Quadriceps syndrome is characterized by back pain, which can occur both with movement and at rest. The reason for this is the main function of the quadriceps muscle - it supports the spine. Therefore, the quadriceps muscle works most of the time - with movement, with simply standing or sitting and even lying down, with the slightest movement.
- Inflammation of the nerves (neuralgia) of the ankle nerve
- causes
- Anatomical and functional features
- causes
- Causes and types of nerve damage
- Primary and secondary disorders
- clinical picture
- types of pain
- diseases and their symptoms
- Treatment of anomalies
- Methods for pain relief
- pain after injury
- When to see a doctor for muscle pain
- Treatment
- Pharmacological treatment
- physical therapy
- treatment tactics
- Symptoms and treatment of a pinched sciatic nerve
- Symptoms of a pinched sciatic nerve
- Symptoms in women with a pinched sciatic nerve
- Treatment of a pinched sciatic nerve
- What is Quadriceps Syndrome?
- diagnosis
Inflammation of the nerves (neuralgia) of the ankle nerve
The ankle nerve is the most unique nerve in the human body and holds a special place in the human nervous system. At the beginning of the last century, doctors realized that it was difficult to find an external or internal pathological factor that would not lead to damage to this nerve. It is its fibers that are the first to be damaged when disease develops.
The common ankle nerve consists of fibers from the fourth and fifth lumbar and first sacral spinal roots. It arises together with the tibial nerve at the point where the sciatic nerve splits in the back of the knee. This nerve then runs along the lateral surface of the knee, bypassing the fibula head and entering the origin of the piriformis muscle. Here the nerve begins to branch into internal and external deep and superficial branches. The sensory branches provide sensitivity to the skin of the hindfoot and lower leg. The motor branches are responsible for the peroneal muscles, the extensors of the foot and toes, and the pronation of the foot (the ability to rotate inward during movement).
Peroneal neuritis is inflammation of the peroneal nerve. It can be accompanied by pain (ankle nerve neuralgia).
causes
The most common cause of fibular neuralgia is pressure on the fibula caused by anatomical structures, usually near the bone head. Thickening of the walls of the anatomical tunnels can occur as a result of a general disease (gout, polymyositis, rheumatoid arthritis, diabetes, osteochondrosis, etc.).
Factors that contribute to the development of nerve inflammation (neuralgia) of the foot nerve:
- Trauma;
- Prolonged standing in a squatting position, kneeling;
- Acute and chronic infectious diseases;
- Poisoning from heavy metals, alcohol, etc.; – wearing tight-fitting shoes;
- Wearing tight-fitting shoes;
- Poor blood circulation in the legs due to thrombophlebitis or other diseases of the arteries and/or veins;
- tumors etc.
Anatomical and functional features
The oculomotor nerve consists of receptive and motor fibers.
It is responsible for sensing the skin of the foot and the outer surface of the shin. The muscle branches ensure the lifting of the foot upwards (extension) and the flexion of the toes.
Consequently, peroneal neuropathy or fibular syndrome leads to impairment of the functions described above. Either partially or fully.

causes
Neuropathy causes many problems due to the location of the tibial nerve because whether it is a compressional ischemic or post-traumatic disorder, the neuropathy makes movement difficult and immobilizes the person.
Among the causes that can lead to this pathological condition are:
- Actual damage, trauma. Direct rupture of the nerve bundle or its compression by scarred keloid tissue after lower leg surgery. Possibly with accompanying damage to the tibial nerve fibers.
- Neoplastic processes with localization on the lower limbs and in women with a gynecological profile. As the nodule grows, it metastasizes and compresses the nerve site. This impairs the ability to transmit signals to tissues.
- Toxic lesions that develop as a result of disease. Kidney failure, diabetes and alcoholism are common causes.
- vascular abnormalities. A lack of blood supply and the resulting lack of oxygen lead to ischemic damage and death of nerve endings and fibers and the loss of the ability to perform their function.

- Various types of infections.
- Staying in an extremely unfavorable posture for the lower limbs for a long time due to work or study. The uncomfortable posture leads to symptoms of tunnel syndrome (neuropathy) of the foot nerve.
Chronic diseases (diabetes), poisoning (industrial toxins and alcohol) lead to the death of nerve fibers and to polyneuropathy. This process is usually bilateral. Physical factors - trauma, tumor, poor posture - lead to a unilateral fibula syndrome.
Also, some systemic diseases lead to the development of sagittal neuritis as a complication. These include gout, rheumatoid arthritis and osteoporosis.
Causes and types of nerve damage
Causes that can trigger neck nerve disease:
- Trauma to the foot and leg, which then leads to nerve dysfunction (this can be a fracture, as there is a risk of nerve entrapment with this type of injury);
- Nerve compression can also lead to severe nerve damage;
- Excessive physical stress and overexertion can seriously affect not only the functioning of the body as a whole, but also that of nerve endings;
- neurological diseases;
- disturbed blood circulation;
- Tumors provoke nerve compression;
- excessive hypothermia or overheating;
- exposure of the body to toxins.
Primary and secondary disorders
The primary form of ankle nerve injury, which develops as a result of an inflammatory response, is independent of any other pathological process in the body.
This condition is most common in people who make heavy use of a single limb for long periods of time (eg, carrying most of their body weight on that limb or alternating legs at the gym). This type of pathology includes inflammation of the peroneal nerve.
Secondary nerve damage is characterized by a complication of the patient's existing disease.
The most common cause of severe damage to the ankle nerve is compression of the nerve, which is characteristic of the following diseases
- osteopathic diseases;
- benign tumors of bone tissue;
- synovitis;
- fractures and dislocations of the ankle;
- bruises of the limbs;
- tendovaginitis;
- inflammation of the inner synovial membrane;
- Deforming osteoarthritis - a chronic disease of cartilage and joint tissue;
- Bursitis peronei - inflammation of the joint capsule;
- Post traumatic arthritis.
clinical picture
Damage to the ankle nerve is characterized by the fact that it affects not only the feeling but also the function of the entire limb. Any disease of the ankle nerve leads to sensory disturbances, restricted movement, severe pain and general discomfort. The disease can develop as a result of the above causes (trauma, neuralgia and other injuries).
Ankle nerve damage can occur as a standalone or associated condition. A characteristic feature of ankle nerve damage is its gradual progression.
types of pain
Acute hip pain is caused by trauma and local inflammation. They can start on the right or left side, but as inflammation develops, it spreads around the waist and radiates to the lower back and legs. Your doctor will prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain quickly. However, sometimes it is necessary to continue treatment after the pain has subsided in order to eliminate the cause of the inflammation.
With nagging pain, it is more difficult for the doctor to make a correct diagnosis. They can appear in one area and recur in another. If they occur intermittently, it is important to pay attention to how they are expressed: at rest, when walking, when squatting, when making sudden movements.
If the pain symptoms last longer than six months, the disease has become chronic. To make the diagnosis, thorough examinations are carried out: X-ray, ultrasound, MRI and blood tests.
diseases and their symptoms
Hip pain can be caused by various diseases:
Bursitis is an inflammatory process that occurs in the joint capsule. It is manifested by acute pain, fever and a deterioration in general well-being. A hot lump forms under the skin that is painful to the touch. The condition is treated by an orthopedic traumatologist.
A chronic disease that destroys bone and joint cartilage. It is a chronic disease that occurs after trauma, during the menopause in women, in metabolic disorders, in excessive exertion in athletes and in heavy physical work. In the initial stages, there are signs of fatigue when walking and pain with fast leg movements. If chondroprotective therapy is initiated early, the progression of arthrosis can be significantly slowed down and the patient can remain active into old age. In the second stage, the destructive processes in the joint spread to the nerves. The pain comes on in the morning and subsides throughout the day. They can spread to the knees and lower back. Tissue swelling may occur. As osteoarthritis progresses, pain occurs around the clock and mobility is limited.
In coxarthrosis, the composition of the synovial fluid changes. It no longer lubricates the joint parts and there is severe pain, displacement and deformation of the femoral head with every movement. The disease develops in old age or after trauma. In the initial stages, a stabbing pain is felt when walking on the right or left side. When the nerves are compressed by the deformity, the pain increases and limping occurs. In the third stage, due to the deformation of the femoral head, there is a shortening of the left or right leg with a difference of 1-1.5 cm. The treatment of coxarthrosis is lengthy and consists of therapy with synovial fluid.
Treatment of anomalies
It is clear that treating symptomatic hip or knee pain alone is not warranted. Before treatment, a comprehensive diagnosis and examination is required, after which the doctor will make an appropriate diagnosis.
Depending on what specific condition has been diagnosed, the appropriate treatment for that condition will be prescribed. It is obvious that the treatment of a disc hernia or a vascular pathology proceeds very differently.
For example, with osteochondrosis, a complex of exercise therapy, swimming, physiotherapy and similar treatments is prescribed, most of which are used in the non-acute period of the disease. In the acute phase, the patient should behave calmly. A herniated disc should be treated in the same way, along with wearing a special brace and taking painkillers.
Treating a condition like thrombophlebitis requires hospitalization for the patient, and in some cases surgery is required to remove the clots discovered and reduce the health risk. The limbs must be rested, and restorative therapy and medication are required. Treatment of such pathologies alone can be fatal.
With joint pathologies, of which there are quite a number, the treatment depends on the exact diagnosis. For tunnel syndrome, the first treatment is symptomatic therapy to reduce pain and improve mobility. Until the treatment is completed, it is advisable to avoid exertion and rest on the injured limb.
Methods for pain relief
If the pain in the knee or hip is not caused by inflammation or other abnormalities, but is due to fatigue or excessive physical activity, which should first be determined by visiting a doctor, there are a number of methods that can be used to both relieve the pain and their cause can also be treated. These methods can be used if no concomitant diseases require additional treatment, or if the doctor approves their use in combination with other therapeutic methods.
At home, a warm, but not hot, bath can be taken, to which herbal preparations or herbs can be added to relieve the tension and relax the muscles. Among the herbs recommended for such ailments are chamomile, oak bark, calendula, linden, nettle, mint and others. In a separate bowl, pour boiling water over the harvest and leave for some time (about 15-20 minutes). Then use as directed. Essential oils can be used as an alternative to the plants themselves.
The use of compresses is also recommended.
Important: The affected parts of the body must not be heated under any circumstances. It is best to make a compress of ice cubes wrapped in a clean cloth or gauze, making slight movements and not fixing the compress in one place to avoid hypothermia.
A gentle massage using creams or essential oils should also be performed. The movements should be performed smoothly and easily to avoid damage. If an allergic reaction or skin irritation occurs, the massage must be stopped immediately.
And if you don't have the time or opportunity, here's a good idea: Lie on a level surface and put your feet up so they're above heart level. The easiest way to perform this exercise is to lie face up on the bed and lean your legs against the wall. Each leg in this position quickly restores normal blood flow and relieves any heaviness in the legs.
pain after injury
Muscle pain from minor injuries usually resolves within a week. However, if the pain persists for more than a week, you should see a physical therapist.
Muscle injuries include bruises (bruising) and sprains:
- First degree sprains (dislocations . A very minor injury that does not require treatment.
- Second degree sprains. A moderate injury characterized by pain, bruising, swelling, and muscle weakness. Healing of second-degree sprains can be accelerated with physical therapy.
- Third degree sprains. A serious injury that manifests itself as a muscle tear. A muscle tear causes pain, bruising, and weakening of the limbs. In this case, it is important to see a doctor, because only after the examination will it become clear whether surgery or mobilization (prevention of movement of the injured part of the body) is necessary.
A follow-up appointment with a physical therapist is also necessary as the rehabilitation plan prepared by this doctor will speed up the recovery process.
When to see a doctor for muscle pain
Muscle pain is not always innocent and harmless. In some cases, home treatment is not enough to eliminate the cause.
- The pain persists even after several days of home treatment;
- severe muscle pain occurs for no apparent reason
- muscle pain accompanied by a rash;
- muscle pain caused by a tick bite;
- the pain is accompanied by redness or swelling;
- the pain started after a change of medication;
- the pains are accompanied by fever.
Symptoms associated with muscle pain that require urgent medical attention:
- Sudden onset of swelling or decrease in urine output;
- Difficulties swallowing;
- vomiting or fever
- shortness of breath
- stiff neck
- muscle weakness
- Inability to move the affected limb.
Treatment
Pharmacological treatment
Pain-relieving treatment is primarily recommended, although NSAIDs may not be effective due to the non-inflammatory nature of the injury. Steroid injections are not always indicated (when injected directly into the tendon) because of the risk of tendon damage.
physical therapy
Physiotherapy is recommended for the treatment of temporomandibular joint disorders. Active therapy with an exercise program is preferable to a more passive treatment approach. Recovery varies greatly from person to person as the disease can be degenerative. In general, patients respond well to rehabilitation programs, but in some cases the tendons do not respond to a range of treatments.
It is recommended to strengthen the abdominal muscles to support the adductors during exercise and to do hip flexion exercises. The exercises should be tailored to the sport in question to avoid recurrence of the injury. In most cases, normal function can be restored within a few weeks, but in more severe cases, rehabilitation can take several months before normal, pain-free activity is restored.
treatment tactics
Rest is required for the first 48 hours after injury. Apply the RICE concept (rest, ice, compression and limb elevation) for 10-20 minutes three times a day to reduce swelling and inflammation. Once the swelling has gone down, therapy to stimulate blood flow can be started to speed up the healing process. Active therapy is then indicated to maximize rehabilitation. It is aimed at restoring muscle and tendon properties, since strength training has a positive effect on the structure of the tendon matrix, muscle properties and limb biomechanics. Recent evidence suggests that an eccentric exercise program is most effective. Eccentric and concentric exercises can also be done slowly with heavier weights to improve pain and tendon function. Cook et al. however, proposed a new 3-stage model of tendinopathy in which treatment with exercises differs between stages. They point out that the current treatment protocol with additional eccentric loading used in stages 2 and 3 may be detrimental to stage 1 tendinopathy. Determining the stage of tendinopathy is critical to effective treatment.
However, there is no single effective method for tendon rehabilitation, and the repetitions, approach, and load vary depending on the stage of rehabilitation and the response of the tendon muscles to the exercises. The exercises are designed to address the neuromuscular and tendon changes (strength and functional capacity) in tendinopathy.
The Cook et al. Suggested stages are reactive tendinopathy, tendon injury (failure to heal), and degenerative tendinopathy. In the early, reactive stages, the key is to bring the load to an acceptable level where the tendon can recover and heal. However, Cook points out that tendons can show a latent response for about 24 hours. That means what seems unresponsive immediately after an activity may become worse 24 hours later. The use of non-steroidal anti-inflammatory drugs is uncertain at this time, but it is suspected that they may be useful. Always consult your doctor before taking any medication.
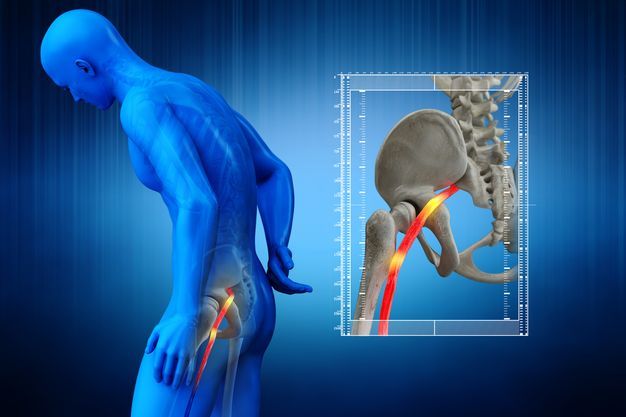
Symptoms and treatment of a pinched sciatic nerve
This condition is very painful and will not go away on its own. When the first symptoms appear, you should consult a specialist – a neurologist, neurologist or general practitioner. He or she will prescribe the necessary treatment and medication.
Symptoms of a pinched sciatic nerve
- Pain in the lower back, hamstrings, buttocks, or lower leg
- Discomfort when walking, putting your legs together, or bending your knees
- A feeling of heat in the toes
- Feeling cold in the area affected by the nerve
- Excessive sweating
- Impaired joint mobility – patients usually complain that they cannot straighten their leg
- Nausea in the extremities
- Feeling of goosebumps on the leg
- Discoloration of the skin on the affected area
- General malaise, apathy and weakness
- Elevated body temperature
Neurologists, neurologists and internists use these symptoms to diagnose a pinched sciatic nerve. If the specialist has doubts, the patient is referred for a CT or MRI scan to fully clarify the situation. The results are used to determine the diagnosis and treatment.

Symptoms in women with a pinched sciatic nerve
This condition can occur during pregnancy. During the second or third trimester, the enlarged uterus puts pressure on the pelvic muscles, causing contractions. The center of gravity of the expectant mother is shifted and the lumbar vertebrae are shifted. Also in the pelvic area, the growing head of the fetus presses on the sciatic nerve.
Between 40 and 80% of pregnant women complain of lower back pain. However, the cause isn't always a compressed sciatic nerve — it only occurs in 5 % of cases.
Doctors claim that the symptoms may disappear after delivery. Until then, however, you should not put up with the pain, it is better to consult a specialist in order to avoid serious consequences and aggravation of the pain.
Treatment of a pinched sciatic nerve
Most of the time, the pain comes on suddenly. Before you see a specialist, there are a few simple things you should do:
- Get into a comfortable and pain-free position. It is best if you lie on your back or on the unaffected side and keep the leg in which the pain occurs straight.
- If possible, avoid activities as any unnecessary movement can cause additional pain.
- Avoid old-fashioned treatments: put the heating pad aside and don't rub the painful area. This can make the pain worse.
- Take painkillers. These help numb the acute, excruciating pain. These are usually available in capsule or ointment form.
If the pain is severe and cannot be suppressed or relieved by analgesics, an ambulance should be called. Medical help is also required in milder cases. Your best bet is to see a neurologist, coroner, or general practitioner. Once the pain has subsided, you should see a doctor at your local GP office.
What is Quadriceps Syndrome?
Quadriceps syndrome is a condition that arises at the level of muscle fibers. Quadriceps psoas muscle syndrome is inherently a myofascial syndrome. This means that both the fibers themselves and the fascia, the connective tissue that holds them together, are affected. As quadriceps syndrome develops, small spastic areas form in the thickness of the muscle called trigger points. Under certain circumstances, these trigger points can lead to widespread painful spasms throughout the muscle. Like any disease, quadriceps syndrome has its characteristic symptoms, which we will now describe.
The symptoms arise from the activation of myofascial trigger points and are directly related to the function of the quadriceps muscle. This means that any movement involving this muscle can cause pain. However, unlike many other muscle pain syndromes, quadriceps symptoms are characterized by a paradoxical appearance.
paradox one. Anyone who has ever had back pain knows: if it hurts when standing, you need to sit or lie down, and if it hurts when lying down, on the contrary, you need to get up and stretch. In contrast, the quadriceps hurt both vertically and horizontally. Especially discouraging is the fact that the quadriceps hurt even at rest. Therefore, to relieve pain, patients do not lie down, but rest their hands on their own thighs, the armrests of a chair, or the seat of an armchair [ibid., Vol. II, p. 1]. 43]. This is very characteristic of the quadriceps muscle. In this way, the patient relieves the muscle from the strain of the upper body. In particularly severe cases, this does not help either. Then only one thing remains: the movement on all fours. The quadriceps position does not require stabilization of the spine by the quadriceps [Ibid. Vol.II.C. 34].
Second paradox. If the pain occurs during unfortunate bending, lifting weights or other awkward movements, the cause of these quadriceps symptoms is clear, it is superficial, and experienced patients try to avoid such situations. However, when the pain occurs as part of normal everyday activities, it is an unpleasant surprise. Cooking a meal, washing the dishes - what's in it? But here's the catch: habitual activity leads to fatigue in the same areas of muscle tissue. And that's already a direct route to trigger points and other quadriceps problems.
diagnosis
Diagnosing quadriceps syndrome requires extensive knowledge on the part of the doctor. And these are not pretty words, but the prose of life. Remember we said that the quadriceps of the back is a wild card that can mime and mislead. It is therefore very important to be able to distinguish this syndrome from similar pathologies. In general, the ability to distinguish between different diseases is an essential skill of the physician, known as differential diagnosis. In this case, to be able to say with certainty that it is Quadriceps Syndrome and not some other pathology, the doctor needs to know what is reflected in the pain, associated muscles, satellite trigger points and more. But to go through all of this in order.
Quadriceps psoas muscle syndrome manifests itself as rebound pain. This means that where you feel pain, the source of the pain is not there but somewhere else. And the realm of pain is just a reflection, like a rabbit in the sun. It must be admitted that catching the sun hare is impossible; he is elusive. The only way to get rid of him is to cover the mirror in which he is reflected. There is no point in acting on reflected pain points. You have to look for the triggers and eliminate them. You are the real source of the pain.
There are four areas that are specific to quadriceps syndrome. But that doesn't mean that it has to hurt everywhere at the same time. The pain may be in one or more of the following areas, or it may migrate from one area to another.
- Upper buttock, along the iliac crest; Lower abdomen, groin and external genitalia.
- The area around the hip joint; the intensity of the pain can be so strong that lying on the side is impossible.
- The sacroiliac joint, or in bilateral quadriceps syndrome, the pain spreads to the lower back.
- Lower buttocks, deep in the buttocks.
Sometimes, in addition to the areas of rebound pain, there are also associated trigger points. These are activated reflexively along with the main trigger points, but the pain they emit can be much more severe than that of the main trigger points. In quadriceps syndrome, the associated trigger points are in the gluteus medius. They cause pain along the sciatic nerve.
Read more:- tibia and fibula.
- extension and flexion of the foot.
- Why do your calves hurt when you run?.
- The muscles that move the foot.
- Calf muscle cramps when walking.
- Acute pain in the calf muscle when running.
- Orthopedic knee orthoses for osteoarthritis when walking.
- Shuffling Feet While Walking Causes.
