In humans, it is the legs that provide the main support. Many biologists and medical professionals say mankind has paid the price for dealing with joint disease.
- Leg pain from hip to knee
- causes of pain
- Main causes of numbness in legs
- Etiology by location of numbness
- Conclusions
- Code to embed the video
- Ideas
- muscles and tendons
- vascular supply
- Functions of the lower limbs
- Who is at risk and why
- What you should know
- How gangrene develops in diabetes
- The pathogenesis of lower limb gangrene: a comparison of the different forms
- What is the risk of a hematoma?
- types of hematomas
- diagnosis of the injury
- treatment of bruises
- The following symptoms should be noted:
- treatment of hematomas
Leg pain from hip to knee
When your leg hurts from the hip to the knee, it's not always possible to say that the source of the discomfort is in the limb. The pain can range in severity from mild to tense to acute. Gait disturbances and stiffness in movement can also occur.
The pain can affect the entire thigh or just the front.
The most common type of pain is pain accompanied by a slight numbness. He occurs intermittently and disappears without medication at the beginning of the development of pathology. Severe abnormalities can cause pain even at rest.
Acute pain is a sign of problems in the body.
Pain can be caused by the following structural elements of the hip:
causes of pain
Leg pain can be caused by a variety of factors. This includes:
- Injuries (fractures, sprains, dislocations, etc.)
- compressed sciatic nerve;
- fatigue, overexertion (leg pain – in this case, the discomfort often goes away on its own);
- Physical reaction to weather conditions;
- pregnancy (increased pressure on the leg joints);
- obesity (increased load on the joints);
- Cancerous tumors (sarcoma, leukemia, metastases)
- inflammatory conditions caused by infections (abscesses, lymphadenitis)
- Venous and vascular anomalies of the hip (varicose veins, thrombophlebitis, phlebothrombosis);
- Diseases of the nervous system (intervertebral hernias, neuritis, thrombosis).
Main causes of numbness in legs
Main causes that cause dangerous numbness:
- diseases of the spine. Compression of nerve endings by spinal fractures, osteochondrosis.
- Systemic diseases: diabetes, cancer and others;
- Arthritis. Joint deformities affecting nerve conduction.
- pregnant women. Excess fluid in the body in women, increased load on the spinal apparatus.
- tunnel syndrome. Condition in people who perform monotonous activities.
- Circulatory disorders (Raynaud's syndrome). Sudden attacks with acute, severe pain.
- Lack of vitamins or minerals in the body. Systematic abstinence from food, unbalanced diet, poor nutrient absorption.
Etiology by location of numbness
The location of the numbness can give an indication of the possible cause of the numbness.
| location of numbness | Possible illness |
|---|---|
| area of the thigh | Intervertebral prolapse of the lumbar spine Mild disc herniation complicated by osteochondrosis Spinal stenosis Inflammation of the sciatic nerve radiculitis |
| From the hip to the knee | vitamin deficiency High body weight strenuous physical activity femoral head necrosis |
| calves | thrombophlebitis varicose vein disease Potassium, sodium or magnesium deficiency CNS abnormalities passive lifestyle |
| From the knee to the foot | intervertebral hernia Rheumatoid arthritis Disorders of the peripheral nervous system of the lower limbs Raynaud's Syndrome |
| Pain in foot and ankle | intervertebral fractures presence of cancer Poor blood supply to the brain spondylosis diabetes Raynaud's Syndrome |
| Numbness in left leg | Nerve root compression in the groin osteochondrosis multiple sclerosis migraine Rheumatoid arthritis Malignant tumor diabetes Vitamin D deficiency |
| Nausea in right leg | thrombosis varicose veins post-traumatic stress Lumbar osteochondrosis lumbar sciatica |
Let's take a closer look at some individual cases.

The success of the treatment depends to 90 % on the doctor's experience and qualifications.
Conclusions
Remember that in amateur sports, there is no point in memorizing the names of all of a person's leg muscles; this is more important in the medical field. However, knowing the basic functions of the muscles and their structure can increase the effectiveness of a workout many times over. This is true for beginners who have just joined a gym, as well as for athletes who have been training for years.

The easiest way to determine the ideal leg shape and joint structure is to look at the distance between the thighs, but there are many pitfalls. First: width

What men and women have in common when it comes to training is lower body development. While men want to build strong muscles through their training, women need tight muscles.

Like the body as a whole, the legs should be developed harmoniously, none of the major muscles should lag behind in development, and the same goes for the hamstrings.

Training your calves at home is no easy task, especially when your shins are a retarded body part and develop little no matter how you train.

Code to embed the video
Ideas
The player will start automatically (if technically possible) if it is visible on the page
The size of the player is automatically adjusted to the size of the page. Image format – 16×9
The player will play a video from the playlist when the selected video is played
Last summer, officials at the Guardianship Service of the South Ural region in the Chelyabinsk region gave multiple mother Yekaterina Odegova a second chance after witnesses found her three-year-old son sleeping by the roadside. However, Ekaterina herself was not ready to give the child a second chance... On January 27, the infant was burned to death in a fire while the mother was rescuing other children.
Neighbors and friends are convinced that it is not an accident but a tragic pattern of a neglecting mother's lifestyle.
Today in the studio of the show Woman/Man we will find out all the circumstances of Vitalik Odegov's terrible death. Why haven't the care authorities responded to the constant complaints from Ekaterina's neighbors and relatives? And will the mother now get a second chance for the criminal negligence that led to the child's death?
muscles and tendons
The lower limbs of man (their muscles are numerous and quite strong) are subjected to heavy loads. The muscles of the thigh are quite large. There are 3 muscle groups: the anterior, posterior and middle thigh muscles. The strongest group is the front. This is where the famous, powerful quadriceps muscle is located.
The lower leg also has three muscle groups. These are the anterior, posterior, and lateral shin muscles. The rear group is the stronger. Therefore, it is in turn divided into a superficial and a deep layer. There are no strong muscles on the medial surface of the tibia. Instead, synovial capsules are found here.
The muscles of the lower leg are numerous. They are very similar to the structure of the hand, only here it is less complex because the foot has lost its grasping function in the course of evolution.
The muscles and tendons of the human lower limbs are most prone to bruises, tears and other injuries. Inflammatory diseases are extremely rare.
vascular supply
The lower extremity is supplied with arterial blood from the pelvis of the femoral artery. It originates as a branch of the external iliac artery. The vessel described is very large, so injuries to it can be fatal.
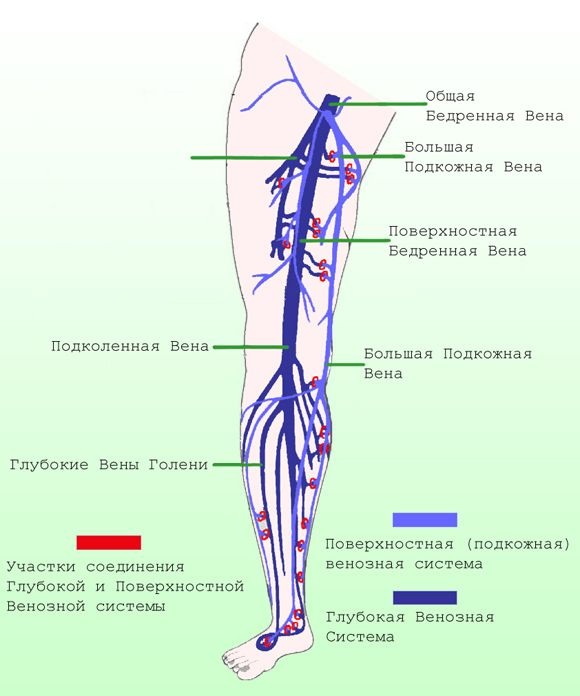
The femoral artery originates at the front of the thigh. Its largest branch is called the deep femoral artery. On the back of the thigh, directly at the level of the femoral fossa, the popliteal artery branches off from the femoral artery.
It supplies the knee joint and the muscles of the lower leg with nutrients. Their branches, in turn, pass into the anterior and posterior tibial arteries. In the foot, these arteries form vascular arches that anastomose with each other, a protective factor against critical ischemia.
Blood flows from the heart to the peripheral tissues (muscles, joints) through arteries and from the tissues to the heart through veins. There are only 2 superficial veins: the small and the large great saphenous vein. The deep veins accompany the arteries of the same name. This is how the blood travels to the heart through the inferior vena cava.
Human lower limbs (the muscles in this area are very well developed) require a high metabolism. A distinctive feature of the veins of the lower limbs is the very high pressure on the valve apparatus.
Because in order to 'pump' the blood from the bottom up while overcoming gravity, a well-developed muscle layer is required. The veins of the lower limbs are particularly prone to varicose veins.
Functions of the lower limbs
The human lower limbs have a support and movement function. Thanks to the well-coordinated work of joints, ligaments and muscle connections, they cushion the movements of the body when walking, running or jumping.
The work of the skeleton, joints, muscles, nerve endings and circulatory system of the lower limbs contributes to the ability of a person to move in an upright position. And walking upright is the most important function of the legs.
You already know that the skeleton of the lower limbs is made up of the bones of the hip, tibia, and foot. The musculature is divided into the gluteus medius, the muscles of the front and back of the thigh, thigh and foot. The blood supply and innervation ensure nutrition and proper metabolism.
Who is at risk and why
Risk factors for atherosclerosis in the lower limbs are no different from risk factors for other areas of the lesions. So people are still particularly at risk:
- smoker,
- High blood pressure,
- who lead a sedentary lifestyle
- Obesity,
- high cholesterol,
- vascular' inheritance (stroke, heart attack, atherosclerosis)
- and an age of over 50 years.
According to modern concepts, the accumulation of cholesterol in the vascular wall is a consequence of existing vascular damage. These are favored by high blood pressure and the vasoconstrictive effect of cigarettes.
'Bad' cholesterol is delivered to the site of existing tears in the microvascular wall to 'mend' the damage. However, when there is too much bad cholesterol, instead of patches, atherosclerotic plaques form.
Contrary to popular belief, excess cholesterol has little to do with fatty foods. It is the result of impaired lipid and carbohydrate metabolism (obesity, lack of exercise, diabetes, hypothyroidism and other diseases), reduced levels of sex hormones and liver disease (the site of cholesterol synthesis).
It turns out that the age-related risks are due to the hormonal background, liver disease and age-related vascular changes (fragility of the vascular wall due to impaired collagen and elastin synthesis). And disorders of lipid metabolism, smoking and high blood pressure only accelerate the process of vascular degradation.
What you should know
Given the above risk factors, atherosclerosis can appear as early as 30 years of age or even earlier. And to catch the problem early, all you have to do is be 'on guard':
As well as the ultra-sensitive C-reactive protein (the earliest, still 'pre-cholesterol', marker for vascular damage).
Clinical Laboratory Diagnostician, Oncologist, Consultant Scientist KDL Laboratory. 15 years of experience
How gangrene develops in diabetes
Diabetes disrupts blood microcirculation and causes neurotrophic changes. Diabetic gangrene is a complication of diabetic foot disease. 10-15 % of diabetics develop permanent sores on their feet. Footwear, calluses, dry skin, and increased pressure on the limbs due to weight gain lead to microtrauma, followed by dermatitis and ulceration. Nerve damage and ischemia in diabetics significantly increase the risk of necrosis, and the prognosis is unfavorable - the affected limb often has to be amputated, otherwise there is a high risk of sepsis and death. Diabetic foot and gangrene are 10 times more common in people with diabetes2 than in people with diabetes1.
How do you recognize diabetic foot syndrome?
- The limbs lose sensitivity.
- The hair on the legs begins to fall out.
- The appearance of the foot changes: pigmentation, pallor and congestion appear.
- The nails become brittle and darken, which is due to bleeding under the nail plate.
- The skin becomes dry and scaly.
- The shape of the foot changes.
- Wounds heal slowly and leave stains after healing.
- Feet and shins become cold and unresponsive to touch, cold, heat, pain, and other stimuli.
- Ulcers form, which are often painless.
- In later stages, dry or wet gangrene occurs.
To reduce the risk, diabetics should have their blood sugar levels monitored constantly, choose shoe size carefully (insole size if sensitivity is reduced and it is not known whether the shoes fit or not), do not walk without socks to avoid cuts and insect bites . Don't get rid of corns and avoid burns and exposure to cold. Check your feet daily for damage. If vision is impaired, it is advisable to involve relatives in the study.
The pathogenesis of lower limb gangrene: a comparison of the different forms
Dry gangrene does not develop so quickly, but one should not underestimate this form. The disease can progress to a wet form, which significantly worsens the prognosis.
- The skin darkens, the limb becomes dry and has less volume than the unaffected limb.
- There is no pulse in the vessels.
- The boundary between necrosis and healthy tissue can be clearly seen.
- The finger can fall off: the body rids itself of the dead tissue in this way.
- The general condition is normal: no fever, no blood poisoning. Infection does not enter the body.
- The limb swells, turns red, then darkens.
- Healthy and diseased tissue cannot be clearly distinguished.
- The foot gets cold.
- Blood pressure rises.
- The patient's condition is severe: toxins enter the general bloodstream, which can lead to an unfavorable outcome.
Pain is observed in both forms. The exception is neuronal death, e.g. B. in diabetes, when the patient is restricted in his mobility, but does not complain of pain. The life-threatening gas gangrene is critical when the wet form is complicated by the attachment of an infection. The limb rapidly decomposes, giving off an unpleasant odor, and gas builds up under the skin.
What is the risk of a hematoma?
A hematoma – is a small pool of blood in an injured organ, tissue or muscle caused by the rupture of blood vessels. It is caused by bruises, bruises, vascular disease, or certain prescription medications.
The bleeding can be small or large and cause compression of internal organs. Some people may bruise the skin from even the slightest touch. For others, they are less common, but a severe impact can cause significant internal bleeding.
Extensive hematomas can cause various complications. Often hematomas begin to compress various nerves or large vessels. In such cases, hematomas must be treated in a medical institution.
types of hematomas
Depending on the localization, the following types of hematoma are distinguished:
intramuscular i Intramuscular and subcutaneous Hematomas have the same symptoms and are generally not harmful. As a rule, these formations resolve spontaneously and normally. However, sometimes they persist for a long time and interfere with the normal functioning of the surrounding organs.
Subdural hematoma (subserous hematoma) – is bleeding located in the chest or abdomen. When it occurs, specialist treatment and surgical intervention is required.
Cerebral hematoma (brain bruise) – is one of the most dangerous forms. The accumulation of blood in the cranial cavity can cause compression of the brain and swelling and damage to brain tissue.
Any head injury can lead to serious consequences! Therefore, urgent consultation of specialists is required.


diagnosis of the injury
Visual inspection of the injury site and collection of medical history are the first step to medical care. If the injury is severe, an X-ray may be taken.
If internal organs are suspected, an ultrasound scan or an MRI can be performed. Blood and urine tests may also be required.
treatment of bruises
First aid for bruised limbs begins with a thorough examination of the bruised area (flexion and extension of the arms and legs). In the case of serious injuries (before examination by a doctor), the injured limb should be immobilized.
If you have a bruise on your chest, head or abdomen Lay the injured person on a flat surface, apply a cold compress and immediately call an ambulance. Do not take painkillers yourself so that you do not miss the moment of exacerbation.
The following symptoms should be noted:
- Appearance of weakness and loss of consciousness (with a head bruise it is important to exclude intracranial hematoma);
- severe pain (this may indicate trauma to internal organs or a fracture),
- shortness of breath, blood in the urine (possible internal bleeding).
treatment of hematomas
The main treatment for bruises is usually to treat hematomas. A cold compress is placed on the bruised area to stop the bleeding. The cold constricts the blood vessels and stops the bleeding.
It should be noted that cold is only effective for the first 12 hours after injury. On the second day, the best treatment for a bruise (and a cure for a hematoma) is a warm compress, which along with physical therapy, will help stop the bleeding.
Hospital treatment for a hematoma may consist of puncturing the skin at the site of the injury and removing the accumulated blood.
Read more:- The parts of the human leg are named.
- What parts of the leg are called.
- Why amputate legs for diabetes?.
- Ligaments of the human leg.
- Diabetic foot ulcers.
- Photo of the right leg.
- The reamputation is.
- Indications for amputation.
