Damage can occur at different levels, both proximally - above the lateral malleolus - and at the level of the calcaneus tuberosum, the lower attachment point of the peroneus muscle.

- Disease in terms of gonarthrosis of the knee
- Anatomy of the knee joint
- Classification of damage to the superior Ogden tendon retainer of the eye muscles.
- Symptoms of a tendon injury of the upper arm muscle.
- causes
- symptoms
- Peroneus brevis muscle
- denervation
- Peroneus brevis muscle
- denervation
- causes
- signs
- Structure of muscles, muscle biology
- causes
- symptoms
- Different treatment methods
- pharmacotherapy
- Sagittal nerve block
- surgical intervention
- Orthopedic correction
- Treatment of femoral neuropathy by an osteopath
Disease in terms of gonarthrosis of the knee
This is a non-communicable disease that mainly affects the hyaline cartilage of the knee joint - it gradually degrades and loses its function, further damaging other parts of the joint, leading to deformity.
It is a degenerative dystrophic disease that usually affects women over the age of 40, but also men, especially those who are overweight and often hyperactive, play sports or have suffered injuries.
Of all osteoarthritis, gonarthrosis of the knee is the most common.
It is believed that the cause of gonarthrosis is salt deposits in the joint. This opinion is completely wrong. The salt deposits are more of a secondary process and cause pain as the disease progresses and lodges at the tendon and ligament insertions. The key to preventing the disease is prevention.
Anatomy of the knee joint
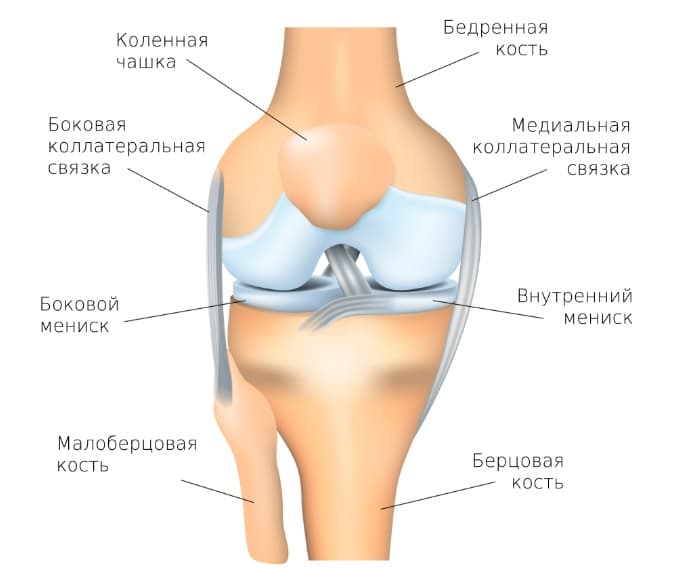
The knee joint consists of two surfaces formed by the tibia and femur. The kneecap, which runs between the condyles of the thigh, protects the knee joint from the front. The fibula is not involved in the formation of the knee joint and actually has no functional load, which is why it is often used to reconstruct other bone elements in the body.
All articular surfaces of the tibia, femur and the inner side of the patella are lined with hyaline cartilage, which is very smooth and characterized by high strength and elasticity, 5-6 mm thick. The cartilage provides cushioning during motor activities, prevents friction and softens impacts.
Classification of damage to the superior Ogden tendon retainer of the eye muscles.
Grade 1 – the bracket is partially detached from the fibula, resulting in subluxation of the fibula muscle tendons.
Grade 2 – the retainer is detached from the fibrocartilage crest resulting in tendon overlap between the crest and retainer
Grade 3 – the fibrocartilage crest is torn along with the periosteum or cortical plate, resulting in subluxation of the tendons between the bone and the detached fragment
Grade 4 – The tendon is detached from the heel bone and the tendon is displaced under the skin.
Symptoms of a tendon injury of the upper arm muscle.
Patients often describe the injury as a sudden severe dorsiflexion of the foot, often with a snapping or clicking sensation in the lateral malleolus.
Patients complain of popping, snapping, a feeling of instability, and pain on the outer surface of the ankle.
Examination for an acute injury may reveal swelling at the posterior surface of the lateral malleolus, pain on palpation of the fibular tendons, and tendon subluxation with muscle strain. With passive dorsiflexion, the patient feels subluxation and instability, and sometimes a dislocated tendon can be felt.
Ultrasonography and MRI are important for diagnosis and often show abnormalities such as the fourth foot muscle, the lower abdomen of the short fibula.
causes
Neuropathy poses many problems due to the location of the tibial nerve, because regardless of the type of neuropathy (compressive - ischemic, compressive - post-traumatic), it complicates movement and immobilizes the affected person.
Among the causes that can lead to this pathological condition are:
- Actual trauma, trauma. Direct rupture of the nerve bundle or its compression by scarred keloid tissue after lower leg surgery. With possible simultaneous damage to the tibial nerve fibers.
- Tumor processes with localization in the lower limbs and in women with a gynecological profile. As the nodule grows, there will be metastasis and possible compression in the area of the nerve. This impairs the ability to transmit signals to tissues.
- Toxic lesions that develop as a result of disease. Kidney failure, diabetes and alcoholism are common causes.
- vascular diseases. A lack of blood supply and the resulting lack of oxygen lead to ischemic damage and death of nerve endings and fibers and the loss of the ability to perform their function.

- Various types of infections.
- Staying in an extremely uncomfortable position for the lower limbs for a long time due to work or study. Poor posture leads to the symptoms of tunnel syndrome (neuropathy, neuropathy) of the foot nerve.
Chronic diseases (diabetes), poisoning (industrial toxins and alcohol) lead to the death of nerve fibers and to polyneuropathy. This process is usually bilateral. Physical factors - trauma, tumor, poor posture - lead to unilateral sagittal syndrome.
Some systemic diseases also lead to inflammation of the sagittal nerve as a complication. These include gout, rheumatoid arthritis and osteoporosis.
symptoms
The inflammation, damage, and excessive pressure that lead to femoral neuropathy cause more or less the same symptoms. Manifestations develop at different rates depending on the type of damaging effect.
The compression of the fibers initially leads to overactivity, in which the foot contracts. If the nerve then dies, the foot muscles become paralyzed.
Ischemic disorders develop slowly and insidiously. Sensory disorders are the most common starting point: the skin of the lower leg and foot becomes hypersensitive and then numb.
A traumatic injury, e.g. B. a car accident is characterized by the immediate onset of symptoms of periarticular neuropathy.
The symptoms and signs of periarticular neuropathy depend on the type and extent of the injury:
- With compression from chronic poisoning of various kinds or diabetes, alcoholism, 'tingling' begins and sensitivity is gradually lost. Mobility remains at the same level.

- Immediate trauma leads to pain syndrome. There is weakness and tension when trying to move the foot. There is pain on the lateral surface of the shin towards the toes, especially in the lower part of the shin, with an additional burning sensation. There may be a feeling of numbness.
- A deep branch lesion results in a slight plantar flexion of the foot (as pictured at the beginning of this article) and a loss of mobility in the toe area. The muscles in this area gradually atrophy and localized sensory loss occurs.
Peroneus brevis muscle
B short fibula muscle muscle (or fibular muscle) lies under the sheath of the long fibula muscle and is the shorter and smaller of the fibula muscles.

The short fibula (extreme lower mark) is a lower leg muscle that helps with plantar flexion and extension of the foot.
It arises in the lower two-thirds of the lateral surface of the fibula shaft, medial to the long muscle of the fibula and at the intermuscular septum that separates it from the adjacent muscles of the fore and hind legs.
The fibers descend vertically and terminate in a tendon that runs behind the lateral ankle along with the preceding muscle, but in front of this both tendons are compartmentalized and lubricated by a common mucosa.
It then travels forward on the lateral aspect of the calcaneus over the calcaneus tuberosity and tendon of the long muscle of the fibula and meets the tubercle at the base of the fifth metatarsal on its lateral aspect. When the base of the fifth metatarsal is fractured, the short fibula can pull and displace the proximal fragment (Jones fracture). Inversion of the foot can stretch the tendon enough to tear the tubercle at the base of the fifth metatarsal.
denervation
It is innervated by the superficial oculomotor nerve (fibular nerve).
Peroneus brevis muscle
B short fibula muscle muscle (or Fibula muscle (peroneus muscle)) lies under the sheath of the peroneus longus muscle and is the shorter and smaller of the two fibula muscles.

The musculus peroneus brevis (lowermost mark) is a lower leg muscle that assists in plantar flexion and foot extension.
It arises in the lower two-thirds of the lateral surface of the fibula, medial to the fibula longus and at the intermuscular septum that separates it from the adjacent forefoot and hindfoot muscles.
The fibers descend vertically and terminate in a tendon that runs behind the lateral ankle along with the preceding muscle, but in front of it both tendons are compartmented and lubricated by a common mucosa.
It then runs forward on the lateral side of the calcaneus, via the calcaneus tubercle and the tendon of the long fibular muscle to the basal tubercle of the fifth metatarsal bone on its lateral side. In a fracture of the base of the fifth metatarsal, the short fibula can pull and displace the proximal fragment (Jones fracture). When the foot is inverted, the tendon can be stretched enough to rupture the tubercle at the base of the fifth metatarsal.
denervation
It is innervated by the superficial ankle nerve (Nervus peroneus).
causes
Peroneal neuralgia is most commonly caused by compression of the ankle nerve from anatomical structures, usually near the bone head. Thickening of the walls of the anatomical tunnel can be caused by a general disease (gout, polymyositis, rheumatoid arthritis, diabetes, osteochondrosis, etc.).
Contribution to the development of inflammation of the fibula nerve (neuralgia):
- Trauma;
- Prolonged standing in a squatting position, kneeling;
- Acute and chronic infectious diseases;
- Poisoning from heavy metals, alcohol, etc.; – wearing tight-fitting shoes;
- wearing close-fitting footwear;
- Poor blood circulation in the legs due to thrombophlebitis or other diseases of the arteries and/or veins;
- canker sores etc.
signs
The appearance of nerve inflammation (neuralgia) in the foot nerve depends on which part of the nerve is affected.
The deeper branches affect the flexion and extension of the backs of the fingers and toes, and the feeling between the first two fingers is reduced.
If the pathology develops in the upper part of the nerve, the muscle function on the front of the tibia is affected.
Inflammation of the superficial branch is accompanied by paralysis of the peroneal muscles.
If the common ankle nerve is damaged, all or more of the symptoms described above can occur, but also
- dying off of foot with inward roll and toe flexion;
- 'Cockerel gait' (stepping, peroneal gait) – when walking, the foot is raised high so that the toes do not touch the surface, and when lowering, the toes first touch the foot, then the outer edge of the foot and then the heel;
- inability to move on the heel;
- Pain (peroneal neuralgia), which is usually mild with a burning sensation, and is located on the posterior, external surface of the lower leg and foot.
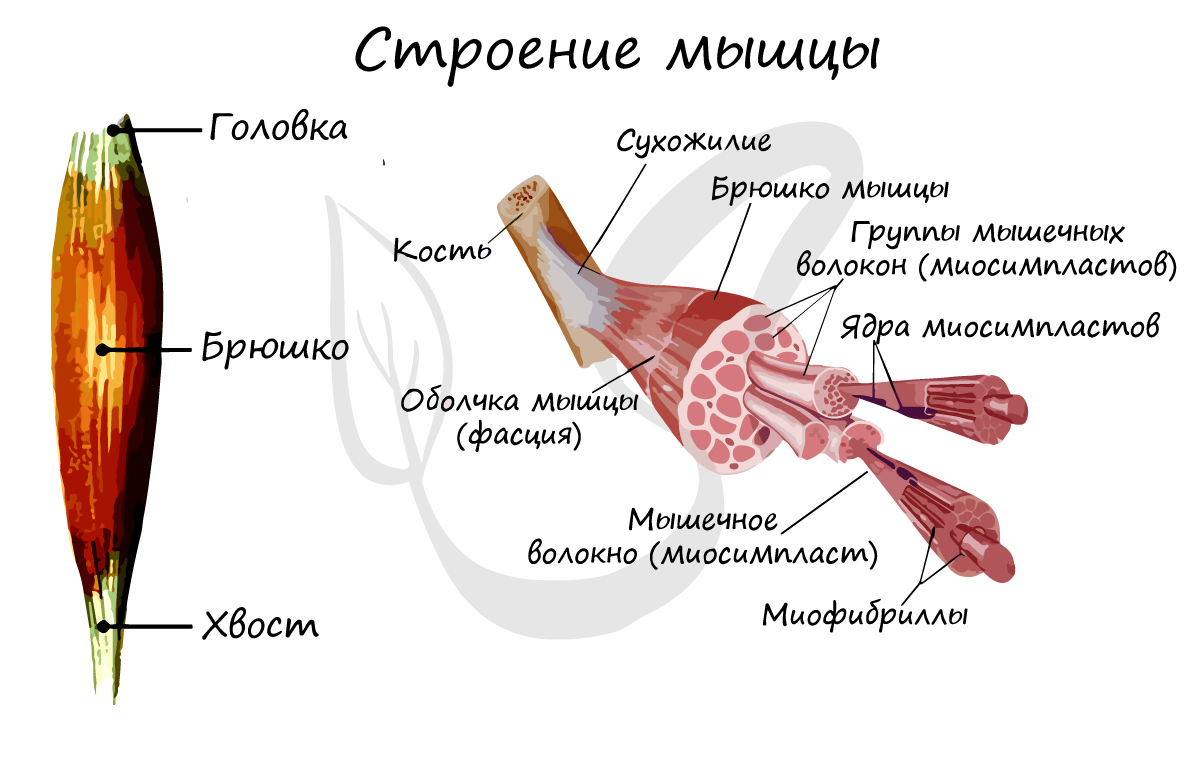
Structure of muscles, muscle biology
The muscles are the active part of the musculoskeletal system. When they contract, they move bony levers: movements are made to make the body and its parts move through space.
building the muscles
Muscles are made up of numerous muscle fibers that form the abdomen of the muscle. A distinction is made between the head and the tail of the muscle: the head is attached to a fixed element, while the tail attracts the moving part of the skeleton when the muscle contracts.
In Muscle Tissue, we took an in-depth look at the structure of striated muscle tissue, which allows us to perform voluntary (mind-controlled) movement. Striated muscle tissue consists of long, multinucleated fibers - myofibrils - that are striated by a basic unit - the sarcomere. The sarcomeres combine to form myofibrils, which form the myotubes.
antagonists and synergists
A distinction is made between antagonistic and synergistic muscles. Antagonistic muscles (from the Greek: antagonistes) are groups of muscles that are parallel to each other and contract to cause the bony arms to move in opposite directions. Simply put, one flexes and the other extends the limb. The most obvious examples of antagonistic muscles are the biceps and triceps.
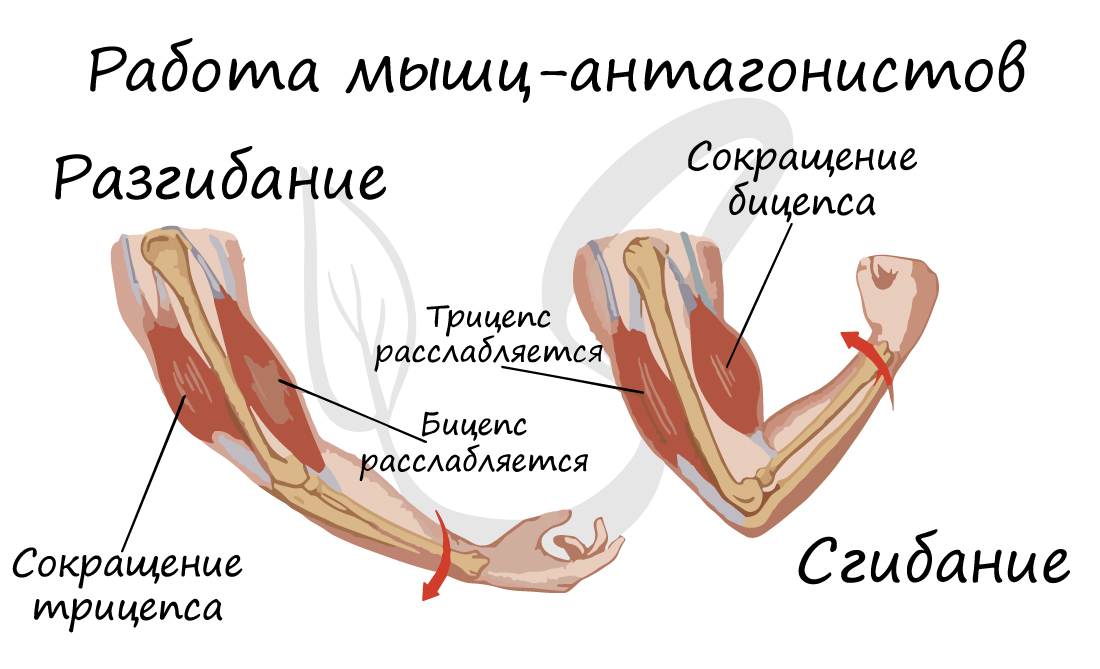
Synergistic muscles (from Greek synergos - working together) are muscles that work together to perform a specific movement. Examples of synergistic muscles are the brachialis and biceps.

causes
Shin splints are most commonly diagnosed in people whose jobs require prolonged kneeling or standing. This is how it most often occurs in furniture assemblers, builders, farmers, etc.
But habits like sitting on your thighs and knees for long periods of time can also cause ankle nerve compression:
- Sitting for long periods with crossed legs;
- Sitting in an unsuitable chair with your legs dangling;
- sleeping with bent legs hanging over the edge of the bed;
- sitting in a chair with your legs drawn up for a long time, as is common for many office workers.
Direct trauma to the knee joint, fibula head, or immobilization of the limb with a cast as a result of fractures, dislocations, certain surgical procedures, etc. can also cause fibula canal syndrome. Also, inflammatory muscle diseases, tumors in the knee area, bruises and swelling of the lower limbs caused by the development of certain pathologies lead to nerve compression.
symptoms
Pinching of the peroneal nerve is accompanied by specific symptoms:
- Various sensory disturbances such as numbness, tingling, goosebumps and burning sensation on the outside of the lower leg and in the dorsiflexion of the foot, affecting the first toe space but not the big toe, and feeling tends to disappear after walking or moving the foot;
- peripheral paresis (muscle weakness) of the extensor muscles of the foot, causing wobbly foot, gait disturbances, reduced stability when walking and frequent stumbling when walking, forcing the patient to lift the affected foot with each step, known as 'houndstooth';
- inability to draw the toes of the foot together;
- Pallor, dryness, coldness of the skin on the lower leg and foot.
In most cases, sensory and other disturbances are observed within 1 to 24 hours, but they can also occur much longer, even lasting 10 days or more.
The disease tends to be insidious. If it is not treated early, pain will appear later in addition to the sensory disturbances. The pain can be burning or stabbing. With increasing muscle weakness, the pain decreases and is replaced by a pronounced bending of the foot when walking. As a result, there is a decline in the lower leg muscles (atrophy), which is visible to the naked eye in severe cases.

Different treatment methods
pharmacotherapy
Alpha-lipoic acid supplements (Thioctacid, Berlithion, Espalipon) are prescribed to restore the nerve's myelin sheath. Along with other neurometabolic drugs, a combination of B vitamins (Milgamma, Combilipen, Neuromultivit) is traditionally used or the combination drug Celtican, which is approved in Russia as a dietary supplement, is prescribed.
The use of nonsteroidal anti-inflammatory drugs for periarticular neuropathy is ineffective because the cause of the persistent pain is less inflammation of the soft tissues and more damage to the nerve itself. These pains are neuropathic and require drugs from other groups: anticonvulsants (gabapentin, Lyrica, Finglepsin); Antidepressants (amitriptyline, Symbalta, Ixel).
Sagittal nerve block
If the pharmacotherapy is not sufficiently effective, a nerve block can be performed at the fibula head. A local anesthetic (lidocaine solution) is injected in combination with a hormone preparation (dipropane, dexamethasone). The clinical effect occurs after a single treatment. If necessary, with persistent pain syndrome, a series of blocks can be performed.
surgical intervention
Surgical intervention is performed:
- A mass in the soft tissues of the knee joint that causes compression of the ankle nerve (Baker's cyst, knee ganglion)
- For trauma that has damaged the nerve trunk
- Anterior muscle bed syndrome of the lower leg
Orthopedic correction
To prevent the ligaments in the ankle from being dislocated, the foot is immobilized with a special orthosis. All factors that can cause compression of the nerve in the upper third of the lower limb (high, tight shoes, squatting, prolonged sitting upright) are excluded.
Treatment of femoral neuropathy by an osteopath
Osteopathic treatment of tunnel neuropathies includes work on nerve compression (relaxation of the musculo-fascial structures that can compress the nerve trunk) and diagnostic and therapeutic techniques on the nerve structures of the affected limb from the spinal root to the terminal branches of the peripheral nerves in order to to eliminate possible double compression of the fibers of the oculomotor nerve on several levels.
Preventive measures include treatment of underlying diseases that can increase the risk of tunnel neuropathy (diabetes mellitus, polyarthritis of the nodules); the correct application of a plaster splint for lower leg fractures; avoiding positions that can result in compression of the ankle nerve.
Read more:- Syndrome of the tibial nerve.
- Tibialis posterior muscle.
- Long fibula muscle.
- Triceps femoris muscle.
- Longitudinal soleus muscle.
- Square soleus muscle.
- Cracked metatarsal.
- Exercises for the triceps tibialis muscle.
