A doctor should be consulted if soft tissue swelling persists for more than 2-5 days or if severe and persistent pain occurs. A specialist consultation is required if the pain in the foot is accompanied by a sharp increase in temperature. An appointment will be made if pain increases and structural changes occur.

- Pain in the hoof nail bone
- Class A: Fractures of the calcaneus
- Methods of fracture diagnosis
- Treatment options for metatarsalgia
- What is the upper ankle joint?
- What is the significance of syndesmosis in the upper ankle?
- Pain in the heel bone of the foot
- Pain in the hindfoot with osteochondropathy of the heel bone – Köhler I disease
- causes
- symptoms
- Causes of Keller disease
- Symptoms of Keller's disease
- Osteochondropathy of the navicular bone (Köhler I disease)
- Osteochondropathy of the heads of the metatarsal bones (Köhler II disease)
- Possible causes of pain
- Anomalies in which the arch of the foot hurts on the inside
- Symptoms of osteoarthritis in the foot
- Classification of foot diseases
- Diagnosis of joint pain in the feet
- Treatment of pain in the bones of the foot
Pain in the hoof nail bone
tarsus is the least mobile part of the foot and consists of the scaphoid, the cuboid and the three sphenoid bones. Typical injuries include multiple fractures or dislocations. The most common fracture of the navicular bone involves its dorsal lip. The second most common is a fracture of the sphenoid bone, followed by a fracture of the shaft of the navicular bone, which can be transverse or horizontal. Fractures of the elbow and sphenoid bone usually occur together and are usually the result of pressure injuries.
Fractures of the tarsal bones are classified according to anatomical principles:
Class A: Fractures of the calcaneus.:
– Type I: dorsal separation fractures
– Type II: tuberosity fractures
– Type III: shaft fractures
– Type IV: compression fractures
Class B: ankle and wedge fractures:
– Type I: fractures of the ulna
– Type II: fractures of the sphenoid bone

Class A: Fractures of the calcaneus
Detached fracture type I is usually the result of a quick flexion with inversion of the foot. This causes overstretching of the heel bone joint capsule and may result in separation of the dorsal surface of the heel bone. A type II tuberosity fracture usually occurs when the foot is abruptly extended. The eversion of the foot leads to strong tension in the tendon of the tibialis posterior muscle, which can detach the tuberosity portion of the navicular bone. Type III shaft fractures and type IV compression fractures are rare.
The aforementioned already mentioned Mechanisms of injury include rapid hyperextension with compression, direct trauma, or hyperflexion with rotation.
The patient complains about Painsand swelling and tenderness around the injury site. In detached fractures, pain occurs on the dorsum and inner surface of the metatarsal bone. With cusp fractures, localized pain occurs over the injury site, which increases when the foot is extended.
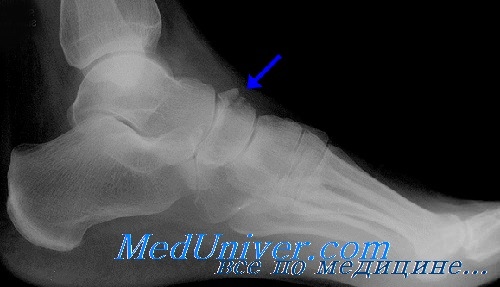
To prove fractures A fracture of the navicular tuberosity is best recognized by straight, lateral and oblique x-rays. A mild fracture without displacement can be difficult to diagnose. Comparison projections or dynamic images are required for precise determination. The accessory bone, the external tibial bone, can often be confused with a detached fracture of the navicular bone.
Dorsal detachment fracture is often associated with fractures of the ligaments of the lateral malleolus. A fracture of the hump is often accompanied by a fracture of the elbow.
Methods of fracture diagnosis
A good diagnosis is the key to appropriate and effective treatment. Diagnostic measures will help you understand what is causing your pain and how to treat it.
If you suffer from metatarsal pain and don't know which doctor to see, you should first consult your family doctor, who can refer you to a specialist after an examination.
Diagnosing the cause of metatarsal pain takes several steps. The first step is an initial medical examination. During this examination, the doctor will pay attention to the following important points:

Many doctors will also ask the patient to leave during the appointment. At this appointment, the nature of the gait can be assessed and even (not always, but in some cases) a preliminary diagnosis can be made.
After the initial examination, the patient is always referred for an instrumental examination. With their help, the clinical picture can be analyzed in more detail and the condition of the tissues and bones of the foot can be examined from the inside. The list of commonly performed instrumental examinations includes:
- X-rays. In this procedure, images of the foot are taken in two projections. The images can be used to determine whether bone and joint deformations are present and how severe they are.




Treatment options for metatarsalgia
Depending on the exact cause of the pain in the arch of the foot, the patient is referred to a specialist. If the symptom is due to trauma, it will be treated by a trauma surgeon; if it is due to arthritis or other musculoskeletal disorders, it can be treated by a rheumatologist; if it is due to a neurological disorder, it can be treated by a neurologist. In some cases, more than one doctor may be needed at the same time. The type of treatment also depends directly on the type of impairment. This could be:
- physical therapy. It is prescribed for abnormalities that are not very serious and do not require major medication or surgery.



In addition to the basic treatment methods, supportive therapies are also used. This includes wearing special orthopedic shoes and orthoses.
To relieve pain, improve blood circulation and metabolism, and correct curvature, doctors recommend walking barefoot on grass and sand. This treatment is effective for both additional pain relief and prevention.

What is the upper ankle joint?
The upper ankle joint consists of three bones - the tibia, the fibula and the talus.
The mobility of the upper ankle joint lies between the ankle joint bifurcations and the talus. The ankle joint fork is formed by the outer ankle bone (fibula) and the inner ankle bone (tibia). It creates a springy position for the ankle bone. The forks of the ankle joint are U-shaped and are held together by ligaments. This bridge of tight connective tissue - the syndesmosis - is the main part that provides support at the front and back. The upper ankle joint is also called the tibial joint because these two bones bear the majority of the weight. The ankle joint is the syndesmosis on the side.
Below this is the term syndesmosis. It is located between the tibia and the fibula.
What is the significance of syndesmosis in the upper ankle?
The forks of the ankle joint are U-shaped and are held in place by ligaments. This bridge of tight connective tissue – the syndesmosis – is the main part that provides front and back support. A distinction is made between anterior and posterior syndesmosis. Syndesmosis is important when evaluating ankle injuries because the strength and position of these two bones is critical to good joint function.
Like all joints, the ankle joint is surrounded by a joint capsule. The ankle joint is also supported by ligaments. These ligaments stabilize the joint depending on the position of the ankle and the anatomical course of the ligaments.
Pain in the heel bone of the foot
Pain in the back of the foot with inflammation of the deep nerve of the talus. In this condition, the pain occurs after damage to the nerve of the deep ankle joint, most commonly from a bruised hindfoot. In the back of the foot, the nerve is superficial and lies under the cruciate ligament of the foot, where it is virtually unprotected from injuries caused by poorly fitting shoes or by crushing. This nerve supplies sensory fibers to the space between the first and second toes, and the patient experiences neuritic pain radiating to this area.
Rearfoot pain in ski boot compression syndrome. With the increasing popularity of skiing, a new complication has been described in which the ankle joint is pinched by the tongue of the ski boot, causing deep peroneal nerve inflammation and extensor tendon synovitis. On examination, the patient has thickening, and gentle palpation causes severe pain on the dorsal surface of the foot. There is little or no sensation between the first and second toes, while the rest of the foot is less sensitive. Dorsiflexion is significantly limited due to extensor tendonitis, but the pulse in the dorsal artery is normal.
The treatment includes elevating the extremity, ice packs, and mild pain medication. The process usually resolves within 36 hours, but tenderness may not be restored after four weeks. In refractory cases, steroid injections are recommended.
Pain in the hindfoot with osteochondropathy of the heel bone – Köhler I disease
heel bone is susceptible to aseptic necrosis because the ossification process in the navicular bone is completed later than in other bones. Necrosis usually occurs between the ages of 4 and 6 years and is often bilateral. In this disease, painful claudication is observed. The etiology is unclear, but the process is usually self-limiting and usually resolves spontaneously.
causes
The disease occurs as a result of a number of causes that lead to impaired blood circulation in the foot area. The main causes are various types of trauma to the foot and constant wearing of tight and uncomfortable shoes of the wrong size. Keller's disease can develop in people who have... arthritis, osteoarthritisThe disease is also caused by a number of diseases related to endocrine and hormonal disorders. A hereditary predisposition to the development of the disease is also an important factor in this case. Acquired or congenital foot defects (most common flat feet) can also lead to the manifestation of the disease. Another important factor is metabolic disorders in the human body. However, experts point out that the exact causes of osteochondropathy are not yet finally known.
Doctors who diagnose Keller's disease define two types of the disease, depending on which bones are affected.
When a person is diagnosed with Keller's disease 1The meniscus bone in the foot is affected. This bone is located on the inside of the foot. Keller's disease 2 manifests itself through pathological changes in the heads of the second and third metatarsal bones. These bones connect their articular surfaces to the phalanges of the toes. Keller's disease grade 2 occurs more often in adolescents.

In addition, doctors divide the course of the disease into several stages when determining the symptoms of osteochondropathy. Under the stage of necrosis The patient suffers from the death of the bone ridges, which are the structural elements of the bone. These changes are pronounced and can even be seen in photos. Under Compression fracture stage New bone elements are formed, but they are not yet strong enough. During this phase, the bone beams are often unable to withstand the heavy load. As a result, fractures occur and the beams can wedge each other. The next stage Fragmentation phaseThis is followed by the fragmentation stage, in which the osteoclasts (bone-degrading cells) promote the breakdown of the bone bars. The final stage – is the process of restoring the shape and structure of the bone. The answer to the question of how to treat the disease directly depends on what stage of the disease you are at. Therefore, treatment of Keller's disease can only be initiated after an accurate professional diagnosis.
symptoms
Keller I disease It is most commonly diagnosed in preschool boys between 3 and 7 years old. Initially, the child notices pain and signs of swelling on the back of the inner edge of the foot. Due to the pain, the child constantly limps and tries to walk resting on the opposite, outer part of the foot. Usually only one foot is affected. The condition lasts for about a year, after which the pain gradually subsides.
Keller II disease (Keller II disease) is most commonly diagnosed in adolescent girls. It was first described by Freyberg, an American trauma surgeon, and Keller studied and described this form of the disease in more detail. This form of the disease often occurs on both sides. The onset of the disease usually goes unnoticed. The pain initially occurs in the area of the head of the 2nd or 3rd metatarsal bone. metatarsal bone. The pain initially occurs when the forefoot is put under strain and later when the foot is at rest. Gradually, a limp may develop, the patient cannot walk in thin-soled shoes, and walking barefoot is very difficult, especially if the ground is uneven. The swelling occurs where the pathological process develops, namely on the posterior surface of the foot. The toe next to the head of the affected bone becomes shorter and movement in the joint is restricted. All of these symptoms persist for about two years, after which the pain gradually subsides. However, if the joint changes during this time, the pain may soon return. Familial cases of foot involvement are occasionally diagnosed. The disease is usually limited to the head of the 2nd or 3rd metatarsal bone; rarely several bones are affected.
Causes of Keller disease
- Inherited predisposition to ischemic processes in the lower limbs
- Abnormal anatomy of the foot due to flat feet
- Constantly wearing unsuitable footwear
- Bone damage
- Recurrent foot injuries
- dislocation of the ankle
- Bone damage
Abnormalities in the metabolism and endocrine systems also affect the foot. These include hypothyroidism, obesity and diabetes.
Symptoms of Keller's disease
The symptoms of bone necrosis in the foot area depend on the type of disease. Pain syndrome is the main complaint of patients with this diagnosis. Keller disease type 1, which affects the scaphoid bone, causes the following additional symptoms:
- Swelling of the foot with swelling on the back of the foot
- Increased pain when walking or palpation
- To relieve the pain in the foot, the child leans on the outer edge of the foot
- Gait disturbance
- Change in the shape of the heel bone
The second type is characterized by necrosis of the metatarsal bone. In addition to pain, there are changes in gait and swelling, and the discomfort increases when walking or wearing tight shoes. Keller disease type 2 is most commonly diagnosed in girls ages 11 to 16. Type 1 is typical for boys aged 3 to 7 years. This pathological condition is not characteristic of adult patients.
Osteochondropathy of the navicular bone (Köhler I disease)
The disease most commonly occurs in boys ages 3 to 10, and sometimes older. Both unilateral and bilateral lesions of the navicular bone can occur (most common). In adults, navicular bone lesions have developed into an independent nosological form of aseptic necrosis, called Müller-Weiss syndrome (disease). There are differences in the pathogenesis of the disease in children and adults.
Aseptic necrosis in children is explained by a disruption in the ossification process of the navicular bone, which is confirmed by X-rays: there is an increase in density, a flattening of the ossification nucleus, which consists of several fragments. Normally, the number of ossification nuclei of the navicular bone should not exceed two. Another characteristic sign of the disease is an enlargement of the intercostal space that separates the navicular bone from the talus and ischium, visible on x-rays. The space around the navicular bone is resolved by reducing its size in the anteroposterior direction.
Aseptic necrosis of the navicular bone in adults is most often caused by trauma to the foot, less often by other causes (consequences of overloading the foot in athletes, workers, etc.). In this case, aseptic necrosis affects not the ossification nuclei, but the already formed bone . The lesion of the navicular bone is often associated with flat feet, foot and toe deformities. The disease should be differentiated from a bone fracture, an isolated tuberculous lesion, or an inflammatory process.
Regardless of the cause of the disease, the clinical manifestations of aseptic bone necrosis are the same: there is strictly localized pain when pressing on the bone and when walking; There is a limp and limited movement in the ankles.
In children, treatment is limited to relieving the pressure on the foot and immobilizing it (in orthopedic shoes, if necessary with a plaster boot).
Pain relief is achieved through heat and massage. The bone structure rebuilds itself within 1.5-2 years. In adults, these measures may not be enough to achieve a cure. In such cases, arthrodesis of the ankle joint is indicated.
Osteochondropathy of the heads of the metatarsal bones (Köhler II disease)
According to the literature, aseptic necrosis of the heads of the metatarsal bones accounts for 0.22 % of all orthopedic diseases. It is one of the most common locations of osteochondropathy. It occurs between the ages of 10 and 20, mainly in women.
In addition to the typical Kähler II location, atypical lesions (multiple bilateral lesions on the heads of metatarsals IV, I, V) are sometimes also found on the heads of metatarsals II and III. Characteristic of the multiple heads of the metatarsals is the presence of static foot deformities: longitudinal and transverse flat feet, flat foot deformity and valgus deformity of the first toe. Many patients also show signs of dysplastic development.
Clinically, there is swelling and pain in the area of the affected metatarsal heads, and the mobility of the metatarsophalangeal joints is limited. The radiological picture depends on the stage of the process. The destructive changes lead to bone remodeling, fragmentation, flattening and deformation of the heads. In the final stage of the disease there are signs of deforming osteoarthritis with typical bone hypertrophy in the head area and minor changes at the base of the phalanx.
Many patients achieve complete clinical and radiographic recovery. Transformation of osteochondropathy into deforming osteochondritis is not at all necessary if repeated trauma to the foot is excluded. A favorable outcome occurs when the primary necrosis is not complicated by a fracture. This is not always avoidable.
Unilateral metatarsal head lesions often result in excessive loading of the other foot, sometimes leading to pathologic remodeling of the metatarsal bone (Deichlander disease). These patients only become aware of a history of Kähler II disease many years later during an x-ray examination for foot pain due to the development of Deutschländer disease.
Possible causes of pain
Attempting to resolve arch pain from within often only makes the condition worse. In order to alleviate the unpleasant symptoms, the cause of the pain must be correctly diagnosed - only a doctor can determine this.
- Inflammatory diseases;
- mechanical trauma;
- Weakening of the ligaments or joints;
- degenerative-dystrophic pathologies;
- various types of foot deformities;
- autoimmune abnormalities;
- metabolic disorders;
- long-term trauma;
- Other diseases.
The appearance or worsening of arch pain on the inside of the foot is often triggered by the following factors:
- hypothermia (including wearing inappropriate, lightweight footwear);
- uncomfortable footwear;
- Excessive exposure to sporting activities;
- Hormonal imbalances;
- Obesity;
- hypodynamia;
- injuries;
- infections;
- unbalanced diet (including weight loss diets);
- Persistent fatigue; Lack of sleep;
- dehydration;
- Exacerbation of chronic diseases.
If you are or have been affected by any of these factors, you should definitely mention this when you visit your doctor.
Anomalies in which the arch of the foot hurts on the inside
Rapid fatigue and pain in the feet are characteristic of clubfoot, flatfoot and other similar diseases. The risk of foot deformity is increased by wearing shoes with very high heels and flat soles.
From the age of 30, the risk of osteoarthritis increases. This is a disease that leads to the gradual destruction of cartilage tissue, including in the ankle and toe area. Mild discomfort eventually develops into severe pain. The pain develops gradually and becomes more and more severe:
Arthritis is an equally dangerous condition. It is accompanied by persistent inflammation (infectious or non-infectious) that attacks the cartilage tissue. In infectious arthritis, the inflammation develops rapidly and leads to severe swelling and deformation of the foot and fever. It is usually preceded by another illness, such as: B. an acute respiratory infection, flu, strep throat or food poisoning.
Gout, a disease caused by an imbalance in purine metabolism, can also cause pain on the inside of the foot. Gout often causes tophi – lumps with a thick, whitish fluid inside. The uric acid crystals build up around the joint, injuring the tissue, causing swelling and inflammation, and deforming the foot. Gout often causes pain in the ball of the foot on the inside of the foot. Another common side effect of gout is severe pain that occurs suddenly, usually at night, and is accompanied by swelling and blue discoloration of the skin. After a while the pain goes away on its own, but without treatment the attacks become more frequent.
The inside of the foot can be affected by inflammatory diseases such as ligament inflammation and tendonitis. In the first case, the ligaments are affected, in the second case, the tendons. Both conditions can be caused by wearing uncomfortable footwear, tissue immobility, trauma, chronic illness (especially diabetes), and obesity.
Symptoms of osteoarthritis in the foot
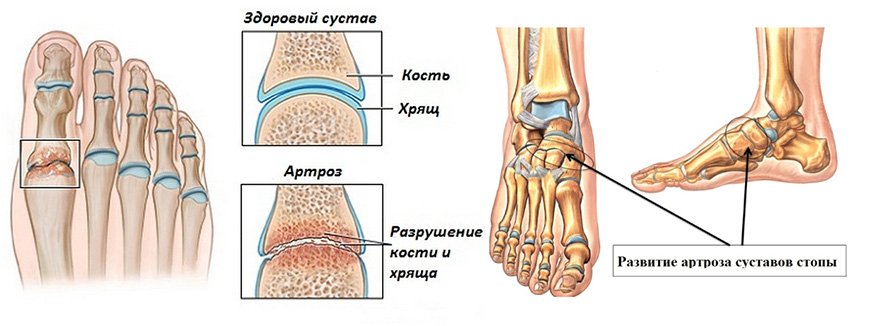
A very important question arises for all doctors: 'How can osteoarthritis in the foot be recognized?
The disease is betrayed by the following symptoms:
- Pain syndrome during long walks, in an upright position and after great exertion.
- Swelling or redness of the skin in the affected area. Sometimes there may also be an increase in body temperature.
- The joint reacts painfully to changes in the weather and also to contact with cold water.
- The feet crunch (this is typical for the second stage of the disease).
- Your feet get tired quickly.
- Stiffness in the feet in the morning.
- Blisters form on the soles of the feet.
Since the disease causes deformation of the joints, the patient usually has gait problems in the later stages.
In addition, arthrosis of the foot is characterized by the following symptoms:
- Pain – may be itching or burning;
- bone hypertrophy in the form of osteophytes;
- Thickening of the ankles.
Since the disease affects not only cartilage and bone fibers, but also muscle tissue, the symptoms of foot osteoarthritis also include changes in muscle structures and fibrosis.
Classification of foot diseases
As already mentioned, the foot is made up of many small joints. For this reason, a destructive tendency can occur in any part of the foot. Osteoarthritis of the foot is divided into different types depending on its location. Specifically, these are:
- subtalar ligament disease;
- Diseases of the ulnar-carpal joint;
- Pathology of the metatarsophalangeal joint and ligaments;
- Osteoarthritis of the finger joints.

According to the source, depending on the stage of development, osteoarthritis is divided into the following types:
- Primary. It occurs as a result of a pathology in the foot itself or as a result of damage to the foot.
- Secondary. It is caused by diseases that are not directly related to the foot. Endocrine and other disorders can be the cause of the disease.
- Polyarthritis. In this disease, several joints are affected at the same time.
Depending on the type of joint destruction, the doctor selects a specific package of measures.
Diagnosis of joint pain in the feet
Before treating the disease, it is necessary to carry out a diagnosis and make an accurate diagnosis. The doctor will determine the source of the pain and its cause and clearly identify the problem caused by it. If symptoms suggest the development of osteoporosis, densitometry is recommended. This test measures bone density in the areas where pain is most severe.
If there is pain in the bones of the foot, an X-ray examination of the painful area, an ultrasound examination of the joints and soft tissues and, if necessary, an MRI examination are indicated. The latter examination is carried out in a maximum of 20 % cases when previous diagnostic methods have not given an objective picture of the anomaly.
The patient may also be prescribed a blood test (OAB, complete blood count, biochemistry, sugar) and urinalysis (general analysis). Since each case is unique, the ordering of the examinations is discussed upon initial admission, explaining the patient's history and symptoms. In the clinic of Dr. Long is prescribed only the tests and examinations necessary to determine the nature of the impairment and make a diagnosis.
Treatment of pain in the bones of the foot
Self-treatment is not acceptable. A consultation with an orthopedist is required to prescribe painkillers. It is strictly forbidden to take painkillers and continue to put pressure on the foot as before. The load on the foot must be reduced. The following therapies are used for this pathology:
- Chiropractic and osteopathic treatments.
- Administering painkillers and anti-inflammatory medications.
- Selection and individual production of orthoses.
- Physiotherapeutic techniques, therapeutic exercises, massages.
- Kinesio taping, shock wave therapy (UWT).
The innovative DiTasin therapy is used in the clinic by Dr. Long applied. Surgical intervention is recommended only in the most extreme cases, when other methods have not produced the desired result. An appointment at our clinic can be made by telephone. We offer free medical advice and diagnostics.

We are recommended by 94% of patients.
We thank you for your trust and your choice.
- Completion of the scaphoid on the foot.
- The tarsal of the foot.
- Fracture of the calcaneus of the foot.
- Cracked metatarsal.
- Fracture of the 5th metatarsal.
- Bone structure of the navicular foot.
- tarsal bones of the foot.
- Heel bone tendon sac in Latin.
