External subluxation of the foot is diagnosed by a widening or deepening of the space between the articular contour of the medial malleolus and the adjacent articular contour of the talus, which usually matches the width of the remaining articular space in the ankle.
- DUPUYTREN'S FRACTURE
- clinical picture
- subluxation of the talus
- Treatment of heel fracture dislocations
- sprains of the pelvis
- symptoms of a dislocation
- First aid measures for a sprained ankle
- professionals in this field
- Glazova Natalia Alekseevna
- Torno Timur Eduardovich
- Maxim Alexandrovich Vavilov
- Our patients
- Anastasia
- Miroslav
- Alexander
- Maria
- Filipp
- description of the case
- discussion
- Показания к вправлению вывиха голеностопного сустава.
- Contraindications for ankle sprains
- Indications for ankle dislocation
- Contraindications for ankle dislocations
- Symptoms of an ankle dislocation
- What exactly is a sprained ankle?
- Treatment
- complications
- prevention
- What questions should you ask your doctor?
- Tips for the patient
DUPUYTREN'S FRACTURE
Dupuytren's fracture (G. Dupuytren's fracture) (G. Dupuytren, French surgeon, 1777-1835) is a fracture of the medial ankle and lower third of the fibula with a tear of the syndesmotic ligaments. This fracture often results in external subluxation of the foot. Dupuytren's fracture is common and was described by H. Dupuytren in 1819.
The mechanism of this fracture is a pronation-abduction fracture. The foot has a natural valgus position of 10° and is therefore more outwardly rotated in trauma. Due to the strength of the medial (deltoid) ligament, the medial ankle is hyperextended and the talus becomes valgus. The talus jams against the lateral malleolus and the ankle fractures with a tear of the anterior interosseous ligament, or, more commonly, both.
clinical picture
Dupuytren's fracture is usually accompanied by swelling of the ankle. External subluxation of the foot results in an abnormal valgus position of the foot, which is best seen from behind. There is acute tenderness of the medial malleolus, talus, and intercondylar syndesmosis on palpation. Active and passive movements of the joint are severely painful and restricted.
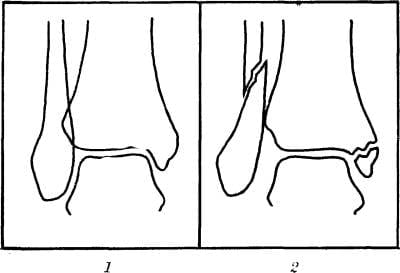
Figure 1: Anteroposterior radiograph of the ankle: 1 - normal (for comparison); 2 – in Dupuytren's fracture (fractures of the fibula and inner malleolus, tear of the lower interosseous syndesmosis).

Fig. 2. X-ray of ankle in Dupuytren's fracture: 1 - direct view (fracture of both ankles - arrows, external subluxation of foot); 2 - lateral view (arrow shows the external fracture line of the ankle).
In direct view, the fracture line of the medial ankle, usually in the fissure, and the lateral ankle at or above the fissure is visible. At the same time, a clear displacement of the fragments and a possible diastasis, ie a joint fork separation, is visible (Figures 1 and 2). A comparative analysis of anteroposterior radiographs (on the same film) of both ankles in the normal position or with symmetrical 27° internal rotation is of great importance for the diagnosis of a tear of the inferior intercondylar syndesmosis.
subluxation of the talus
Class B: Dislocation of the ankle bone after a fracture. If the overload continues after a femoral neck fracture, the ankle bone can snap into the fork of the ankle joint. This locks the foot in a hyperextension position while this mechanism is occurring. An even greater destructive overextension force is required for a posterior fracture.
These patients have one a history of Hyperextension with the foot locked in this position. Typical symptoms are severe pain, tenderness and swelling.
To detect this pathology pathologyA routine X-ray examination is usually sufficient.

Treatment of heel fracture dislocations
The emergency treatment includes administration of pain medication, elevation of the limb, and urgent referral to an orthopedist for repositioning. Late repositioning is associated with a high probability of skin necrosis and avascular necrosis.
In the latter is the development of avascular necrosis necrosistraumatic arthritis, skin necrosis and delayed healing.
sprains of the pelvis
heel bone sprains There are two types of dislocations: total talar dislocation and periarticular dislocation.
Total Total talar dislocation This second dislocation is fully disengaged from the ankle fork and rotated so that the inferior articular surface faces posterior and the head of the ankle bone is medial. Shepard introduced the term peritarsal dislocation to more accurately describe the dislocation of the talus from the surrounding joints (talonavicular joint, etc.) and the subtalar joint.
Peritarsal Dislocations can be divided into medial and lateral depending on the position of the foot in relation to the distal tibia. In the more common medial type, the femoral head is palpated externally.
The lateral periarticular dislocation is less common and the femoral head is directed medially and is usually palpable.
symptoms of a dislocation
Fortunately, the injury can be diagnosed as soon as it occurs. One of the first signs of injury is the distinctive grinding sound as the dislocation occurs. Secondary symptoms that indicate you should see a doctor include:
- Acute pain. The pain can vary depending on the severity of the dislocation. Grade 1-2 injuries cause discomfort when you try to move or lean your leg. Dislocations with a broken bone cause severe pain even at rest.
- hematoma and edema. Swelling usually occurs around the ankle and increases day by day after the injury. The more severe the injury, the more pronounced the swelling and discoloration.
- changes in foot position. A foot that is frozen in an unnatural position and won't reset is often a sign of a torn ligament.
- Crunch. When you try to move your foot, you may hear a cracking sound that indicates a sprained ankle.
If you experience any of the above symptoms, you should seek medical attention immediately. Only an experienced specialist can determine the nature of the injury and prescribe appropriate treatment.
First aid measures for a sprained ankle
Timely first aid treatment of injuries ensures that the consequences are minimized and the recovery time is shorter. Preventive measures immediately after a sprain include:
- Normalization of blood circulation. To do this, eliminate all factors that can adversely affect blood circulation. This includes tight shoes, tight socks or tights. If, at the time of the sprain, the injured person was wearing high-heeled shoes, e.g. B. boots, it is not advisable to take them off. Because if there has been a rupture, this can only aggravate the situation.
- Provide sedation. First, a pillow or bolster should be placed under the injured foot. Second, the ankle should be secured with a bandage or elastic bandage.
- relief of symptoms. The injured area should be iced to reduce the risk of severe swelling. Painkillers can be given for acute pain.
Even if first aid can temporarily improve the condition of the injured person, only a specialist is able to fully heal the injured limb. It is therefore advisable to consult a doctor immediately after the first aid.

A distinction is made between fractures of the femoral neck, the shaft, the head and the posterior process of the talus. These fractures are often combined not only with each other, but also with dislocations of parts of the talus or dislocations of the foot in the subtalar joint.
Two main mechanisms predominate in talus fractures. The first factor is the impact on the plantar surface. The second factor is twist. It is not uncommon for both fractures to be present and complement each other. These fractures are most common in motorcyclists. The fracture occurs when the motorcyclist's foot is on the footpeg - an accident, a severe impact of the footpeg on the sole of the foot. In motorists, the mechanism is similar, but the footrest is the pedal. These fractures also occur during sports, a fall from a great height or a failed jump. The patient feels severe pain. Sometimes there is visible deformation of the foot, especially with displaced fractures. Severe fractures are often open. X-rays and computed tomography (CT) are used for diagnosis.
With few exceptions, all thigh fractures are intra-articular. Also, no muscles are attached to the plate. This means that the nourishment of the cartilage (up to 70 percent of the body of the talus is covered by cartilage) is heavily dependent on the synovial fluid in which the talus literally 'swims'. Early movement is essential for synovial fluid circulation. Surgical treatment is therefore the priority for thigh fractures. Long-term immobilization is not acceptable here. Only surgery makes it possible to initiate early movement and thus ensure good nutrition of the plate.
A distinction is made between fractures of the femoral neck, the shaft, the head and the posterior calcaneal process. Often these fractures are combined not only with each other, but also with dislocation of part of the talus or dislocation of the foot at the subtalar joint.
The main treatment for heel bone fractures is surgery. Even non-dislocated fractures must be fixed with screws through skin punctures to allow early movement of the foot.
professionals in this field

Glazova Natalia Alekseevna

Torno Timur Eduardovich

Maxim Alexandrovich Vavilov
Doctor of medicine, orthopedist and traumatologist, President of the Russian Ponseti Society, staff member of the YSMU Department of Pediatric Surgery.
Our patients
Anastasia



Diagnosis: Congenital bilateral severe atypical clubfoot
Treating doctor: Maxim Vavilov
Miroslav



Diagnosis: Congenital bilateral severe clubfoot
Treating doctor: Maxim Vavilov
Alexander



Diagnosis: Congenital right-sided severe clubfoot
Treating doctor: Maxim Vavilov
Maria



Diagnosis: Congenital bilateral clubfoot
Treating doctor: Maxim Vavilov
Filipp



Diagnosis: Congenital bilateral clubfoot
description of the case
A 28-year-old young man was admitted to the emergency room at our Level I Trauma Center after suffering a serious injury to his left lower extremity in a fall from 40 feet. On admission he was hemodynamically stable. There was slight shortness of breath. A skin lesion in the left frontal cranial region and perivascular excitotoxicity on the left side were evident. He was conscious (GCS:15) and later found to have no neurosurgical trauma.
The entire left lower limb was externally rotated and the foot was swollen, tight and deformed, with a medially displaced hind foot and a supinated fore foot. The tibialis posterior and dorsalis pedis pulses of the limb were normal. The left elbow was deformed with a 2 cm open wound; the left wrist showed deformation and swelling. The radial pulse was weak with delayed capillary filling.
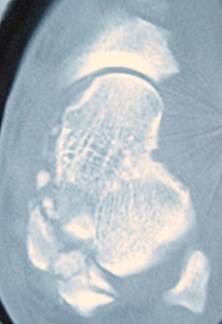
After a comprehensive clinical examination, X-rays were taken in the emergency room. Limb radiographs showed posterolateral dislocation of the left ulna, fracture of the distal epiphysis of the left radial bone, intercondylar and subcondylar fracture of the left humerus, and closed total dislocation of the calcaneus with an associated fracture of the elbow bone (Figures 1, 2, 3 ).


Chest x-ray showed interstitial pulmonary contusion, pneumothorax, and hemothorax. Pelvic X-ray showed a transverse fracture of the left pubic bone and CT scan revealed a stable sacral fracture on the contralateral side.
discussion
Complete dislocation of the talar bone from all three joints (tibial, subtalar, and talonavicular) is a rare injury resulting from high-energy trauma. This type of injury is thought to be a continuation of the subtalar dislocation as the force increases and progresses. Dislocation of the subtalar joint is the first stage of injury. As the force increases, the talonavicular joint becomes dislocated and finally the tibial joint becomes dislocated. The mechanism is considered to be excessive supination or pronation. Supination force leads to a lateral dislocation and pronation force to a medial dislocation. The purpose of closed reduction is to reduce the tibiofemoral joint. When the tibiofemoral joint is reduced, the other joints (subtalar and talonavicular) are reduced spontaneously. [5, 6]
In the present case, the injury mechanism is axial loading from a fall with or without a supination or pronation injury. Because of the high energy of injury, combinations of mechanisms are responsible and a precise isolated mechanism cannot be elucidated. Closed reduction was unsuccessful, the main cause being locking of the subtalar joint in the dislocated position and entrapment of the femoral neck between the flexor tendons. Open reduction via an anteromedial approach with displacement of the subtalar joint allowed easy reduction of the dislocation, and all other dislocations were subsequently reduced.
Due to the rupture of all thigh capsules and ligaments in this injury and the dependence of the femoral vasculature on these elements, avascular necrosis of the thigh is predictable in most cases. Although some investigators believe that avascular necrosis is an inevitable consequence of injury, there are case reports of complete dislocation of the talar bone without osteonecrosis. Restricted movement and osteoarthritis in each of the three joints are also foreseeable complications. [6-8]
Показания к вправлению вывиха голеностопного сустава.
Most ankle dislocations occur posteriorly or posteromedially and are associated with fractures of the ankle, distal fibula, and posterior tibia.
The ankle should be corrected soon after a closed ankle dislocation or dislocation with fracture is diagnosed. A neurovascular deficit or herniated dislocation associated with trauma where skin tension at the injury site threatens integrity requires immediate reduction.
Open dislocations require surgical treatment, but when an orthopedist is unavailable and neurological and vascular disorders are present, closed techniques with repositioning and splinting are performed as indirect treatments.
Contraindications for ankle sprains
There are no contraindications for closed ankle dislocations, even if they have not been orthopedically evaluated and treated. However, repositioning open dislocations without vascular lesions—when surgical intervention is required—may be better performed with thorough lavage in the operating room (rather than lavage in the emergency room) prior to repositioning.
Compression syndrome Compartment syndrome In compartment syndrome there is an increase in tissue pressure within the fascial space, which leads to the development of tissue ischemia. The first symptom is disproportionate pain. Read more (due to the soft tissue trauma and swelling from the primary injury) and joint damage that worsens with time to reduction. This complication is related to the injury itself, but can be prevented with timely reduction.
Most complications arise from the fracture itself—a dislocation.
Indications for ankle dislocation
Most ankle dislocations are posterior or posterior-medial and involve fractures of the talus, the distal aspect of the fibula, and the posterior aspect of the tibia.
The ankle should be corrected soon after a closed ankle dislocation or fracture dislocation is diagnosed. A neurovascular deficit or fracture dislocation associated with trauma where skin tension at the injury site threatens the integrity of the ankle requires immediate reduction.
Open dislocations require surgical treatment, but when an orthopedic surgeon is unavailable and neurological and vascular disorders are present, closed reduction techniques and splinting are performed as indirect treatments.
Contraindications for ankle dislocations
There is no contraindication for closed ankle dislocations, even if they have not been orthopedically evaluated and treated. However, reduction of open dislocations without vascular lesions—when surgical intervention is required—may be better achieved by careful lavage in the operating room (rather than lavage in the emergency department) prior to reduction.
Compartment syndrome In compartment syndrome, there is an increase in tissue pressure within the fascial space, which leads to the development of tissue ischemia. The first symptom is disproportionate pain. Read more (due to the soft tissue trauma and swelling from the primary injury) and joint damage, which worsens the longer the reduction lasts. This complication is related to the injury itself, but can be prevented with timely repositioning.
Most complications arise from the fracture itself—a dislocation.
Symptoms of an ankle dislocation
Patients often have symptoms associated with a dislocation, ranging from mild to severe. A minor dislocation does not usually cause major problems and athletes are often able to continue training or competing, while a serious injury may require hospital treatment. However, in order to avoid many problems and recurrence of the injury, you should not ignore the symptoms and consult an orthopedic sports doctor as soon as possible.
A sprained ankle is usually associated with ankle pain, which worsens with walking as the pressure on the injured ligaments increases. Another symptom is swelling (swelling) and bruising – this is quite common, although not in all cases.
A sprained ankle is graded on a 3-point scale based on the degree of tissue damage. Treatment of the injury depends on the extent of the damage.
What exactly is a sprained ankle?
The ankle joint is formed by the articular surfaces that include the distal end of the tibia and fibula and the talar block. Also, it includes the joint capsule, which strengthens the ligaments: on the medial side of the tibia and on the lateral side, the anterior fibular ligament, the posterior fibular ligament, and the femoral ligament. The joint capsule holds the bones that make up the joint and creates the right conditions for the joint to function by preventing the surrounding tissue from getting between the bones and retaining synovial fluid.
Ankle sprain (as a sprained ankle is commonly called) is actually a sprain or tear of an ankle ligament with damage to the joint capsule.
– The most common type of injury issupination (lateral sprain, inversion sprain) resulting in excessive mobility of the ankle. The sole of the foot rotates inward, damaging the lateral ligaments of the ankle.
- On the other hand, pronation Eversion (external rotation of the ankle) is less common but can be associated with a fracture. The sole of the foot is turned outward, damaging the tibial ligament of the ankle (medial side).
The most common injury is an anterior tibial ligament (ATFL) injury. Anterior tibial ligament (anterior talofibular ligament) tapeThe anterior talofibular ligament (ATFL) is a common injury. The anterior talofibular ligament is also the main stabilizer of the ankle. The most important ligament is therefore injured most often, and its injury is usually underestimated. As the name suggests, this ligament attaches to the anterior edge of the long bone and runs anteriorly and medially. The final attachment of the ligament is at the anterior edge of the lateral articular surface of the ankle block.
Treatment
Treatment of an old talus fracture with foot subluxation depends on how long it has been since the injury. If it has been less than two months since the injury, it is sometimes possible to repair a fixed ankle fracture with subluxation using conservative measures under local anesthesia. In other cases, only surgical treatment is possible.
The goal of surgical treatment is to eliminate excessive diastasis (diastasis is a tear in the intermetatarsal membrane between two bones, the tibia and fibula) in the intermetatarsal joint and restore the anatomy of the injured ankle. Percutaneous Ilizarov osteosynthesis is the best treatment option for long-term tears of the distal intercondylar syndesmosis. During the operation, the fragments are separated from each other, and sometimes individual pieces of bone and cartilage have to be excised. The anatomical structure of the joint is then restored and fixed in the correct position - osteosynthesis. The most common surgical treatment for isolated lateral malleolus fractures is the use of plates. Rear ankle fractures are most commonly fixed with screws. A combination of plates and compression screws is used for a double ankle fracture. Sometimes, when a long time has passed and the joint has become severely degenerated, ankle atrodesis (surgery to immobilize the joint) may need to be performed. In this case, the joint loses its function and is fixed at right angles.
complications
Complications of a protracted ankle fracture with foot subluxation arise when the fracture is not properly identified and inadequately treated.
Misdiagnosis of distal intertibial syndesmosis and recurrence of excessive diastasis in this joint during treatment, as a rule, leads to one of the most common and serious complications - chronic rupture of tibial syndesmosis (tibiofibular joint tear), which significantly reduces the function of the lower limbs even with fixed ankle fractures impaired.
prevention
To prevent a permanent ankle fracture with foot subluxation, any patient with an ankle injury needs early evaluation by a trauma surgeon. The patient must be examined radiographically, and an appropriate treatment tactic must be chosen. All fracture dislocations must be operated on in a timely manner.
One form of prevention to reduce the risk of ankle and ankle fractures in general is to train the leg muscles, which can strengthen the muscles and ligaments in the ankle to protect it from injury.
What questions should you ask your doctor?
How can I visually distinguish a sprained foot from a broken ankle?
How long does the cast have to stay in place after treating a broken ankle?
Tips for the patient
Since ankle fractures are very common in all active people (adolescents, athletes), one should be particularly careful with ankle injuries.
Read more:- Fracture of the heel bone.
- Diagram of a joint with and without a dislocation.
- The shaft of the heel bone.
- The lateral ankle is.
- Displacement fracture of the heel bone.
- pelvic bones.
- Lisfranc joint.
- tibia and fibula.
