the injured spot. These processes increase swelling and inflammation.

- Causes of ankle ligament tears
- Types of ligament tears
- Causes of torn ligaments in the foot and ankle
- Diagnosis of torn ligaments in the foot and ankle in the clinic
- exercise packs
- Anterior cruciate ligament (anterior cruciate ligament)
- Anterior cruciate ligament (ventral ligament)
- Ulnar collateral ligament
- practice principles.
- Will there be any consequences?
- Treatment
- Anatomy of the ankle ligaments.
- Factors that increase the risk of an ankle injury:
- Prevention of torn ligaments during sports:
- Symptoms of a ruptured ligament
- Diagnosis of torn ligaments
- SURGICAL TREATMENT
- RESULTS OF SURGICAL TREATMENT
- Symptoms of ankle ligament injuries
- Treatment of ankle ligament injuries
Causes of ankle ligament tears
A ligament tear can result from a jump, a fall, an unphysiological flexion of the extremity during sport or an impact. Football players, track and field athletes, gymnasts, basketball players and skiers often suffer such injuries. Domestic and sports injuries usually involve isolated ligament tears.
In rare cases Cause of the joint ligament tear In rare cases, joint ligament tears occur in a car accident. They are associated with fractures of the extremities, pelvis, blunt abdominal trauma, chest trauma, head trauma, and other injuries.
To understand why a tear occurs, it is important to know what ligaments are.
They are dense structures with connective tissue at the core. Ligaments are like ligaments or flat plates and connect individual bones and organs together.
Depending on the specific site of attachment, ligaments direct or restrict movement in the joint or strengthen the joint. They ensure that the joint surfaces are congruent and have a constraining function. Depending on their primary function, they are supporting, leading or inhibiting.
The large joints of the legs (knees and ankles) are particularly stressed. Therefore, strains often occur in these areas, even if the joints are sufficiently strong.
Injuries can also occur in other joints: shoulder, wrist and hip.
Types of ligament tears
There are two main types of ligament tears There are two main types of ligament tears:
On the side of Total loss of the ligament The bands are completely separated into two parts. Virtually all ligament fibers are damaged. This type of tear also means that the ligament has separated from its attachment point.
At the partial tear Several fibers of the ligament are damaged. In such cases, a 'sprain' is diagnosed. A partial tear of the joint ligament does not lead to a loss of function of the ligament.
The cause of a sprain or torn ligament is caused by extreme stress. Although the band is very strong, it is not flexible enough. This means that overstretching the ligament can cause its fibers to tear.
The extent of the crack influences the type of crack. A specialist can diagnose a patient with a partial or complete tear or classify the injury. Grades 1 and 2 indicate a partial tear and grade 3 a complete tear.
Types of ligament tears Torn ligaments in a joint The types of ligament tears also differ depending on the cause
- Traumatic ligament tears occur due to trauma.
- Degenerative ligament tears – Injuries occur due to wear and tear of ligaments and tendons. These injuries are more likely to occur in patients over 40 years old.
Causes of torn ligaments in the foot and ankle
This injury usually occurs in the winter months when the foot twists on icy steps or flat surfaces. It can also be caused by jumping from a height or other movements.
Factors that increase the risk of injury include:
- overweight. Excess weight increases the constant strain on joints and ligaments.
- Metabolism disorders. Such diseases cause ligaments and joints to lose their mobility.
- Age-related changes. These inevitably occur in the musculoskeletal system due to wear and tear on the tissue.
- previous trauma.
- Congenital deformities.
- Wearing uncomfortable footwear (including high-heeled shoes).
Diagnosis of torn ligaments in the foot and ankle in the clinic
An experienced traumatologist can make the diagnosis after reviewing the patient's complaints, medical history and objective examination. When the front ligaments are torn, the foot moves forward freely. If the lateral ligaments are torn, the lateral mobility of the foot is increased. The examination is carried out by a trauma surgeon in comparison to a healthy joint.
Our doctors have all the necessary skills and knowledge to make a quick diagnosis. If necessary, they recommend an instrumental examination.
exercise packs
LFK is a whole science divided into small subsections. This means that each injury has its own healing complex. There are several main rupture sites and exercises for these:
- Rehabilitation after a lanyard rupture. If the acromioclavicular joint is injured, gymnastics is usually started in the second week. The exercises should be carried out until a slight sensation of pain occurs. When lying down, slowly stretch your arms to 90 degrees, while standing, rotate your arms and raise your limbs straight.
- Rehabilitation of a torn cruciate ligament in the knee. In the initial phase of rehabilitation, it is advisable to sit or lie down so as not to put any strain on the painful joint. It is necessary to bend the injured leg at the knee, tense the hip muscles, sit on an elevation and walk with light contact with the ground. To increase the load, you can do half squats, hold onto the rail, roll the load from heel to toe and vice versa, or roll the ball on the floor.
Danger!!! Remember to keep the knee joint slightly bent to avoid overexertion.
Anterior cruciate ligament (anterior cruciate ligament)
Possible exercise sequences for a torn anterior cruciate ligament:
Anterior cruciate ligament (ventral ligament)
Exercises for a rupture of the posterior cruciate ligament:
Ulnar collateral ligament
Exercises for problems with the ulnar collateral ligament:
practice principles.
Failure to perform an exercise program correctly results in lengthy rehabilitation, distorted fusion, and sometimes recurrent ruptures. To avoid such consequences, a few practice rules must be followed:
- The exercise program in rehabilitation is drawn up by the treating doctor and must be carried out step by step and without errors. Self-supplementation is only possible with the consent of a specialist.
- Each exercise should be performed until a slight pain is felt. There should be no acute discomfort associated with the activity. If the load appears too high, the exercise or the entire workout should be stopped.
- A simple warm-up is recommended for best results. In difficult cases, a simple heating pad can help warm up the necessary muscles. This is particularly useful in the rehabilitation of a tear in the anterior cruciate ligament tendon in the knee.
- It is advisable not to deviate from the schedule if possible. Therapeutic practice favors consistency. If it is not possible to visit a practice room, an easier variant at home is recommended. Be sure to inform your doctor and seek individual advice.
- It is also important to pay attention to good breathing. Cells that are supplied with the right amount of oxygen recover faster. Synchronous breathing increases the body's endurance and allows you to gracefully endure the exercise from start to finish. Breathing exercises are an indispensable part of rehabilitation after shoulder ligament rupture surgery. In this case, disturbed breathing leads to an unpleasant stinging feeling.
- Despite the individual approach for each patient, it is advisable to perform exercises in groups. This helps raise overall tone and mood and helps learn tasks faster.
Will there be any consequences?
Many people who have suffered an injury worry that they will not be able to recover properly. However, doctors say that rehabilitation is quite possible. 'If the patient has followed the specialist's advice and followed all the recommendations, he will gradually return to a normal lifestyle,' says an orthopedist. – says an orthopedist and trauma surgeon.
So, the key to a successful recovery lies in proper first aid and detailed treatment recommended by the specialist.
Because there are contraindications. The doctor's advice should be sought.
Treatment
First aid for ligament and tendon tears and standard treatment for all tears includes the following measures
- absolute calm;
- Cold;
- compression of the limb, which is applied with a bandage;
- elevation of the limb;
- In case of severe pain, administration of analgesics.
For Grade I, early mobilization of the injured limb is most effective for the patient.
For moderate grade II injuries, immobilization is performed for several days with a sling or bandage.
Immobilization for up to several weeks is recommended for severe Grade II injuries and multiple Grade III wounds. In addition to a sling or bandage, a plaster cast can be applied.
Grade III tears are usually treated surgically (e.g., a tear of the supraspinatus tendon).
Anatomy of the ankle ligaments.
The ankle is a complex intermediate joint between the tibia (fibula and tibia) and the foot (about 27 bones) with a range of motion of 63 to 66 degrees. Slight lateral movements are possible during flexion, while these movements are not possible during extension. The stability of the joint is provided by the joint capsule and the collateral ligaments on the sides of the joint, which run from the ankles to the adjacent bones of the foot.
- The lateral collateral ligament, most commonly damaged when the foot is rotated inward (80 % of all ankle sprains). It extends from the lateral ankle and consists of three opposing ligaments: the anterior (to the talus), the inferior (to the heel bone), and the posterior (to the posterior part of the talus).
- The internal ligament (deltoid) runs from the inside of the ankle in three fan-shaped bundles down to the talus, calcaneus, and navicular bone;
Factors that increase the risk of an ankle injury:
- Previous or existing ankle injuries, especially with inadequate treatment and rehabilitation (major risk factor);
- Lack of ankle strength when walking;
- Impaired or reduced mobility of the joint;
- Any disorder of the coordination (biomechanics) of walking;
- Sudden changes in direction, including acceleration or deceleration.
- Poor condition of the playing surface;
- Lack of or insufficient warm-up;
- Unsuitable or uncomfortable footwear;
- Lack of flexible fixation of a previously injured ankle.
Prevention of torn ligaments during sports:
- Movement technique training before the start;
- A complete warm-up that works all the muscles and ligaments that are particularly important for the function and stability of the joints during movement;
- Gradual increase in intensity and duration of training;
- Regular exercises to train strength, flexibility, balance and resilience of the joints;
- Practicing movement technique, especially in sports with high loads, sudden accelerations and changes of direction;
- Adequate recovery time between training sessions;
- Flexible fixation of the previously injured joint;
- wearing comfortable, appropriate footwear that ensures stable fixation of the foot and ankle;
- Proper playing surface preparation (flat, dry, etc.);
- Adequate water intake before, during and after exercise;
This information is general in nature and serves as an introduction to the issue. They do not replace the advice of a specialist doctor; In the event of an injury, a qualified specialist, a practicing orthopedic trauma surgeon, should always be consulted.
Symptoms of a ruptured ligament
The main clinical signs are acute pain in the area of injury, swelling and redness or even bruising in the area of injury, the characteristic cracking sound of a torn ligament, abnormal configuration of the articular surfaces, disruption and 'loosening' of the joint, impaired support function and pathological mobility of the components in the area of the crack.
A torn ligament in the shoulder may be associated with impaired grip function, and later calcifying subacromial bursitis, periarthritis, or tendinitis may develop. A torn ligament in the shoulder is always accompanied by severe pain and impaired motor skills.
A torn ligament can be dangerous due to complications such as tendonitis, bursitis (synovitis) and bleeding into the joint cavity with simultaneous soft tissue and muscle injuries.
Diagnosis of torn ligaments
A clear clinical picture of a ligament tear and objective examination data are one of the first steps in diagnosing musculoskeletal system injuries.
A cruciate ligament rupture in the knee, including rupture of the anterior cruciate ligament, is a reason for the mandatory exclusion of a meniscus injury in the knee using modern diagnostic methods.
Radiological examination and treatment monitoring (e.g. in the case of accompanying injuries to the cartilage) as well as MRI are essential diagnostic procedures.
A tear in the anterior knee ligament can lead to hemarthrosis (bleeding into the joint cavity), which is why this area should be punctured or arthroscopically for both therapeutic and diagnostic purposes.
SURGICAL TREATMENT
Most patients with a torn patellar tendon require surgery to restore normal function of the knee joint. During this operation, the tendon is reconnected to the kneecap.
The sooner the operation is carried out, the better the result. During a longer operation, the tendon shortens and becomes shorter.
Inpatient treatment. Suturing the tendon is sometimes performed on an outpatient basis, but most patients remain in the hospital for at least a day after such an operation. Whether this is the case in your particular case will be determined medically.
The operation can be performed under regional anesthesia (spinal anesthesia), in which only the lower half of the body is 'frozen', or under general anesthesia.
Surgical technique. To repair the tendon, the end of the tendon is sutured, and these sutures are passed through bone channels created in the lower pole of the kneecap. The sutures are then tied, restoring the normal tension of the tendon and the normal position of the kneecap.
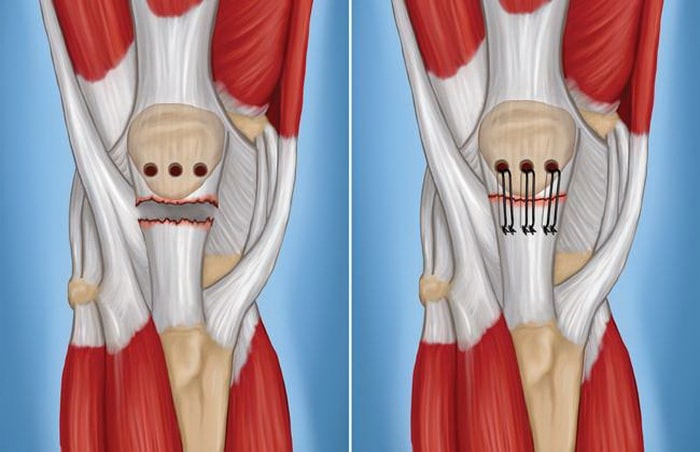
To repair the patellar tendon, small bony tunnels are created in the inferior pole of the patella (left), through which sutures are passed to secure the tendon to the patella (right).
New minimally invasive techniques. Currently, suture anchors are most commonly used to attach the tendon to the kneecap. These are small metal or polymer implants with threads. When used, bone canals in the kneecap are not required. It should be noted that the possibilities of these modern methods are much greater than in the past. The use of anchors will accelerate rehabilitation and improve functional outcome.
Additional methods of stabilization. To further protect the tendon suture, some surgeons find it necessary to further stabilize the kneecap with wire sutures while the tendon heals. In such cases, additional surgery may be required to remove such a wire suture.
RESULTS OF SURGICAL TREATMENT
Most patients return to their previous jobs and physical activities after a patellar tendon rupture. Many patients report limited range of motion of the knee joint, although most of them have almost the same range of motion as another knee joint.
If you are an athlete, your surgeon will likely want to assess the extent to which your knee joint has recovered and the strength of the surrounding muscles before allowing you to return to the sport. For this purpose, special functional tests are carried out, e.g. B. hopping on one leg. The muscle strength of the injured leg must be at least 85-90 % of the muscle strength of the sound leg. In addition to muscle strength, muscular endurance, body balance and the occurrence of swelling in the knee joint after exertion are also assessed.
The surgeon will discuss with you in detail the options and conditions for returning to competitive sport.
Symptoms of ankle ligament injuries
All three types of ankle ligament injuries have the same clinical symptoms, but the extent of symptoms depends on the severity of the injury.
A patient with an ankle ligament injury complains of pain when walking. At the site of injury, you may notice swelling and bruising. Palpation of the injured ligaments is painful. Hemarthrosis (blood in the joint cavity) is possible.
When the ankle ligaments are dislocated, the swelling is localized and the injured person feels pain but can still walk. If the ligaments of the ankle are torn, the swelling will spread to the outside and front of the foot. Walking is made difficult by the pain.

The appearance of the foot after a torn ankle ligament
An ankle ligament rupture is accompanied by hemarthrosis, swelling and bruising on the dorsal and plantar surfaces of the foot. Walking is severely impaired, sometimes impossible due to the pain.
If an ankle ligament injury is suspected, an X-ray is required in most cases to rule out a possible fracture, which can present with similar symptoms of swelling and pain. If there is no fracture, the extent of the ligament injury can be assessed based on these external signs.
Examination of the injury site can be painful because the foot must be moved in different directions during the functional test to determine the location and extent of the injury. When the ligaments are completely torn, there is joint instability. There may also be damage to the joint surfaces, which can also be suspected on examination.
If there is suspicion of significant ligament damage, destruction of the joint surfaces or bone damage, an MRI scan (magnetic resonance imaging) may be necessary. With this examination it is possible to visualize the presence or absence of fractures, ligament injuries, etc.
Treatment of ankle ligament injuries
Grade I and II ankle ligament injuries are treated on an outpatient basis.
Conservative treatment may vary depending on the extent of the ligament injury. For example, in the first degree of severity, it is advisable to protect the injured limb, cool it (simple ice should be applied as soon as possible after the injury - within 20-30 minutes) and immobilize it sufficiently (e.g. with a tight Association). It is also advisable to keep your feet above body height when resting or sleeping. The combination of these methods can significantly reduce swelling and pain and eliminate dysfunction of the lower limbs.
For Grade II injuries, the same treatment methods are used, but over a longer period of time. In addition, special splints can be used to immobilize the foot and ankle for a longer period of time.

Ankle splint for ankle injuries
For severe injuries (Grade III), a plaster cast remains on the injured limb for 2 to 3 weeks. Even in this case, surgery is rarely necessary.
During rehabilitation, common physiotherapy methods such as ultrasound and electrical stimulation are used to reduce swelling and pain and prevent chronic diseases. Physiotherapy – active and passive exercises to train the joint – is also an important part of rehabilitation after an injury. If the exercises are too painful, you can try to reduce the strain by doing them in water. The difficulty of the exercises is gradually increased depending on the level of recovery - as soon as the previous exercises are easy to perform, more difficult movements are added. In this way, muscle strength and range of motion of the joint are restored over time.
Read more:- Injury to the ligaments of the ankle.
- Rupture of the ligaments of the ankle.
- Damaged ligaments of the ankle.
- Treatment of torn ligaments in the ankle.
- Damaged ligaments of the ankle photo.
- Treated subluxation of the ankle.
- Injury to the ankle.
- dislocation of the ankle.
