Early detection of Guillain-Barré syndrome prevents complications and improves the prognosis. The diagnosis is based on the characteristic clinical signs of the disease. To clarify the diagnosis, additional test procedures are carried out:

- paraparesis
- etiology
- Types of obstetric paraparesis
- symptoms
- Symptoms of hemiparesis
- Peripheral hemiparesis
- Central hemiparesis
- Paresis in radiculopathy and myelopathy
- Treatment of hemiplegia
- Medical therapy
- Physiotherapy for paralysis.
- Orthopedic devices and other treatment methods
- DEGREES OF CEREBRAL PALSY
- CAUSES OF CEREBRAL PALSY
- Central paralysis and paralysis
- Symptoms of central paralysis and paresis
- etiology
- Symptoms of Guillain-Barré syndrome
- Treatment results with the Filum system
- List of references.
- Classification of paresis
- causes
- Symptoms of the disease: when, how and why
- How we can help
paraparesis
Paraparesis is a neurological syndrome that affects two limbs and is characterized by the inability to conduct nerve signals, resulting in low muscle activity and, in severe cases, complete paralysis.
This disease is quite common. Paraparesis in children can be congenital (due to fetal malformations or intrauterine injuries, infectious diseases of the mother during pregnancy) or acquired (due to tumor formations or spinal cord injuries). It occurs in both adults and children, regardless of gender.
There are several forms of the disease, of which spastic paraparesis is the most common. The diagnosis of paraparesis is made after a comprehensive examination. The treatment has a positive effect and in severe cases partial motor activity can be restored. The therapy lasts a long time.
etiology
The motor function of the lower limbs is influenced by the brain: if impulses are not passed through the central or peripheral nerves, paraparesis occurs. If both limbs are affected, the cause may lie in the spinal cord, spine or lumbar spine.
The causes of this problem are:
- Head injuries, spinal injuries of any kind;
- Disc prolapse;
- stenosis of the spinal canal;
- Tumor-like growths;
- vascular diseases of the lower limbs;
- B vitamin deficiencies;
- thrombosis of the vertebral arteries;
- sequelae of hematomas;
- autoimmune diseases;
- abscesses;
- Multiple sclerosis;
- Myelopathy and its variants.
The pathology is caused by a history of infectious diseases or genomic abnormalities, which are often hereditary. The pathological process must be treated and the cause of the disease eliminated, as it can progress rapidly and lead to paralysis and complete loss of motor functions.
Cases of paraparesis in children are often reported as a result of birth trauma. Every case is different and requires a good and early diagnosis.
Types of obstetric paraparesis
Depending on the severity Obstetric paraparesis can be divided into two types:
Depending on the location of the injury, obstetric paresis is divided into:
– UpperUpper paresis: In the upper type, which is more common than the lower type, the arm hangs passively, the hand has no or limited mobility, the arm is usually adducted to the trunk and rotated inward, and the hand is in a palmar flexion position. The fold between torso and shoulder is deepened. When the child is picked up, the shoulder hangs back. The muscle tension is sluggish, passive movements and joints are spared.
– LowerLower: In lower paralysis there is no movement of the hand and fingers, the hand hangs down and the child lifts it by supporting it with the other hand. There is atrophy of the small muscles of the hand, resulting in hyperextension of the proximal phalanges and flexion of the distal phalanges.
– TotallyComplete paresis of the hand (total arm paresis) is the result of damage to the upper and lower primary brachial plexus bundles in the spinal cord or detachment of nerve roots from the spinal cord.
symptoms
Neonatal paresis is often accompanied by cerebral abnormalities: tremor, reduced muscle tone, increased excitability, inhibition of unconditioned reflexes. All anomalies are related to the complex effects of birth trauma and asphyxia on the newborn's body. The lesions are transient and resolve rapidly, suggesting an association with impaired cerebrospinal circulation.
The course of paresis depends on the severity of the lesions. With mild impairments, hand function is restored from the first days of life, and active movements are fully performed within 2-5 months. In some cases, muscle weakness may persist for a long period of time. It becomes more noticeable when the child begins to assume an upright position, that is, sitting or standing. Impairment of the arm's function can be seen when it is raised beyond a horizontal position or when the arm is pulled backwards. Decreased muscle strength may be evident when the child reaches for a toy.
With moderate to severe damage, recovery of arm function is slower and may be incomplete due to muscle wasting, contractures, and nerve fiber degeneration. With severe spinal cord injuries, detachment of the dorsal roots, rupture of the brachial plexus, the restoration of hand function is minimal, there is atrophy, muscle contractures, a tendency to dislocation of the shoulder joint.
Symptoms of hemiparesis
Peripheral hemiparesis
Reduced or absent innervation in peripheral flaccid paralysis leads to varying degrees of impairment: hypotonia, atrophy, and impaired reflex function.
Symptoms range from a slight decrease in tension, muscle strength and reflexes to their complete loss. Fasciculations (involuntary muscle contractions) are also occasionally observed.
Central hemiparesis
Central hemiparesis is a spastic paralysis characterized by muscle hypertension.
- The arm is usually pressed against the torso, the knee is bent and the hand and foot point downwards.
- The limbs can only be bent or flexed by applying force, although no smooth transition is possible - the arm or leg folds like a pocket knife.
- Superficial reflexes decrease and deep reflexes increase. Clonic convulsions are possible.
- There are several abnormal flexion and extension reflexes.
- Synkinesia (involuntary repetition of movements of the second limb after the first) is present.
- Abnormal facial expressions (nervous tic, smoothing of the nasolabial fold and drooping of the corner of the mouth on the affected side, etc.).
Paresis in radiculopathy and myelopathy
- The paresis in radiculopathies is usually one-sided: there is a monoparesis in which either the upper or lower extremity is affected, depending on the extent of the nerve damage. Occasionally, bilateral involvement of the upper or lower limbs can also occur - paraparesis. Hemiparesis in radiculopathies is not common.
- Large dorsal hernias, dislocations and spinal injuries causing CM compression result in: spastic paraplegia and quadriplegia (when the lesion affects the C1 to C5 level of the cervical spine).
Treatment of hemiplegia
Treatment for paralysis consists of a combination of medication and physical therapy. The treatment must be aetiotropic, that is, the disease responsible for the peripheral nerve damage and conduction disorder must be eliminated. Unfortunately, many of the changes are irreversible, so the status quo must be maintained to prevent further progression.
Medical therapy
Paralysis drugs are prescribed to improve metabolism, nerve conduction and adaptation:
Physiotherapy for paralysis.
With flaccid hemiplegia, massage and physiotherapy are carried out according to the following scheme:
- First, the doctor performs passive movements with the hand or leg.
- As the limbs develop, the trainee begins active, non-weight-bearing movements.
- In the third phase, resistance movements come into play.
The movement methods are dosed gradually.
Spastic paralysis requires mechanical exercises that are performed on robots using the Hal therapy method. This method involves repeating the same movements over and over again.
Orthopedic devices and other treatment methods
A great help in the treatment of hemiparesis are:
- orthopedic splints, bandages that fix the limbs in the correct position;
- orthopedic shoes.
- Orthopedic chairs and cots.
Sick children need not only therapeutic treatment, but also constant care and monitoring:
- It is important to set up the child's work and sleeping area accordingly.
- Young children need to learn to crawl and walk properly.
- In case of speech disorders and developmental delays, additional sessions with a speech therapist, child psychologist for social adaptation and other specialists are required.
- Work training, physical hardening and outdoor activities are of great importance.
DEGREES OF CEREBRAL PALSY
The modern classification distinguishes five degrees of cerebral palsy, where the first degree is characterized by a mild impairment that allows the child to move independently, and the fifth degree is characterized by complete dependence on others.
The GMFCS (Gross Motor Function Classification System) is a functional classification of cerebral palsy. It is a descriptive system that takes into account the level of motor development and limitations of movements in daily life for 5 age groups of cerebral palsy patients: up to 2 years, 2 to 4 years, 4 to 6 years, 6 to 12 years , 12 to 18 years. According to the GMFCS, there are five stages of gross motor development:
CAUSES OF CEREBRAL PALSY
For many parents, a diagnosis of cerebral palsy sounds like a terrible verdict. It is a disease that cannot be completely cured. A family's life changes when an extraordinary child is born. Unfortunately, even today, specialists are still unable to diagnose cerebral palsy in the womb. The causes of cerebral palsy in children are diverse and are divided into:
prenatal damage (infections and birth defects, chromosomal abnormalities, endocrine, cardiovascular disorders, maternal toxicity during pregnancy
maternal toxicity during pregnancy, etc.).
Perinatal insults (prematurity, birth complications, birth trauma, hypoglycemia, CNS infections)
Postnatal injury (brain injury, infections, intracranial hemorrhages, acquired encephalopathies, neonatal seizures).
It is difficult to name the exact cause of the disease, but factors that increase the likelihood of cerebral palsy can be named. These include environmental factors, the mother's lifestyle before and during pregnancy, and diseases that occur during pregnancy.
Any form of cerebral palsy requires long-term treatment and rehabilitation measures. The child's well-being and future quality of life largely depend on how early the diagnosis is made and how treatment and rehabilitation are organized.
No family is immune from having a child diagnosed with cerebral palsy.
Principles of the Dobroserdiye Charitable Foundation's approach to supporting the treatment and rehabilitation of children with cerebral palsy.
General principles of assistance.
- We provide treatment and rehabilitation assistance to disabled children diagnosed with infantile cerebral palsy (ICP), up to the age of 18, who are citizens of the Russian Federation and registered and residing in Moscow and the Moscow region, regardless of their status nationality, their faith or religion. We work with the child's legal representative and act in the child's best interests.
- The decision to help a disabled child within the framework of the 'Movement for Life' project is made only after consultation with an orthopedic specialist from the Foundation (the costs of the consultation are borne by the Foundation).
- The fund begins collecting all funds to support a disabled child as soon as the beneficiary is accepted into the project.
- We try to collect funds as quickly as possible, but cannot guarantee that funds will be collected by a specific date.
- Our goal is to help as many children as possible, but due to limited resources we cannot help everyone in need. We reserve the right to refuse assistance without giving reasons.
Central paralysis and paralysis
paralysis is characterized by a complete loss of feeling and movement in one area of the body, while paresis is characterized by a partial loss of feeling and movement. Depending on the degree of damage, paralysis and paresis can occur centrally or peripherally.
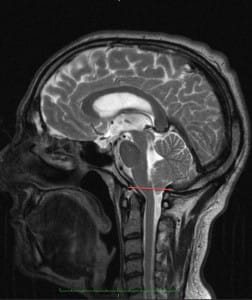
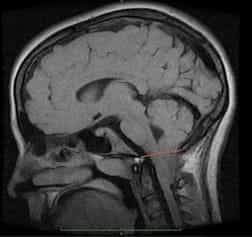
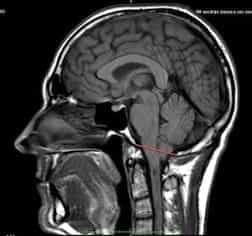
The cerebral control of motor and sensory activities is quite complex. To put it simply, it works as follows. Certain nerve cells - central motor neurons - are located in certain areas of the so-called precentral cortex of the cerebral hemisphere. The branches (axons) of these neurons form pathways. These pathways cross to the opposite side at the border between the brain and spinal cord, descend and end at the frontoparietal level (the so-called 'ventral tegmentum'). anterior horns) of the gray matter of the spinal cord. The motor neuron II is located in the front horns. From this neuron, motor fibers run to a specific anatomical area.
The death of motor neurons in the cerebral cortex inevitably leads to central paralysis or paresis. The main cause of central paralysis and paresis is a cerebral hemorrhage (stroke). A stroke can be caused by intracerebral bleeding (hemorrhage) or blockage of these vessels by atherosclerotic plaques (ischemia). In addition to stroke, central paralysis can also be caused by brain injuries, neuroinfections and brain tumors.
Symptoms of central paralysis and paresis
In central paralysis, the peripheral neurons in the frontal horns of the spinal cord remain intact. Likewise, the reflex arc nerve fibers from the spinal cord to the innervated areas remain intact. This leads to pathological activity of spinal cord neurons that have lost the inhibitory, regulatory influence of the cortex as a result of the stroke. This activity is accompanied by muscle spasms caused by the loss of the ability to move in certain anatomical areas. Therefore, central paresis is also called spastic paresis.
In a stroke, the paresis or paralysis affects one side of the body (hemiparesis) and is contralateral, that is, it develops on the side opposite the damaged hemisphere. In contrast, facial muscle paralysis, which causes facial asymmetry, occurs on the affected side. In this case, the affected area covers a fairly large area. Patients with central paralysis show a large increase in the tension of the paralyzed muscles. The muscles are tense, the upper extremity is flexed and reduced to the trunk, the lower extremity is maximally erect and therefore stretched.
If the central paresis is mild and the patient can still move, a characteristic gait can be observed. In order to avoid the patient hitting the ground with his straight leg, he performs rotational movements with this leg. In central paresis or paralysis, physiological tendon reflexes are increased, and abnormal tendon reflexes that are not normally present are often noted. In contrast, the cutaneous reflexes of the abdominal wall, feet, and scrotum are inhibited or absent.
Despite the extent of the changes, atrophic processes in the muscles do not usually develop in central paralysis. The peripheral nerve fibers that lead to the muscles do not degenerate either - they remain intact.
etiology
The disease is caused by autoimmune damage to the myelin sheath of nerves following infection, trauma, or surgery.
Risk factors that increase the risk of inflammation:
- herpes infection (Epstein-Barr virus, herpes types 1 and 2, cytomegalovirus);
- Infectious mononucleosis;
- Viral enteritis;
- ACUTE RESPIRATORY INFECTIONS;
- Systemic connective tissue pathology (scleroderma, lupus erythematosus);
- HIV;
- fractures, concussions;
- cave surgery;
- malignant tumors.
Researchers at the University of Oxford recently discovered that Coronavirus can also cause Guillain-Barré syndrome.
A breakdown of the immune mechanisms leads to the formation of antibodies not only against the infectious agent, but also against the myelin sheaths of the nerves, which are thereby broken down (demyelination).
Symptoms of Guillain-Barré syndrome
The syndrome develops 2 weeks after infection, trauma or surgery.
- Prolonged subfebrile fever (37-37.8 degrees);
- Muscle aches;
- paresthesia (tingling in the fingertips);
- weakness in extremities;
- chills in the hands and feet;
- excessive sweating;
- general malaise.
In most cases, the disease begins acutely with symmetrical flaccid paralysis of the arms and legs. The pathology is ascending - muscle weakness begins in the lower limbs and then spreads to the chest, upper limbs, neck and face.
The characteristic symptoms of the disease are:
- flaccid paraparesis (only arms or legs affected) or quadriparesis (arms and legs affected);
- muscle weakness in the proximal limbs (closer to the body);
- Reduction or complete extinction of tendon reflexes;
- Decreased sensitivity to pain, touch and temperature;
- Autonomic disorders (sweating, tremors, cardiac arrhythmias, unstable blood pressure);
- Disorders of breathing and swallowing.
Symptoms take 2 weeks to appear and the disease lasts 3-4 weeks. Life-threatening complications include cardiac arrest, respiratory arrest, difficulty swallowing.
Treatment results with the Filum system
More than 1,500 patients with Arnold-Chiari I syndrome, with/without syringomyelia and/or scoliosis, have already been operated on using the Filum System® method.
The aim of the operation is to stop the progression of the disease (both anatomical (increased tonsil prolapse) and symptomatic (further development of symptoms)). In most cases, symptomatic improvement and in some cases elevation of the cerebellar tonsils are noted.



List of references.
- Dr. Miguel B. Royo Salvador (1996), Syringomyelia, escoliosis i malformation de Arnolda Chiari idiopáticas, etiología común (PDF). REV NEUROL (Barc); 24 (132): 937-959.
- Dr. Miguel B. Royo Salvador (1996), Platibasia, impresión basilar, retroceso odontoideo y kinking del tronco cerebral, etiología común con la siringomielia, escoliosis y Arnold-Chiari malformation idiopáticas (PDF). REV NEUROL (Barc); 24 (134): 1241-1250
- Dr. Miguel B. Royo Salvador (1997), Nuevo tratamiento quirúrgico para la siringomielia, la escoliosis, the Arnold-Chiari malformation, the bending of the cerebral tronco, the retroceso odontoideo, the basilar impresión and the idiopacific platibasia (PDF). REV NEUROL; 25 (140): 523-530
- MB Royo-Salvador, J. Solé-Llenas, JM Doménech, and R. González-Adrio, (2005) 'Results of the section of Filum terminale in 20 patients Syringomyeliascoliosis and Chiari malformation' (PDF). Acta Neurochir (Vienna) 147: 515-523.
- MB Royo-Salvador (2014), 'Bibliography of the Filum-System®' (PDF).
- MB Royo-Salvador (2014), 'A Brief Introduction to the Filum System®'.
Described: 1883 by the surgeon and anatomist John Cleland (1835-1925) from Perthshire, Scotland. He described elongation of the cerebellar vermis, prolapse of the cerebellum and fourth ventricle in a boy with hydrocephalus, encephalocele, and spina bifida. In 1891 and 1896, Hans Chiari described and classified new cases. In 1894, Jules Arnold helped spread knowledge about the disease.
Named: Schwalbe and Gredig in 1907 as 'Arnold Chiari malformation'. The official modern nomenclature in the World Health Organization's Codification and Classification of Diseases refers to this disease as 'Arnold-Chiari syndrome or disease I' (Q07.0, CIE-10). (WHO, (International Statistical Classification of Diseases and Related Health Problems, 10th Revision (c) Geneva, OMS, 1992).
Classification of paresis
Although it is common, few people know what lower limb paraparesis is and how it occurs. It is a neurological syndrome in which 2 limbs (the upper or lower) are paralyzed at the same time. Muscle strength is reduced and the ability to perform voluntary movements is partially lost. This is because the nerve impulses from the brain to the spinal cord and then to the peripheral nerve endings in the legs do not reach. A particular muscle or group of muscles does not receive a nerve signal, resulting in weakness and atrophy (thinning) of the fibers. This is caused by diseases of the brain, lesions of the spinal cord and its roots.
It is important to distinguish between inferior paraparesis, paralysis, and other similar disorders. Paralysis (plegia) is a condition in which there is a complete lack of voluntary movements. It occurs for the same reasons as paresis.
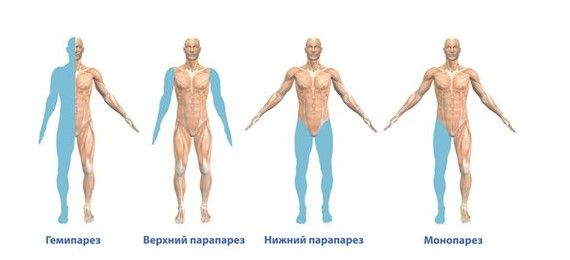
Types of paralysis by number of limbs affected
Types of paralysis according to the number of affected limbs:
- Monoparesis – one limb is affected.
- Paraparesis – 2 arms or legs are affected.
- Triparesis – 3 limbs are affected.
- Tetraparesis – 4 limbs are affected at the same time.
Paraplegia is the paralysis of both upper or lower limbs.
Depending on which neurons are affected (central or peripheral), these types of paraparesis are distinguished:
- Lower spastic paraparesis – simultaneous decrease in motor activity, increased muscle tone or even muscle spasms and increased segmental reflexes. Spastic paraparesis occurs when the central motor neurons are damaged.
- Lower flaccid paraparesis – the muscles relax, begin to atrophy and protective reflexes gradually disappear. This happens because the peripheral motor neurons are damaged.
- Inferior mixed paraparesis – the symptoms of spastic paraparesis and flaccid paraparesis occur when both central and peripheral neurons are damaged.
causes
As already mentioned, movement disorders of both limbs are caused by damage to central or peripheral neurons. They are often the result of compression of the spine (thoracic or lumbar), spinal cord, surrounding roots or blood vessels.
Doctors have distinguished the main causes of spastic paraparesis:
- Transient ischemic attack.
- Brain stroke.
- Tumor or abscess in the spinal cord area.
- Inflammatory process of infectious or non-infectious origin.
- Multiple sclerosis.
- Transient paresis of two limbs that occurs after an epileptic seizure.
- Injuries to the spinal cord or its roots.
Common causes of flaccid paralysis of both limbs:

muscle weakness
- Acute polymyositis (Guillain-Barré syndrome).
- Poisoning with heavy metal salts.
- Long-term use of certain medications, e.g. B. Cytostatic drugs (vincristine), tuberculosis drugs (isoniazid), muscle relaxants (tolperisone).
- Autoimmune diseases in which damage to the peripheral nerves occurs.
- Acute intermittent porphyria.
- Pathologies that disrupt neuromuscular transmission, e.g. B. Myasthenia gravis (muscle weakness), botulism (toxicity affecting the medulla oblongata and spinal cord).
- Inflammatory myopathies in which the striated muscles are damaged.
- Hypo- or hyperkalemic periodic paralysis.
One of the pathological causes is the lack of vitamins B9, B12, etc.
Mixed-type paraparesis occurs in Lou Gehrig's disease (lateral muscular sclerosis) and other spinal cord pathologies.
A notice. Paraparesis most commonly occurs in myelopathies (spinal cord lesions) caused by osteochondrosis or spondylosis (bony overgrowths on the edges of the vertebrae). The spinal cord or its roots are pinched by a bulge, a herniated disc, or a displaced vertebra. The disease is often triggered by trauma or a tumor in the spine.
Symptoms of the disease: when, how and why
A child with spastic quadriparesis suffers from damage to both arms and legs. The disease manifests itself as spasticity, a condition in which the muscles of the limbs contract frequently and strongly but cannot relax on their own.
There are five levels of movement disorders:
- walking without restrictions;
- comes with restrictions;
- requires a cane, crutches or walker to walk;
- requires a motorized wheelchair for independent mobility;
- Complete dependence on other people.
In one in two children with this form of cerebral palsy, epilepsy occurs in addition to the symptoms of quadriplegia. Intellectual, visual, auditory and language disorders are not uncommon.
An experienced doctor detects clear signs of cerebral palsy in the first week of a newborn's life, but the diagnosis is made much later. In this way, the risk of cerebral palsy is recognized early, but the child already receives help.
How we can help
Although there is no known cure for quadriplegia, there are medications that can help relieve the condition. Neurologists at the Center for Speech Neurology and Pediatric Rehabilitation at NeuroSpectrum select the most effective combination of medications for each patient. Our massage therapists have extensive experience working with patients with cerebral palsy and have mastered the technique of myofascial massage.
The specialists of our center also help mentally stable children with 'difficult' behavior: aggressive, withdrawn, shy. We help overcome speech problems, offer speech therapy massages and conduct individual and group lessons with a speech therapist.
Read more:- paraparesis.
- Lower spastic paraparesis.
- Inferior paresis - what is it?.
- paresis of the lower body.
- paresis is.
- These are the pronator muscles.
- Equino valgus.
- Bracers for children with cerebral palsy.
