Women suffer from patellofemoral arthrosis more often than men. This is due to their less stable hormonal balance.
- Dysplasia of the patellofemoral joint
- Possible causes
- What is a metatarsophalangeal fold?
- When can the metatarsophalangeal fold cause pain and discomfort?
- symptoms and diagnosis
- Current treatment approach
- symptoms of the disease
- Causes of metacarpal hypertrophy
- Which doctor should be consulted?
- Diagnosis of osteoarthritis of the patellofemoral joint.
- Treatment of patellofemoral arthritis
- Medication
- Mediopatellar folding syndrome
- dysplasia
- Fracture of the kneecap
- Osteoarthritis of the patellofemoral joint of the knee
- causes
- Symptoms and general characteristics
- Mechanism of pain development
- Symptoms of patellofemoral arthritis
- principles of treatment
Dysplasia of the patellofemoral joint
Patellofemoral joint dysplasia is a diagnosis that appears more and more frequently in doctors' reports every year. So let's try to get to the bottom of this fairly common but still misunderstood diagnosis.
It is a pathological condition characterized by certain abnormalities in the structure of bone tissue. These form the patella layer and the surface of the joint. This has an unhealthy effect on the cartilage and muscle fibers. The disease can be congenital or develop over the course of life. The congenital form arises in the uterus and can worsen during adolescence. It is usually diagnosed in the first year of life.
Possible causes
The exact causes of this condition are not known. Possible factors that may contribute to the development of dysplasia include:
– Bad maternal habits during pregnancy, especially in the first trimester;
– Malposition of the fetus in the uterus;
– mother’s stress or anxiety during pregnancy;
– Viral or infectious diseases in early pregnancy;
– A relatively poor diet during pregnancy with deficiencies in important vitamins and micronutrients;
– Genetic predisposition to dysplasia.
Note: Since the disease is very rare in older people, it is considered congenital.
What is a metatarsophalangeal fold?
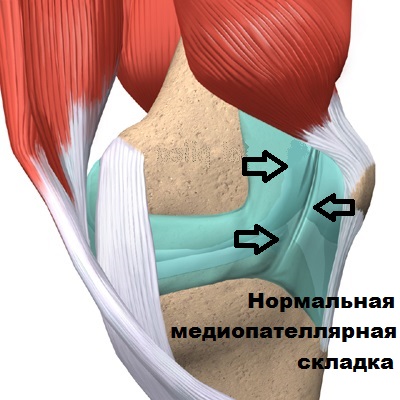
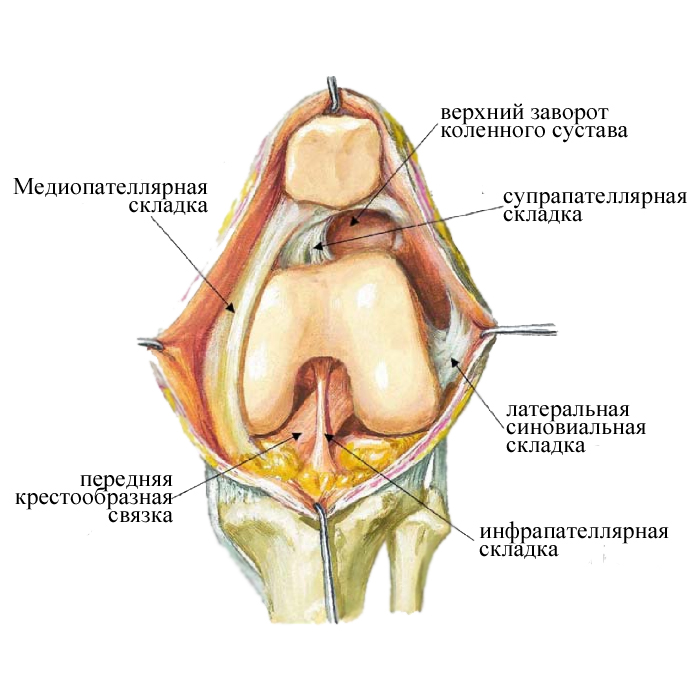
The metatarsophalangeal fold is the rudiment of the septum that separates the joint during the embryonic period. If for some reason the fold does not disappear during the embryonic period, it can also be detected in adulthood. The metatarsophalangeal fold occurs in 50 % of adults, but causes no symptoms in most.

The knee joint is contained in a type of waterproof bag called the joint capsule. The inside of the joint capsule is lined with a special membrane, the synovial membrane. The synovial membrane is a thin membrane that produces synovial fluid (synovial fluid) and is rich in blood vessels and nerves. The metatarsophalangeal fold looks like a tourniquet, or thickening of the synovial membrane that connects the kneecap to the femur.
When can the metatarsophalangeal fold cause pain and discomfort?
The metatarsal fold causes problems for the patient when it is inflamed and thickened. Inflammation can occur if the fold is irritated over a long period of time by certain repetitive movements in the knee joint. During running, cycling, and fitness activities, the knee joint is repeatedly flexed and extended. This activity causes the metatarsophalangeal joint crease to become inflamed and correspondingly enlarged. The thickened, swollen fold begins to resemble a stretched cord, which, when moving, touches and destroys the articular cartilage of the femoral condyle.
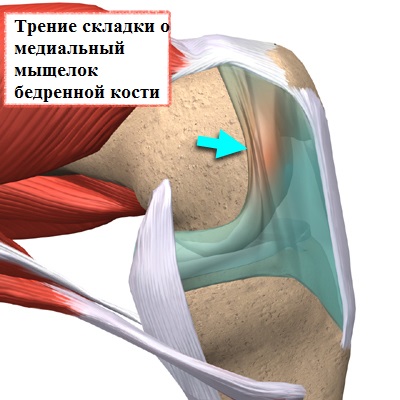
The hypertrophied fold also irritates the surrounding synovial membrane, which also becomes inflamed and scarred.
Sometimes medial inflammation occurs after a direct blow to the inner surface of the knee joint, such as: B. during a football game or a traffic accident.
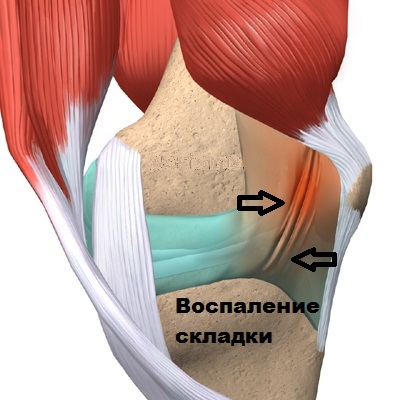
In some cases, long-term damage to the meniscus and anterior cruciate ligament results in synovitis, which causes swelling and the formation of thick, rough scars around the middle phalanx.
symptoms and diagnosis
The main symptom of patellofemoral syndrome is pain caused by provoking factors. The patient has difficulty locating the exact location of the pain. A crunching sound can be heard when the lower limbs move. This noise occurs when the cartilage is missing or thin and the bones of the joint begin to touch each other.
Patients note a subjective feeling of 'locking' in the knee joint and stiffness of the joint after prolonged extension of the bent leg. During examination, the orthopedist may detect a deviation from the normal biomechanical axis of the lower limbs, increased or decreased mobility of the knee joint, and hypotrophy of the quadriceps muscle of the thigh.

Doctors at Yusupov Hospital use X-ray, CT or MRI scans. In the early stages of the disease, when x-rays show no signs of cartilage or bone damage, ultrasound is an informative diagnostic method.
Current treatment approach
Doctors at Yusupov Hospital apply comprehensive conservative therapy aimed at eliminating the biomechanical and pathophysiological changes that lead to the development of patellar pain syndrome. The first stage of treatment is eliminating pain. The orthopedist prescribes non-steroidal anti-inflammatory drugs (Meloxicam, Nurofen, Rheumoxicam, etc.) and limits physical activity.
To eliminate the cause of the pain, the kneecap is repaired with a brace that holds the knee joint in place. For this purpose, an orthosis is used to hold the kneecap in place. Modern external orthoses make it possible to support the kneecap throughout the entire flexion and extension cycle. Treatment includes physiotherapy and physical therapy.
If conservative therapy does not work, orthopedic surgeons surgically remove the patellar collateral ligament. This allows the kneecap to return to its normal position. In severe cases, surgery may be necessary. The operation can be performed in two ways: through arthroscopy or through a lateral incision.
Patients are advised to be selective when choosing their sporting activities. After the operation, you can do swimming, slow jogging and Nordic walking. Football, volleyball, basketball, tennis and skiing are not recommended.
If you notice the first symptoms of patellar pain syndrome, call us. Timely treatment is a sure prevention of the progression of the disease and the development of disability.
symptoms of the disease
Shortly after a fall, a bruise, or a blow to the knee, a stabbing pain occurs in the joint. It occurs suddenly and usually when walking and is usually a stabbing pain. The pain decreases when the range of motion is reduced, but increases when you switch from walking to running or put weight on the injured leg. He is accompanied by:
Because of these symptoms, hypertrophy of the medial knee joint fold is often confused with other pathologies, for example, meniscus damage. Therefore, an accurate diagnosis can only be made on the basis of an instrumental examination. Inflammatory flatulence is often found in humans:
This is because your knee joint is regularly exposed to high levels of stress. It literally wears out.
Causes of metacarpal hypertrophy
Because the knee is heavily involved in human movement, it is one of the most stressed joints. Located between the femur and the kneecap, the metatarsophalangeal fold is a small thickening of the synovial membrane that lines the joint capsule. Overloading causes this fold to become trapped. It becomes inflamed and thickens. If this is not resolved:
The thickening hinders the movement of the individual parts of the joint and the load on them increases accordingly. Hypertrophy of the metatarsophalangeal joint fold of the big toe can be triggered by:
- a bruised knee;
- a blow to the knee flexor;
- prolonged intermittent running;
- uncontrolled fitness activities;
- long cycling.
A knee injury involves an impact on the metacarpophalangeal joint. Running, cycling and sports keep the knee joint in constant rhythmic movement, which causes swelling of the kneecap. In both cases, inflammation is inevitable.
Which doctor should be consulted?
If a sharp pain is felt in the knee when walking or running quickly, this indicates the development of pathology in the joint. To find out the cause of the problem, you should consult a doctor:
Diagnosis of osteoarthritis of the patellofemoral joint.
During the examination, the doctor checks the mobility and stability of the knee joint, examines it for fever or swelling, and determines whether it limps or not. The specialist will then examine the movement of the knee when the joint is flexed.
The doctor will also take a medical history. To this end, he asks several questions, among others
- after previous injuries and damage to the knee;
- the presence of swelling throughout the day;
- the mobility of the knee in the morning after waking up;
- Sensations in the joint when moving;
- the type of work and how long the knee problems have lasted.
To confirm the diagnosis, the doctor will refer the patient for further examinations:
- X-ray of the knee. The doctor will take a picture of the joint in flexion and extension. This way you can see the condition of cartilage and bones.
- MRI (magnetic resonance imaging). One of the most meaningful studies. It can help examine the condition of synovial fluid, meniscus, inflammatory and cancerous diseases of the knee.
- CT scan (computed tomography). Allows examination of the extent of bone and soft tissue damage.
- Urine and blood tests (general and biochemical). Essential for determining calcium levels and other important trace elements in the blood.
- arthroscopy. Two punctures are made in the knee and a sterile saline solution is injected through the arthroscope. The doctor then examines the structures of the knee through the chamber of the arthroscope.
- Ultrasound examination of the joint. It makes it possible to examine the condition of the tissue around the affected joint. The examination can detect the disease at an early stage.
These examinations are mandatory. They help rule out other diagnoses and get a more complete picture of the disease.
Suspicion of acute arthritis can be raised at home. The final diagnosis is made by the doctor after an examination and visual inspection.
Treatment of patellofemoral arthritis
Treatment of patellofemoral arthritis is based on correcting the load on the knee. The aim of therapy is to either stop the degeneration of the cartilage or slow down the destruction process.
Crunch in the joints – when to worry
Intra-articular hyaluronic acid injections
Medication
At the initial stage, the patient is prescribed non-steroidal anti-inflammatory drugs (Ibuprofen, Analgin, Diclofenac) or other painkillers. These reduce swelling and allow the knee to maintain a normal range of motion.
In grade 2 patellofemoral arthritis, the affected person is prescribed corticosteroid (hormone) injections into the affected joint. These include betamethasone, prednisolone, dipropane, etc. These drugs quickly relieve pain, but also have side effects. Corticosteroids have adverse effects on the skin and internal organs. Therefore, they are not sprayed more than 2-3 times a year.

Myorelaxants are prescribed to relieve muscle spasms in the thigh that occur as a result of inflammation. These include drotaverine, spasmomen and adiphenine.
Hyaluronic acid is prescribed when the synovial fluid in the joint is insufficient. It acts as a lubricant for the joint components, supports the cushioning properties of the cartilage and increases its trophicity.
At stage 3 of patellofemoral arthritis, chondroprotective injections (Ostenil, Sinvisk, Sinocrom) are prescribed. These are used after the inflammation has subsided. These preparations protect the cartilage from further damage, promote cartilage regeneration and relieve pain.
At any stage of patellofemoral arthritis, the patient can be prescribed calcium supplements and B vitamins. The former are needed to strengthen bone mass, the latter to eliminate pain and restore the functioning of the nervous system.
Mediopatellar folding syndrome

This is a rudiment (rudiment that has lost its function), a remnant of the intra-articular septum that all humans possessed during fetal development. It is only needed by humans during their development and is gradually 'absorbed' after birth. Sometimes this process is incomplete and a remnant of one of the membranes, called the metatarsophalangeal fold, remains in the knee joint.
Why did this happen to me?
According to official statistics, MPS occurs in 30 % of people, but it is worth noting that it is much more common in people of the Mongoloid race. The wrinkle is the result of a genetic predisposition, and no external factors affect the likelihood of its formation.
What is Metatarsophalangeal Fold Syndrome?
It is a pain syndrome in the knee joint caused by inflammation of the fold. As already mentioned, 30 % of people have a metatarsophalangeal joint crease, but this does not mean that it necessarily becomes inflamed. That depends on the way of life a person leads. Often, sports that put a lot of strain on the knees (volleyball, basketball, hockey, etc.), viral infections and jobs that require standing on your feet for a long time lead to inflammation of the fold. Because MPS most commonly occurs in both knee joints, the pain can occur intermittently and lead to systemic diagnoses such as rheumatoid arthritis.
How does the syndrome manifest itself?
Pain in the front of the knee joints, occasional 'popping', pain after sitting for long periods and a feeling of 'heaviness' in the knee joint are common symptoms of this condition. As a rule, anti-inflammatory drugs and ointments have a positive effect, but all these complaints return after further stress.
dysplasia
In dysplasia, the shape of the articular surfaces of the kneecap and the pulley groove are not congruent. In such cases, the articular cartilage is subjected to greater strain when the knee joint moves and wears out more quickly.

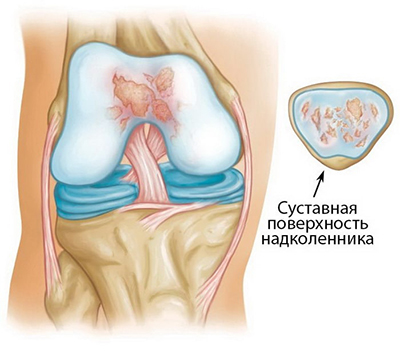
X-ray image of the patellofemoral joints showing dysplasia that has led to the development of significant patellofemoral arthritis. On the left side the joint space has completely disappeared. On the right side, the patellofemoral sulcus is severely distorted.
Fracture of the kneecap
When a kneecap fracture occurs, it is not uncommon for the articular cartilage that protects the back surface of the kneecap to be damaged. In such cases, after the fracture has healed, the joint surface is no longer as smooth as it used to be. The friction between the articular surfaces of the kneecap and the pulley groove increases and eventually leads to the development of osteoarthritis at this point.
The main symptom of kneecap joint inflammation is pain. The patellofemoral joint is part of the front part of the knee joint, so if you have patellofemoral joint disease, pain occurs in the front part of the knee joint. The pain can be annoying at rest and when the knee joint is not moving. However, most often they occur during certain activities that are accompanied by increased pressure of the patella on the corresponding articular surface of the femoral condyle: sitting on your knees, squatting, climbing up or down stairs, getting up from a low chair.
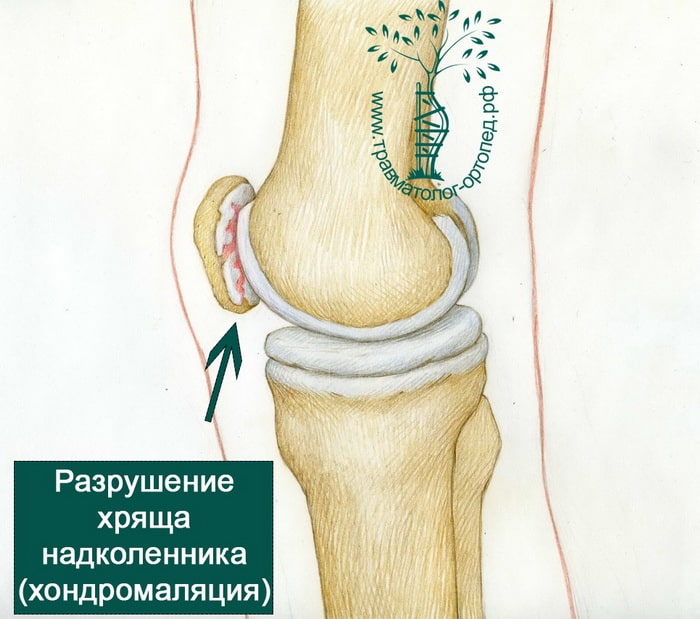
You may also feel a characteristic crunching sensation in the area of the patellofemoral joint, called crepitus. Sometimes this crunching sound is accompanied by pain and can even be heard in the distance. As the disease progresses, the patellar joint may become blocked or 'stuck' in a certain position when the knee joint is extended.
Treatment for patellofemoral arthritis is generally similar to that for osteoarthritis of the knee. Most causes of this disease can be easily controlled without surgery. The components of conservative treatment are:
Nonsteroidal anti-inflammatory drugs (NSAIDs). Taking medications such as aspirin or ibuprofen can reduce pain and swelling.
Physical movement. Regular physical activity helps improve knee joint mobility and strengthens the muscles around the joint. Patients with patellofemoral arthritis should try to avoid physical activities that place greater stress on the front part of the knee joint, such as: B. squatting. If you do strenuous exercise regularly, you can reduce the intensity of the exercises to reduce the stress on the knee joint and reduce the severity of pain and swelling. Walking and swimming are good options for low-intensity exercise.
Osteoarthritis of the patellofemoral joint of the knee
Detecting this disease is relatively easy. In addition to the pain, osteoarthritis of the kneecap joint is characterized by a number of other symptoms. Here are the most important of them:
- Limited mobility due to discomfort in the affected joint;
- Discomfort that is aggravated by sitting in one position for a long time, especially in a hunched position;
- Pain in the joint with additional stress (jumping, squatting, running, climbing stairs).
Older people and athletes are the most commonly affected. In recent years, the disease has also appeared in athletes and fitness enthusiasts. Patellofemoral syndrome is also promoted by previous knee injuries, especially if they have not yet fully healed.
If you experience any of the above symptoms, you should consult your doctor. However, before you make an appointment, you can do a self-diagnosis online. It is freely available on the Internet. With this practical test you can shorten the list of possible causes of pain. However, it does not replace a visit to a specialist. Rather, you can only get an idea of the severity of your symptoms and assess the condition of your body.
causes
This syndrome often affects the knee joints. It affects all age groups: young and old people alike. Patellofemoral syndrome has the following causes, among others.
- Cartilage deformations resulting from congenital or acquired injuries;
- abnormal development of the knee joint;
- Wear and tear of cartilage tissue as a result of prolonged stress.
Inflammation of the kneecap also occurs against the background of other diseases. For example, in the case of valgus or varus misalignment of the joint or instability of the kneecap. The inflammatory process develops in the groove under the kneecap. This is accompanied by severe pain in the affected joint. If the syndrome is not caused by other diseases, it usually resolves spontaneously. However, if the pain persists, it should not be ignored.
Symptoms and general characteristics

Patellofemoral pain is pain in the kneecap area and can occur around, behind, or below the knee. The symptoms usually occur or worsen with physical exertion and are particularly common in certain positions of the lower limbs. Kneecap pain usually occurs when squatting and climbing and descending stairs. The symptoms can also occur when sitting for long periods of time.
Other signs of pathology include:
- Stiffness in the knee, which is particularly noticeable after prolonged extension of the limb.
- Abnormal alignment of the lower leg.
- Excessive or insufficient mobility of the knee joint.
- Hypotrophy (reduction in size) of the quadriceps femoris muscle.
- Intermittent joint effusion due to overloading.
- Cracking noises in the knee joint.
Patellofemoral syndrome can occur in one or both knees. The severity of the symptoms can vary; Most often, patients complain of a deep, dull pain that is not clearly localized.
Mechanism of pain development
Patellar pain is caused by a displacement of the kneecap, causing the kneecap to move differently than the outside of the limb. This displacement causes overstretching of the structure that supports the kneecap, causing discomfort and pain.
If this condition is not corrected in a timely manner, patellar pain syndrome leads to changes in the neuromuscular structure of the affected lower extremity. Prolonged microtrauma and accompanying inflammation reduce the elasticity of the ligaments that stabilize the kneecap. As a result, the normal movement of the limb is impaired and the muscle structures activate compensatory mechanisms. This can lead to accelerated destruction of the cartilage tissue on the articular surfaces.
Doctors ensure that the risk of developing patellar pain increases with:
- Valgus alignment of the knee joint.
- weakened thigh muscles.
- Incorrect alignment of the foot.
- Imbalance of muscle-tendon groups.
- Contractures of the thigh muscles.
- Overload during sports training.
Recognizing the factors that contribute to patellar pain syndrome can help you achieve a relatively quick recovery and reduce the risk of the problem recurring.
Symptoms of patellofemoral arthritis

Patellofemoral arthritis is a gradually progressive disease that can become disabling if not treated promptly.
There are usually few or no symptoms in the early stages of the disease. Depending on the severity of the knee joint lesions, three stages are distinguished.
The first stage is characterized by mild destruction of the articular cartilage, which is difficult to detect even with X-rays. Clinically, this pathology is manifested by short-term, low-intensity knee pain during increased physical stress, which disappears after rest.
In the second stage of osteoarthritis of the knee, a clear and extensive degenerative-dystrophic change in the cartilage can be seen on the X-ray. The patient complains of severe pain in the knee that occurs when jogging, climbing stairs, standing up after sitting for a long time, etc. In some cases, a slight limp occurs when walking long distances. However, there is no pain when at rest.
The third stage is reached when there are extensive pathological changes in the articular cartilage and it is completely destroyed in some areas. The clinical picture includes knee pain both during exercise and at rest. The mobility of the knee joint is limited and it is externally deformed. In advanced stages it is virtually impossible to move the knee.
principles of treatment

In the first and second stages of osteoarthritis, conservative treatment may be the best option.
First of all, with this pathological process it is necessary to relieve the knee joint as much as possible. This includes avoiding sports training, wearing orthopedic shoes and special bandages or knee pads.
Pharmacological treatment consists of taking nonsteroidal anti-inflammatory drugs to suppress pain. If pain is very severe, intra-articular injections of glucocorticosteroids are administered.
Glucosamine derivatives have a good effect. In 2018, researchers from Kazan State Medical University published a paper in which they found that topical administration of glucosamine derivatives effectively inhibits the development of patellar arthrosis.
Surgical treatment is indicated for third-degree disease.
Read more:- The lateral dislocation is.
- How much does knee surgery cost?.
- Rupture of the medial collateral ligament.
- How to wear a knee brace for osteoarthritis.
- Knee splint for knee arthrosis.
- Axis of rotation of the knee joint.
- The sit bones.
- tibial ligaments.
