iodine ointment to the affected areas every night. This can reduce inflammation, speed up the healing process, and reduce pain. To enhance the effect, aspirin should be added to the iodine, and the finished mixture should be regularly applied to the affected joints.
Yusupov Hospital actively uses physiotherapeutic treatment methods that effectively reduce inflammation and the number of attacks, prevent urate stagnation and restore diseased joint tissues. To this end, the hospital has:
- electrophoresis;
- phonophoresis;
- ultratunophoresis;
- heat treatments;
- magnet therapy;
- amplipulse;
- Ultrasonic.
Doctors at Yusupov Hospital put together an individual nutritional program to exclude foods that trigger a gout attack. The hospital's rheumatologists prescribe therapeutic exercises to restore the former mobility of the joints, normalize blood circulation and metabolic processes in the body, and strengthen the patient's muscular apparatus.
If you have gout in your big toe and you need treatment, you should contact the specialists at Yusupov Hospital. Doctors will conduct a comprehensive examination that includes:
Diagnosis.
At the reception, the doctor takes an anamnesis and an external examination of the patient and listens to his complaints. A neurological exam is then performed to diagnose nerve compression and assess nerve root sensitivity.
The following instrumental examinations are carried out to confirm the initial diagnosis and exclude pathologies with a similar clinical picture:
- X-rays - a fundamental step in identifying growths;
- Electroneuromyography – to determine the current state of the peripheral nervous system;
- CT – shows bone density and texture, the current condition of the vertebrae, visualizes tumors, trauma and other pathological changes;
- MRI - depicts bones, muscles, cartilage, blood vessels and nerves in detail, detects most pathological changes.
treatment of osteophytes
How can the disease be treated? Treatment of osteophytes of any localization begins with treatment of the underlying pathology. How can bone outgrowths be treated conservatively? The main therapeutic measures are listed below:

- therapeutic treatment – relieving inflammation, pain, restoring local metabolic processes using NSAIDs, chondroprotectors, which helps slow down further destruction of joint tissues;
- Physiotherapy – the method is selected by the doctor depending on the type of growth, its location, the patient's age, the presence of concomitant diseases and the individual characteristics of the body
- Physical therapy – relieves muscle spasms, improves local metabolic processes, reduces loads on painful joints;
- Massage;
- healthy lifestyle (avoidance of bad habits, work and rest, avoidance of stress);
- Avoiding a sedentary lifestyle, regular walks in the fresh air;
- use of orthotics (corsets, cuffs and others);
- proper nutrition (adults should avoid fast food, fried, spicy, salty and smoked foods, and eat more greens, fresh fruits and vegetables, as well as nuts, fish, seafood and other foods rich in magnesium and calcium);
- Weight loss (for obese people Source:
Dysphagia secondary to esophageal compression by cervical osteophytes. Kirilenko SI, Litvin AA, Kryzh SA, Rozhin VV Surgery News, vol. 23, no. 6, 2015. pp.688-692 ).
Such treatment cannot reverse the process and eliminate the bone outgrowths. However, it is possible to stop the progression of the disease, reduce the size of the outgrowth and relieve unpleasant symptoms. How to get rid of osteophytes if conservative therapy does not help? In this case, an operation is indicated in which the growths are surgically removed.
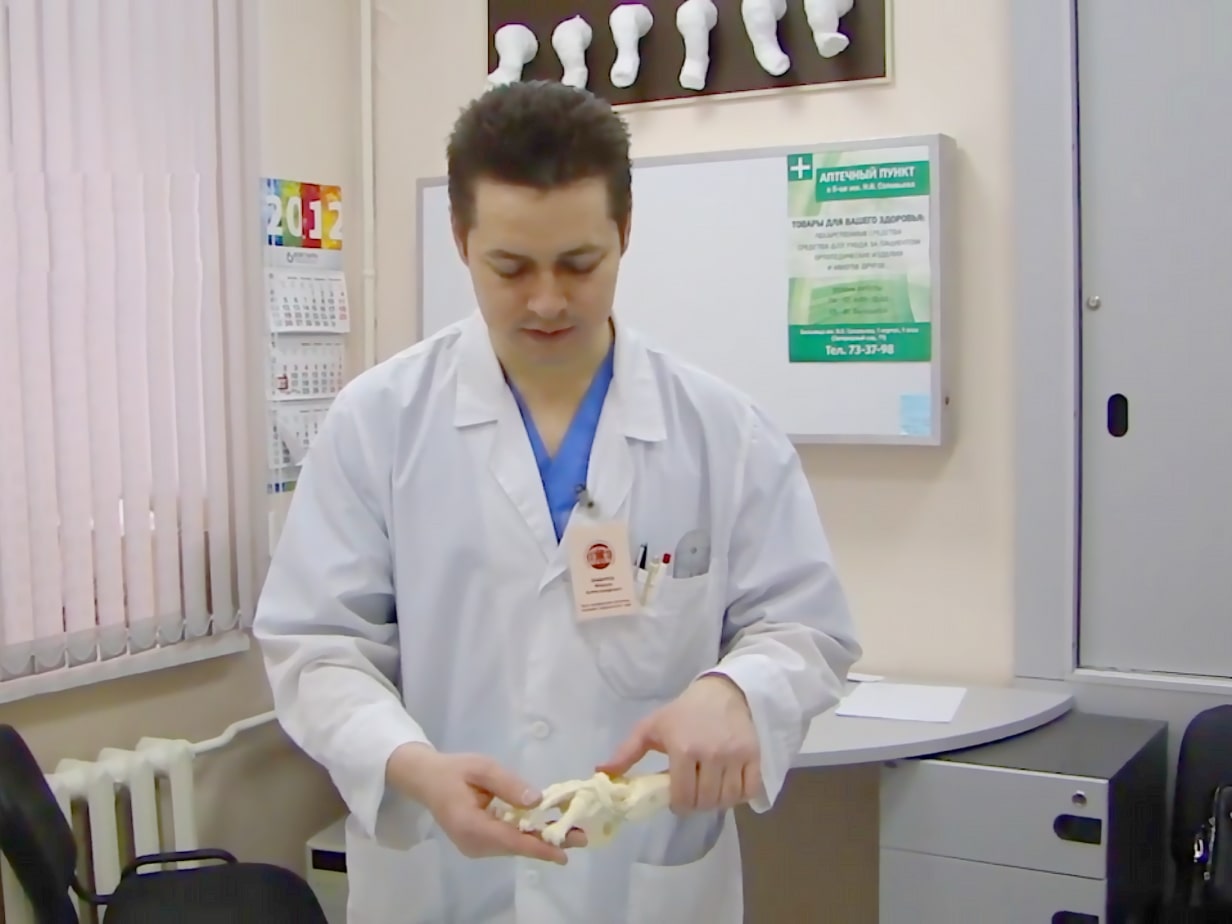
Ponseti on YouTube












cost of treatment
The total cost of treatment depends on the severity of the deformity and the number of casts needed to completely correct the deformity, as well as the number of feet with clubfoot (clubfoot)
Clubfoot is a common foot deformity characterized by a deviation from the long axis of the femur and tibia. Clubfoot has the following characteristics: the foot is inward, the outer edge is downward and backward, the inner concave edge is upward. The disease occurs in Russia in 1-3 cases per 1000 newborns.
Clubfoot is currently being treated successfully. The main goal of treatment is to eliminate all elements of the deformity or to significantly reduce its severity in order to achieve a functional, flexible, pain-free, strong, supportive foot with normal shape and the ability to wear normal anatomical footwear. The Russian Ponseti Association was formed to consolidate the efforts of orthopedic surgeons in treating severe clubfoot using the Ponseti method with a common algorithm.
The association consists of pediatric orthopedic surgeons who use the Ponseti method to treat severe clubfoot and the Dobbs method to treat vertical shoulder in children. By joining the association, the specialists have demonstrated their expertise in treatment. On November 30, 2012, the Russian Ponseti Association was officially recognized by the Ponseti International Association (PIA). More and more traumatologists in Russia and around the world are using the Ponseti method in the treatment of clubfoot, since this method is minimally invasive, short and effective, and in most cases it is able to correct a severe deformity within 2-3 months, while in 95 % of the cases a positive result is obtained.
side effects.
The following side effects may occur when using the drug: allergic reactions (itching of the skin, urticaria), burning, irritation and numbness of the nasal mucosa, dry mouth, redness of the eyes, atopic dermatitis, Quincke's edema, anaphylactic shock. If any of the side effects listed in the leaflet occur or worsen, or if you experience other side effects not listed in the leaflet, tell your doctor.
Salts of zinc, copper, lead, silver, mercury, iron, aluminum form insoluble precipitates with silver proteinate solution; Silver proteinate is inactivated by alkaloid salts and organic bases (epinephrine). If you are taking any of the above or any other medicines (including over-the-counter medicines), consult your doctor before taking the medicine.
overdose
If used as directed, an overdose is unlikely. Increased side effects in the form of irritation, burning of the nasal mucosa, itching of the skin are possible after excessive use. Accidental ingestion may cause irritation of the gastrointestinal tract.
Read these instructions for use carefully before use as they contain important information for the patient.
Please keep this manual safe, as you may need it again.
If you have any questions, consult your doctor.
The medicine you are being treated with is for you personally and must not be given to other people as it may harm them, even if they have the same symptoms as you.
If any of the side effects listed in the leaflet worsen, stop treatment. Your nasal discharge may turn gray or blue. The recommended doses should not be exceeded, especially in children and the elderly.
Effect of the drug on driving ability and mechanisms.
The drug does not affect the ability to drive or other potentially dangerous activities that require high concentration and rapid psychomotor reactions.
Factors affecting wound healing
Wounded skin heals at different rates depending on individual body characteristics and environmental factors:
- A person's general health
- Age – older people have slower skin regeneration times than younger people
- state of the immune system
- eating habits
- weather conditions
- How infected the wound is
- Bad habits (smoking, alcohol, drugs)
- Associated diseases (diabetes, cancer)
treatment of lacerations
There are numerous preparations for the treatment of lacerations, both in the form of active ingredients and dosage forms 4,5,6 .
solutions
povidone iodine

Betadine® is available in a concentration of 10 %. For use on lacerations, it can be used neat or diluted 1:10 as a 1%ige solution (2 x 5 mL (2 teaspoons) and 100 mL (½ cup) of a 10%ige solution) 2,3 . Dilute with saline, Ringer's solution, phosphate buffer solution, water for injections or, as a last resort, clean drinking water.
Povidone iodine has antiseptic, antiviral, antifungal and antiprotozoal effects.
It is effective against gram positive and gram negative bacteria.
Unlike 5%iger Alcoholic Iodine Solution, Povidone Iodine can be applied directly to the wound. It does not burn, does not dry out the skin and does not interfere with tissue regeneration.
Chlorhexidine Bigluconate
Chlorhexidine bigluconate is an antiseptic that fights bacteria, fungi, and viruses. It is available as an aqueous and alcoholic solution. A 0.2-0.5% aqueous solution should be used to treat cuts. An alcohol-based preparation can cause uncomfortable burning reactions and slow down the healing process.
hydrogen peroxide
This solution is prepared and used at a concentration of 3 %. Hydrogen peroxide has a hemostatic effect and contributes to the mechanical removal of debris from the wound by the formation of gas bubbles. Using hydrogen peroxide can cause allergic reactions.
Heptral®.
Instructions for use
A source of active amino acids essential to liver function, Heptral ® stimulates the initiation of natural* liver cell repair from within. Heptral ® helps eliminate toxins and improves liver function after 1 week of use 1-3.




instructions
composition
Active ingredient: Ademetionine 1,4-butanedisulfonate 760 mg (equivalent to 400 mg ademetionine ions).
Excipients: Colloidal Silicon Dioxide - 4.40 mg, Microcrystalline Cellulose - 93.60 mg, Sodium Carboxymethyl Starch (Type A) - 17.60 mg, Magnesium Stearate - 4.4 mg; Tablet coating: methacrylic acid and ethyl acrylate copolymer (1:1) - 27.60 mg, macrogol-6000 - 8.07 mg, polysorbate-80 - 0.44 mg, simethicone emulsion (30%) - 0.13 mg, sodium hydroxide – 0.36 mg, talc – 18.40 mg, water – QS
Description
Oval, biconvex, smooth, white to pale yellow, film-coated tablets.
indications
- Adjuvant therapy in pre-existing chronic liver disease to improve and maintain liver function.
- Worsening of fatigue in existing chronic liver disease.
contraindications
Genetic disorders affecting the methionine cycle and/or causing homocystinuria and/or hyperhomocysteinemia (cystathionine beta synthase deficiency, vitamin B metabolism disorders).12).
Hypersensitivity to ademetionine and/or any of the excipients of the preparation.
Under 18 years of age (since there are no data on the efficacy and safety of ademetionine in this age group).
If you have any of the above diseases/conditions or risk factors, consult your doctor before taking this medicine.
Use during pregnancy and lactation
Talk to your doctor before taking Heptral® if you are pregnant, think you may be pregnant, or are planning to have a baby. If you are breast-feeding, consult your doctor before taking Heptral®.
Heptral® should not be used during pregnancy and breastfeeding without medical supervision.
Why is there an indentation under my toenail?
- A trauma of the nail;
- chemical burns from the use of low-quality gel nail polishes or from contact with household chemicals or other aggressive substances;
- thinning of the nails by removing artificial nail polish or filing the nail plate with a file or bur through a manicure;
- Onychophagia, a mental disorder in which a person bites or picks at the nail plate and the skin surrounding it. This causes the nail to detach from the nail bed;
- Try to push away the hyponychium or use something sharp to remove the dirt from under the nail;
- Dermatological abnormalities.
If you noticed the first signs of onycholysis, contact Podolab in St. Podiatrists will advise you on the problem. They will quickly restore the attractive appearance of your nails.
How is onycholysis treated?
The sooner you see a podiatrist or dermatologist to determine the cause of your peeling nails, the better chance you have of successfully eliminating the problem.
During toenail recovery, there is a strict prohibition on all traumatic treatments, nail extensions, decorative nail polishes and harsh chemical liquids.
If the fungal spores have entered the cavity under the nail, and the onycholysis is infectious, the treatment of onychomycosis is prescribed by a dermatologist.
If your fingernail plate occasionally comes off, you likely need to see an endocrinologist and have your hormone levels corrected.
The specialists of the center professionally and painlessly treat the nail plate with onycholysis on the feet and hands using modern equipment.
They will also provide home care recommendations to avoid recurrence.
Read more:- The Ponseti method.
- Ponseti breeches.
- Sesame legs of the hock.
- 1 year old child with clubfoot.
- Congenital clubfoot.
- Photo of scraped feet.
- Clubfoot in 7-year-old children.
- clubfoot.
