Classic pain – aggravated by exertion, morning stiffness, swelling, swelling and hypersensitivity of the skin over the affected joint. Occurs as a result of autoimmune reactions, obesity, aging, genetic predisposition, gout, after infectious diseases.

- Arthritis of the foot: symptoms and treatment
- Symptoms of osteoarthritis in the foot
- Ligament stretches
- Wart on the sole of the foot
- Which warming and vasodilating ointments should I use?
- Pain-relieving and anti-inflammatory ointments
- Foot pain and osteopathy
- When to see a doctor
- Foot injuries ↑
- What to do if you have foot pain: First aid
- Conservative rehabilitation methods
- Causes of abdominal pain and diarrhea
- Some medical conditions that cause diarrhea and stomach pain
- 1 Intestinal infections and toxic infections
- 2 Diarrhea in travelers
- Natural pain reliever
- Conclusions
Arthritis of the foot: symptoms and treatment
Arthritis – joint pathology associated with changes in synovial fluid, inflammation and destruction of joint components.
Osteoarthritis of the foot - the most important component of the human musculoskeletal system - is accompanied by distortion of the anatomical features, mechanics and impairment of the function of the foot and the leg as a whole.
Inflammatory foot diseases have very negative consequences because nature has entrusted the foot with important tasks: it ensures an upright posture, helps maintain balance and fulfills elastic and resilient functions. The foot is also rich in reflexogenic areas.
The musculoskeletal system is a complex system in which all parts are interconnected and influence each other. That is why arthrosis of the foot can lead not only to impairment of the entire limb, but also to impairment of the spine (due to incorrect redistribution of loads). The spine is the support of the human body through which the spinal cord runs. Therefore, as osteoarthritis progresses, it can affect vital organs throughout the body.

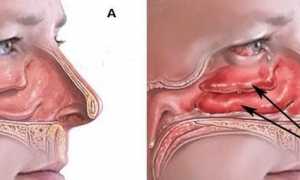
The foot consists of a large number of small bones connected by joints that form the tarsal arch and ensure the mobility of the foot. Any of these small joints (e.g. the Lisfranc joint or Shopar joint) can become inflamed under adverse conditions, and the inflammation tends to spread over time and affect new areas, resulting in tissue destruction, an impairment of mobility and even complete immobilization, i.e. leading to crippling arthrosis of the foot.
There are many causes that can lead to a risk of osteoarthritis in the foot. Causes include genetic predisposition, infectious agents (fungi, viruses, bacteria), metabolic disorders, foot injuries, obesity, aging of the musculoskeletal system, overexertion or lack of exercise, incorrect footwear, bad habits, micronutrient deficiencies, stress, other chronic diseases (e.g. diabetes) , individual foot characteristics and structure.
Symptoms of osteoarthritis in the foot
Although each type of arthritis of the foot has its own specific symptoms, all types of arthritis share some basic symptoms:
Pain in the affected area. Perhaps the main symptom of arthritis. In the beginning they are easy and most people don't pay attention to them. Then the pain increases so much that it has to be relieved with painkillers. At the same time, osteoarthritis in the foot can immediately cause severe pain. As a rule, the pain occurs at rest and with movement, but it increases significantly with movement. It is strongly recommended that if you experience the mild pain of foot osteoarthritis, you should take immediate action to prevent the disease from causing serious damage to the joints of the foot and the entire musculoskeletal system.
Redness of the skin, local fever and swelling due to inflammation of the foot. These symptoms of foot arthritis come and go at regular intervals. However, its disappearance does not mean that the disease is over, only that remission has occurred (a temporary state in which the foot arthritis is practically no longer noticeable and there are no or few symptoms).

Restricted mobility and a reduced range of motion in the affected joints is a necessary sign of arthritis of the foot. In the early stages of foot osteoarthritis, joint stiffness occurs in the morning, immediately after getting up. If the person walks for a few minutes, the stiffness will subside. This is a very important symptom of foot osteoarthritis and should be treated by a qualified specialist as soon as possible. It only gets worse: Arthritis stiffness in the foot can happen all the time.
Joint deformities (swelling, curvature, nodules, 'bones', bony erosions, toe protrusion) are a sign of an advanced stage of foot arthritis. The gait deteriorates, the toes may claw or hammer, ankylosis and subluxation of the ankle joints and valgus deformities may occur.
Ligament stretches
One of the most common causes of foot or leg pain is a ligament strain. Ligaments are bundles of tough tissue that connect bones together and form joints. Ligament strains can be caused by walking for long periods of time in uncomfortable shoes, or simply by putting too much strain on the feet compared to what we are used to, or by sudden and clumsy movements while walking or running on uneven ground. Dancers or soccer players who train on artificial turf can sometimes experience pain in their toes because the ligaments around the joint become overstretched. In addition to the pain, a sprain can cause swelling and restricted movement. The most important treatment for sprains is rest. In severe cases, the help of an orthopedic trauma surgeon may be necessary.
If your big toe hurts and swells, gout may be the cause. Gout is a type of arthritis that involves a buildup of uric acid in the body. Uric acid crystals can build up in the joints and cause severe pain and inflammation even at rest. Gout usually affects the joints of the big toe first. It is sometimes difficult to distinguish gout from other types of arthritis. If the pain in the toe lasts for several days, is very severe, increases with the slightest movement or even touch, and is accompanied by redness of the skin and swelling of the joint, you should call your family doctor or see a doctor.
Wart on the sole of the foot
A plantar wart is a hard growth on the sole of the foot. It can cause pain in the foot or heel because its weight puts pressure on the surrounding tissues of the foot. A wart looks like a small, flat, rounded patch of rough skin, sometimes with a black dot in the center. There are ways to treat plantar warts at home. If these are not effective, professional help from a dermatologist should be sought.
Sometimes a hard lump forms at the base of the big toe, causing pain in the foot and making walking difficult. This is a common problem, especially among women. The big toe curves toward the other toes, called a valgus deformity, and the joint of the toe begins to protrude excessively, forming a bony bump. An orthopedist and traumatologist treats the acetabular joint.
Which warming and vasodilating ointments should I use?
This group includes topical ointments that stimulate blood circulation around the joint, thereby relieving pain and spasm. The cells are better supplied with oxygen and nutrients so that other processes (e.g. cartilage regeneration) can occur more intensively.
Snake or bee venom and red pepper are used as warming agents. Do not use on broken skin (with wounds) or inflamed joints. Preparations containing poison should not be used for long periods of time as there is a risk of 'stretching' the ligaments. Warming ointments should be applied before going to bed.
The most popular preparations from this group are:
- Voltaren – with the addition of snake venom;
- Apisartron – with bee venom;
- Espol – with red pepper;
- Gevkamen – contains several ingredients including menthol, camphor, clove and eucalyptus essential oil.
Warming ointments contain bee or snake venom
Pain-relieving and anti-inflammatory ointments
These ointments are based on diclofenac, ibuprofen and other strong anti-inflammatory agents. Their use is appropriate in the initial stages of treatment of arthrosis or osteoarthritis, as well as in cases of exacerbations. The most commonly used include:
- diclofenac;
- Fastum gel – based on ketoprofen with analgesic effect;
- Naise – contains nimesulide with pain-relieving and anti-inflammatory effects;
- Dolgit – contains ibuprofen and a warming agent.
Foot pain and osteopathy

Calluses, corns, bone protrusions, arthritis, osteoarthritis, swelling and varicose veins - many of these problems are caused by flat feet, short legs or a crooked pelvis that have been 'treated' with orthoses of varying thickness. The human body is in a delicate balance, and all it takes is one imbalance for disease to snowball.
Osteopathy can help prevent this. The therapist works on displaced and deformed areas and brings organs, joints, cartilage and bones back into the correct position. It is a painless and non-invasive procedure, which is why it is suitable and recommended for very young children who may have suffered trauma during birth. Osteopathy is effective for adults and school-age children who spend a lot of time in school and whose flat feet and other defects are slowly becoming noticeable.
The osteopath restores the symmetry of the body, shows a series of corrective exercises and restores the mobility of the body so that the effects of the suffering are eliminated.
When to see a doctor
If you have had problems in both feet for a long time, you should not delay seeing a doctor. Even mild ailments require attention - vigilance can prevent complications.

However, there are medical conditions that require immediate treatment. See a doctor immediately:
- if injuries are suspected;
- Swelling and deformation of the ankles, numbness in the toes;
- for severe pain that lasts for several days;
- When every movement or touch causes pain and discomfort;
- if the skin on your feet changes color when you have a fever;
- if the foot pain is caused by a circulatory disorder or diabetes.
Foot injuries ↑
Different types of injuries – are a common cause of foot pain itself. The most common foot injuries include:
- Bruises are the most common type of injury. They arise from blunt trauma and are characterized by pain in the foot, hematomas and swelling of the skin. X-rays are taken to rule out fractures or dislocations. The patient is advised to take it easy for the first few days;
- Ligament strains – occur immediately during sporting activities or heavy physical work. After the injury there is swelling, severe pain and bleeding under the skin. The ligaments in the ankle joints are often damaged, causing pain in the upper part of the foot. All movements are restricted.
diagnosis
The first step to full recovery is Professional examination by a spine surgeon. He can narrow down the causes of the symptoms using external signs. The patient is recommended an MRI scan, X-rays of the feet, bones, ligaments and tendons. The doctor makes the correct diagnosis and prescribes the appropriate treatment, taking into account the results of the initial examination.
Treating pain in the foot when walking
The special chiropractic techniques of the chiropractors and verbologists at the Dr. Ignatiev help patients with foot pain recover quickly.
What to do if you have foot pain: First aid
Rest the injured limb calmly and in an elevated position with pillows, blankets or other objects. This decreases blood circulation and helps reduce swelling.
If injured, apply cold and secure the foot with a tight bandage or splint. If you suspect a fracture and have serious complications, you should go to the nearest trauma center (there is a 24-hour trauma doctor's office in every city).
In case of frostbite, you should apply a dry bandage and never try to warm the feet using intensive methods, as this can cause further tissue damage. Topical anesthetics and anti-inflammatories in the form of ointments or gels may be used to relieve symptoms of nontraumatic lesions before seeking medical attention.
Conservative rehabilitation methods
Therapy consists of a specific exercise program determined by the doctor after an assessment of the condition. Depending on the type and severity of the injury, the specialist determines the intensity of the permissible load and, if necessary, prescribes function-correcting and supportive orthopedic aids for the duration of the treatment.
In the case of sprains or fractures, a reduction is performed, in the case of severe pain, a nerve block is performed (before and after these procedures), and a plaster cast is applied. The following drugs are used in treatment:
- NSAIDS;
- antibacterial and antiviral preparations;
- Means for improving blood circulation in vascular pathologies;
- Revision of the antidiabetic treatment regimen.
Once acute symptoms subside, patients are referred for physical therapy to restore full function of the foot as quickly as possible. Modalities such as physiotherapy, massage, electrophoresis with novocaine, electrical stimulation, UHF and laser therapy are considered effective.
Causes of abdominal pain and diarrhea
These symptoms are most often associated with diseases of the abdominal organs: stomach, intestines, liver, gallbladder and bile ducts, pancreas, internal genital organs and urinary bladder. The pain is caused by contractions or stretching of the walls of the hollow organs (intestines, stomach, gallbladder), stretching of the outer membrane of the liver and pancreas, poor blood circulation and inflammation of the organs themselves as well as the abdominal skin that covers them.

Physiologically, loose stools can be caused by:
- increased secretion of fluid into the intestinal cavity due to irritation of the intestinal cavity, e.g. B. through bacterial toxins in food poisoning,
- Accumulation of water-attracting substances in the small or large intestine, such as: B. if you have lactose intolerance;
- Inflammation of the intestines, accompanied by the secretion of various fluids, e.g. B. Mucus, pus in non-specific ulcerative colitis;
- Increased intestinal peristalsis, e.g. B. in irritable bowel syndrome,
- slowed motility, e.g. B. in scleroderma.
Due to common causes, diarrhea and abdominal pain often occur in combination. In particular, an increase in the volume of intestinal contents and the accumulation of gases that stretch the intestinal walls lead to pain. Inflammation and cramps, in turn, worsen symptoms.
Some medical conditions that cause diarrhea and stomach pain
Diarrhea can be divided into acute and chronic forms. Acute episodes can last up to 2 weeks 1 . If the loose stool lasts longer than 4 weeks, it is called a chronic form 2 . Both variants can be caused by the same disease.
1 Intestinal infections and toxic infections
Acute diarrhea is usually infectious in nature1 and is caused by the ingestion of pathogenic microorganisms or their toxins via contaminated water and food as well as by neglect of personal hygiene.

- Bacteria such as E. coli, Salmonella, Shigella, Vibrios, Campylobacter and Yersinia;
- Viruses such as enteroviruses, rotaviruses or adenoviruses;
- Various protozoa: amoebas, redworms, giardia, etc.
Liquid stools can occur several to 30-40 times a day1, often accompanied by abdominal cramps, fever and weakness. The occurrence of nausea and vomiting may be accompanied by damage to the stomach and small intestine, that is, with the development of inflammatory bowel disease1.

Nausea, weakness, abdominal pain and diarrhea, mucus and blood in the stool, and improper bowel movements are more common in colitis, that is, inflammatory bowel disease 1.
Intestinal infections, especially in children and the elderly, can cause dehydration. If you experience frequent vomiting or loose stools, you should consult an infectious disease specialist.
2 Diarrhea in travelers
Traveler's diarrhea is most common in visitors from Central and West Africa and India. What you can do: Diarrhea and stomach pain can be related to changes in diet, water quality, acclimatization, time zone changes and other stressors. Some strains of E. coli 1 cause the infection. The stool disorders occur upon arrival or within the first two days in the new country, usually up to three times a day, are accompanied by cramps and abdominal pain, last on average no longer than a week1 and can be treated independently. If symptoms persist for a long time, medical consultation and examination is required.
Natural pain reliever

To prepare, mix 1 teaspoon of powdered ginger with 180 ml of cooled, boiling water. Add 25g of fresh honey, mix thoroughly, cook for 15 minutes and then cool.
The ginger drink is taken in the morning, before breakfast and 60 minutes before bed.
Conclusions
It is also necessary to treat the underlying disease. Your doctor may prescribe medication and physical therapy. For more information about what else you should do if your joints hurt at night, watch the video in this article.







- tarsal and metatarsal joints.
- The tarsal of the foot.
- tarsus.
- tarsus.
- The tarsal and metatarsal bones.
- tarsus.
- If your soles and heels hurt.
- Pain in the heel bone of the foot.

