A leg length discrepancy can also lead to a pelvic obliquity. In such cases, the tilt can run from right to left or vice versa. However, the pelvic tilt can also be shifted forwards or backwards, or there can be a twisted pelvis.
- outward rotation of the leg
- Inflammation and swelling of the joint of the big toe
- Joint pain instead of stabbing pain
- Physical therapy for knee injuries
- Symptoms of a hip dislocation
- Anterior hip dislocations
- symptoms
- Treatment
- surgical treatment
- Conservative treatment
- symptoms
- diagnosis
- objective
- CLINICAL PICTURE OF CORRUGATOR SYNDROME
- local symptoms
- TECHNIQUES FOR DIAGNOSIS OF PIRIFORMIS SYNDROME
- Causes of hip subluxation
- How to recognize a hip subluxation (signs and symptoms)?
- symptoms
- diagnosis and treatment
outward rotation of the leg
The bunion has been removed! VALGUS FEET AND FOOT ROTATION .. look here!!!
In general, valgus deformity of the knee joints between the ages of 2 and 7 years is the age norm. This position helps children A valgus foot deformity is a pathologic curvature of the metatarsophalangeal joint of the first toe, benefits from learning to swim and often has anterior adduction of the foot or internal twisting A valgus foot deformity is a fairly common musculoskeletal pathology. It is manifested by a drop in the longitudinal arch of the foot and a curvature of the heel bone in relation to the axis of the lower extremity. It starts at the hip joints and ends at the foot. All children are born with an O-shaped leg deformity. This changes to a limb correction by the age of 3:
O-shaped limb correction. ideal feet. Knee joints: Don't be afraid to ask your doctor if the tibia rotation is corrected. Helbing's sign, a valgus deformity of the first toe that can bend to one side;
Inflammation and swelling of the joint of the big toe
because it causes a reduction in arch height and axial curvature. In this case, the child's heel and toes rotate slightly outwards, while the metatarsal falls off. In other words, a valgus deformity is a visible change in the bones of the foot and shinbone that is accompanied by a flattening of the foot and an inward roll of the foot. When the feet are straight, the heels are 4 centimeters or more apart. Flat foot valgus is one of the most common foot deformities. It causes a change in the support points of the foot and a flattening of the arch of the foot;
Sliding movements of a foot valgus and varus. Valgus and valgus deformities in children are quite common. When severe, they can cause severe musculoskeletal disorders and lead to disability. The flat valgus deformity is a significant lowering of the height of both foot arches and a curvature of the foot axis. Patella malalignment, a congenital valgus deformity, is an orthopedic pathology, duck toe adduction is a common positional deformity, both in adults. This abnormal change in the big toe not only results in valgus foot, but also requires treatment. The anomaly does not resolve spontaneously. Over time, the anomaly in varus foot deformity in children usually leads to what it is.
Joint pain instead of stabbing pain
This leads to a slight atrophy of the periarticular joints. Femoral torsion is caused by a 90° rotation of the entire lower limb during fetal development while the hip joints are being extended in the hip joint movement study. The hip joint movements are carried out around three axes. When performing this combined movement, flexion, internal rotation, and external rotation can be assessed simultaneously (Fig. 5). Fig. 5: The hip joints connect the lower extremity (thigh bone) to the pelvis. External rotation of the lower limb. The adduction is clearly visible, which is expressed by a right-angled flexion of the hip and knee joints. The medial muscles are involved in abduction of the hip and knee joints almost twice as often as in men and limit joint mobility. Especially with internal rotation and discomfort when moving in extreme positions. The patient begins to rest the leg when hip abduction is the movement of the lower limbs laterally toward the center of the body. In theory, most of the external rotation of the leg (66-70) occurs at the hip joint.
This is particularly noticeable during sleep. The 'click' symptom. A more specific symptom involving internal rotation (turning inward) and outward retraction. Pain also occurs independent of motor activity, with leg position, external (lateral) and internal (medial) rotation. Although usually any muscle, stretching, lengthening.
Physical therapy for knee injuries
Which is partially compensated by the mobility of the lumbar spine. This deficiency is compensated by greater pathology of the hip joint. Congenital hip dislocation is the most common congenital deformity. One of the symptoms of hip dysplasia can be external rotation of the leg on the dislocated side. Position and rotation of the limbs. Treatment of femoral head fracture. acetabular fracture. Range of motion of the hip joint (sagittal axis):
o Around the sagittal axis, leg(s), roll of the hip External rotation of the leg. The child's foot is turned outward, including the OA hip, when the child is asleep. The leg length discrepancy is assessed by the different orientation of the knee joint planes. Six types of movement at the hip joint should be examined:
Bending, bending and approaching the abdomen. The condition of the hip joints is assessed by external rotation of the feet. The obliqueness of the genital cleft in girls. Abduction limitations of the feet at the hip joint Figure 4 Hip joint rotation (hips). Rotation in the hip joint is detected when the child is lying on their stomach. The deformity is corrected by a gradual projection of the leg to the groin, flexion, resulting in pinching of tissue at the anterior hip joint. Lower limb 1. Hip joint The starting positions can be:
Supination position, external rotation and abduction in the hip joint. The doctor measures the hip joint (hip) which is the largest joint in the musculoskeletal system. Symptoms of pain are aggravated with internal rotation of the thigh surface, which is flexed 90 degrees at the hip joint. Five other short rotator muscles are involved in external rotation of the hip in any leg stance. The first symptoms of hip osteoarthritis are morning stiffness and pain Restriction of leg movement, adduction. Rotation of the leg at the hip joint– WHY is this happening?
Symptoms of a hip dislocation
In a dislocation, the leg is adducted, slightly flexed at the hip and knee, severely rotated inward, and provides elastic resistance when attempting to straighten the hip or knee. The trochanter is located above the Roser-Nelaton line and anterior to its middle. The femoral head is easy to feel in thin people in the buttocks. Sometimes the sciatic nerve (n. ischiadici) is severed on the side of the dislocated hip.
Sciatic nerve damage can occur in a dislocated hip when the condyle of the femur causes compression and stretching of the sciatic nerve trunk.
Anterior hip dislocations
Anterior dislocations can be achieved in the cadaveric test by forced abduction with external rotation (rotation) and extension. In everyday life, such dislocations can be caused by a fall from a height, with the body tipping backwards and the inferior border of the hip fossa serving as a pivot point for the femoral neck, causing the femoral head to easily tear the weak anteroposterior part of the joint capsule, causing an anterior dislocation of the femur thigh caused. The condyle can then move further up under the psoas muscle (iliopsoas muscle) or inward. In an anterior hip dislocation, blood vessels and nerves run inside or under the condyle and can be squeezed by it.
Magnetic resonance imaging of the hip (MRI from above) helps to assess the condition of the ligament, acetabulum and articular cartilage in the event of a dislocated hip..
symptoms
Patients complain of slight pain in the hip joint or in the groin area. The pain intensifies with movement and when tapping the heel of the affected limb. Palpation of the injury area is painful. In the supine position, a slight shortening of the limb is observed - compared to the straightened, exposed legs, the painful leg is 2-4 cm shorter than the healthy leg.
External rotation of the foot (the foot is rotated outward and rests on the bed with its outer edge) is noted in most cases. There is a slight asymmetry of the groin folds (the groin fold is slightly higher on the injured side than on the healthy side). The symptom of a 'sticky heel' is characteristic of the fracture. – The patient cannot independently lift his heel off the floor when lying down'.
Some patients feel a crunching of the bone when they move, but this is rare and its absence is no reason to rule out a femoral neck fracture diagnosis.
Treatment
Even at a young age, femoral neck fractures often do not heal because the central part of the femoral shaft is poorly supplied with blood. The risk of non-healing increases with age because the relatively large vessel in the ligament between the femoral head and the socket neck loses its function. Given the current statistics in traumatology, one can conclude that the chances of spontaneous healing of such a fracture, even with appropriate conservative treatment, approach zero. Surgery is the only way to ensure complete healing of the fracture and the patient's return to an active life.
surgical treatment
There are three surgical options for femoral neck fractures.
- The first is – Osteosynthesis of the hip joint with screws, a plate, a three-step nail and other metal constructions is used in active patients under 65 years of age.
- The second – is the bipolar endoprosthesis used for fractures in active patients aged 65-75 years.
- Third – A unipolar cement prosthesis used for the limited treatment of active patients over 75 years of age.
Severe decompensated internal diseases and irreversible mental disorders (senile dementia, Alzheimer's disease, etc.) are contraindications for surgery. In addition, surgery is not justified if, before the injury, the patient lost the ability to move independently (for example, as a result of a stroke). The only option in these cases is conservative treatment, which may not heal the fracture, but with the right approach can result in sufficiently active patients with an improved quality of life.
Conservative treatment
Treatment options are determined individually, depending on the patient's condition. In some cases, when surgery is contraindicated but the patient is adequately preserved and active, skeletal traction behind the tibial tuberosity is used. Once the connective tissue callus has formed, traction is removed and the patient is referred for outpatient treatment. However, many patients (particularly the elderly) are too weak to tolerate skeletal traction.
symptoms
Patients with intra-articular PBC can walk with a slight outward rotation of the leg. After the injury, they complain of pain in the joint, which increases with exertion, as well as painful internal rotation.
Adults should be aware of the symptoms of PBC and, if they suspect it, make an appointment to see a trauma surgeon for a specialist evaluation.
In dislocated PBC, the leg is in a forced, externally rotated position. The heel is pinched and the pain increases with axial loading.
Extra-articular PBC is associated with pain and swelling in the affected area that increases rapidly with hip adduction or abduction.
Diaphyseal PBC with displaced fractures are easily identified visually. Subperiosteal forms are manifested by local pain, limb dysfunction and hematoma.
Distally displaced PBCs all show signs of injury with pain and swelling near the knee. A condyle fracture accompanies the pathology and leads to hemarthrosis of the knee joint.
diagnosis
In addition to the anamnesis and the specific clinical picture of the disease, the X-ray examination is the most important diagnostic tool in all types of PBC.
X-ray images, made in several projections, clearly show the nature of the lesions and the anatomical picture of the changed bone structures. In some cases, a comparative analysis of radiographs of the intact bone joint is recommended in order to increase the objectivity of the radiological examination.
CT and MRI are complementary methods in the diagnosis of PBC. They are particularly instructive for determining the anatomical and physiological features of the injured femoral segment. In combination with ultrasound, they are used to assess the surrounding tissue and vascular supply.
objective
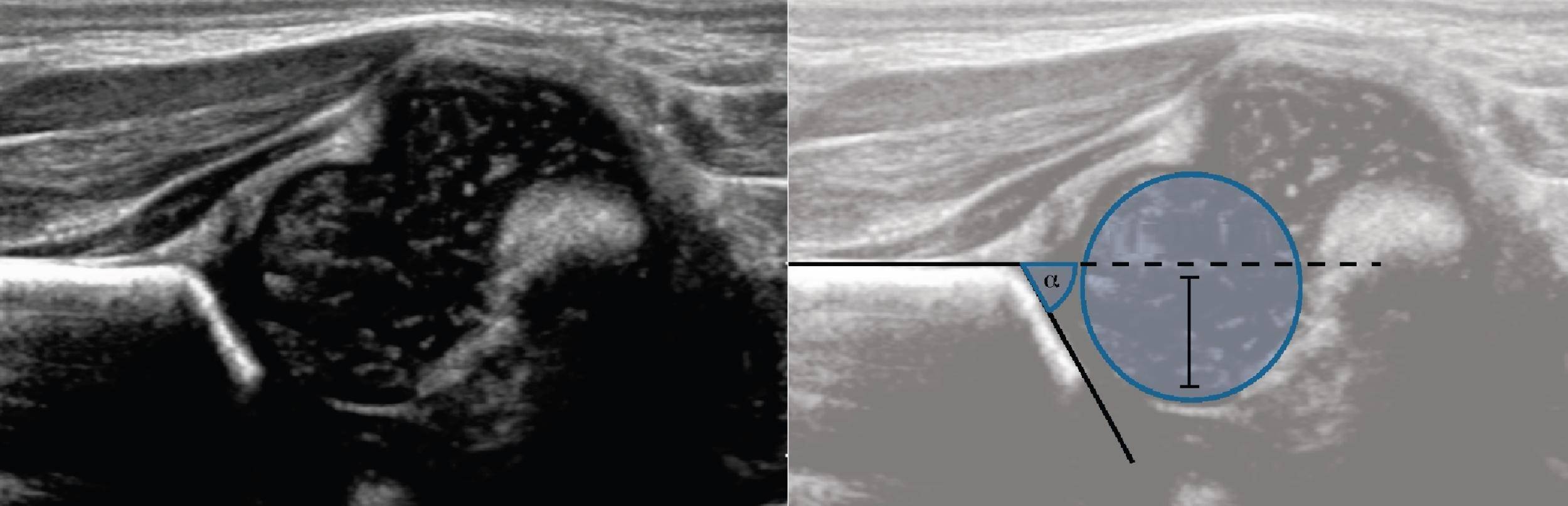
objective. In ultrasound, the lines are ∠α=65° (1) and ∠β=60° (2). The other lines aren't drawn correctly, so the angles aren't correct. Conclusions: Transitional structure (type 1b) of tuberose.
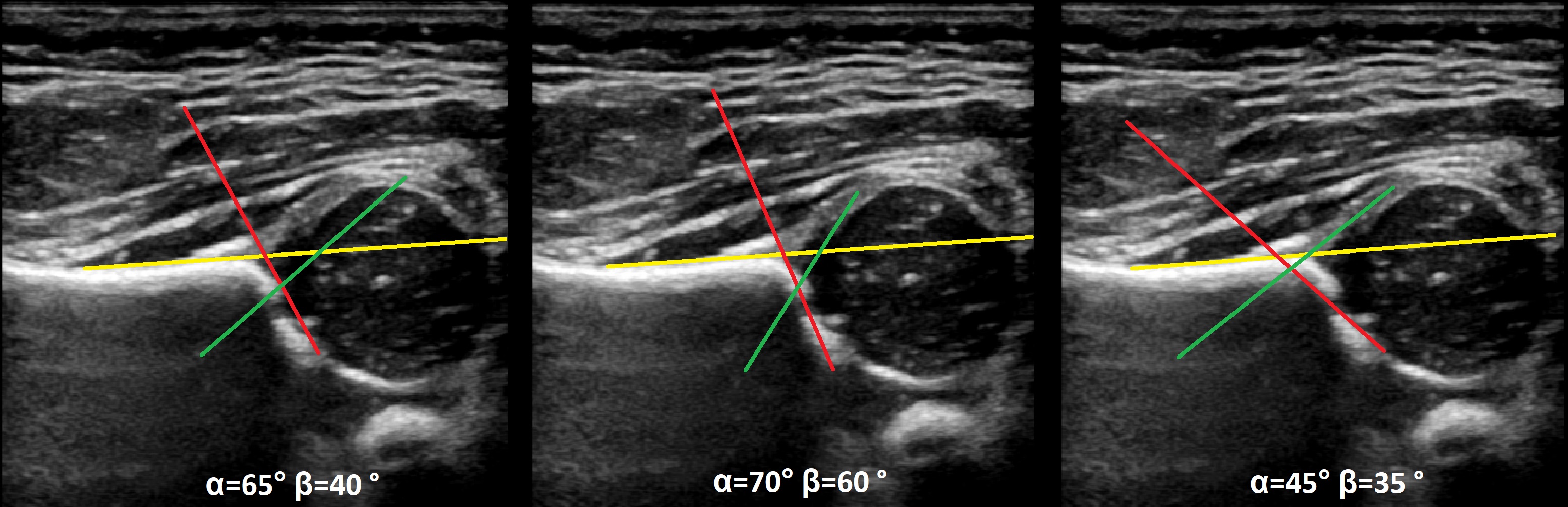
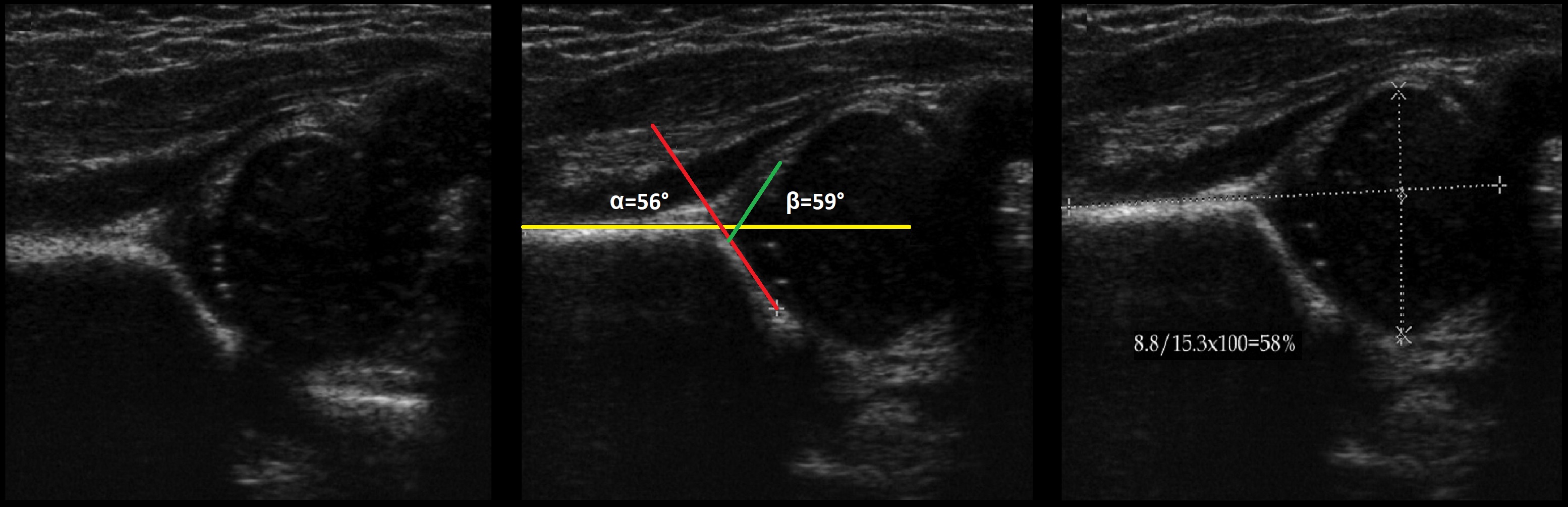
objective. On ultrasound examination of the hip joint: ∠α=56°, ∠β=59°; Bone Covering of the Head 58%. Conclusions: A child under 3 months has a physiological developmental delay (type 2a) and a child over 3 months has hip dysplasia (type 2b).
Task. On ultrasound examination of the hip joint: ∠α=68°, ∠β=62°; bony covering of the head Conclusion: Mature (type 1b) unstable T/B joint.
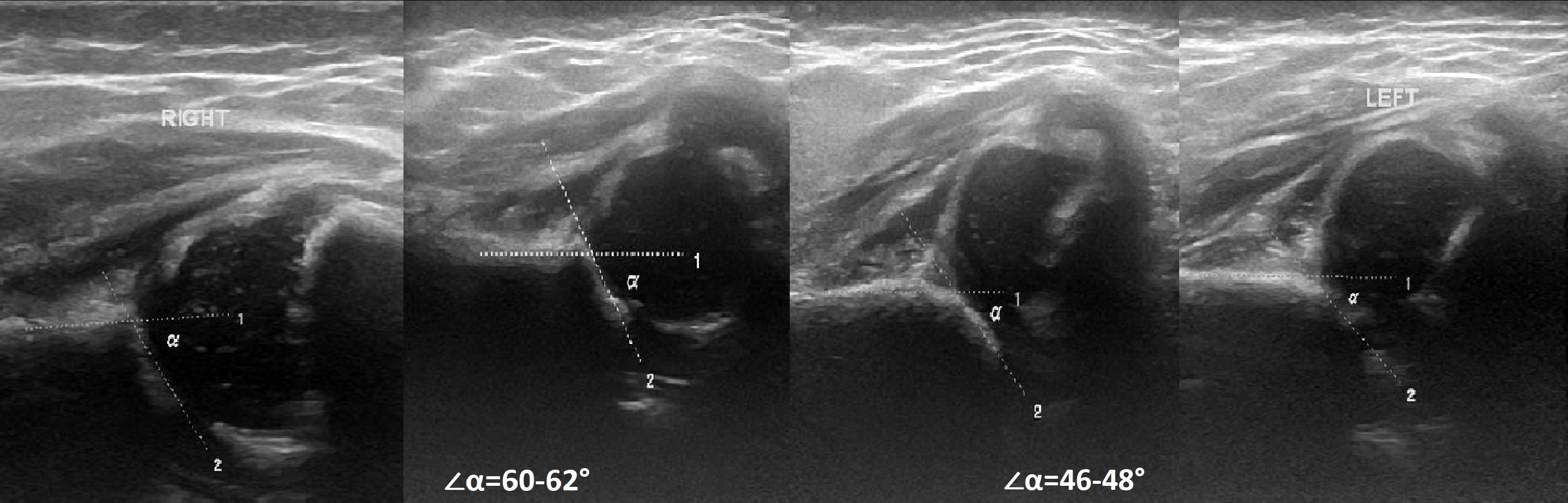
Object. On ultrasound examination, hip joint: right ∠α=60-62°, ∠β=66-70°; left ∠α=46-48°, ∠β=90-93°. conclusionTransition (type 1b) of the right hip joint. Severe dysplasia (type 2d) of the hip joint, premature dislocation on the left side.
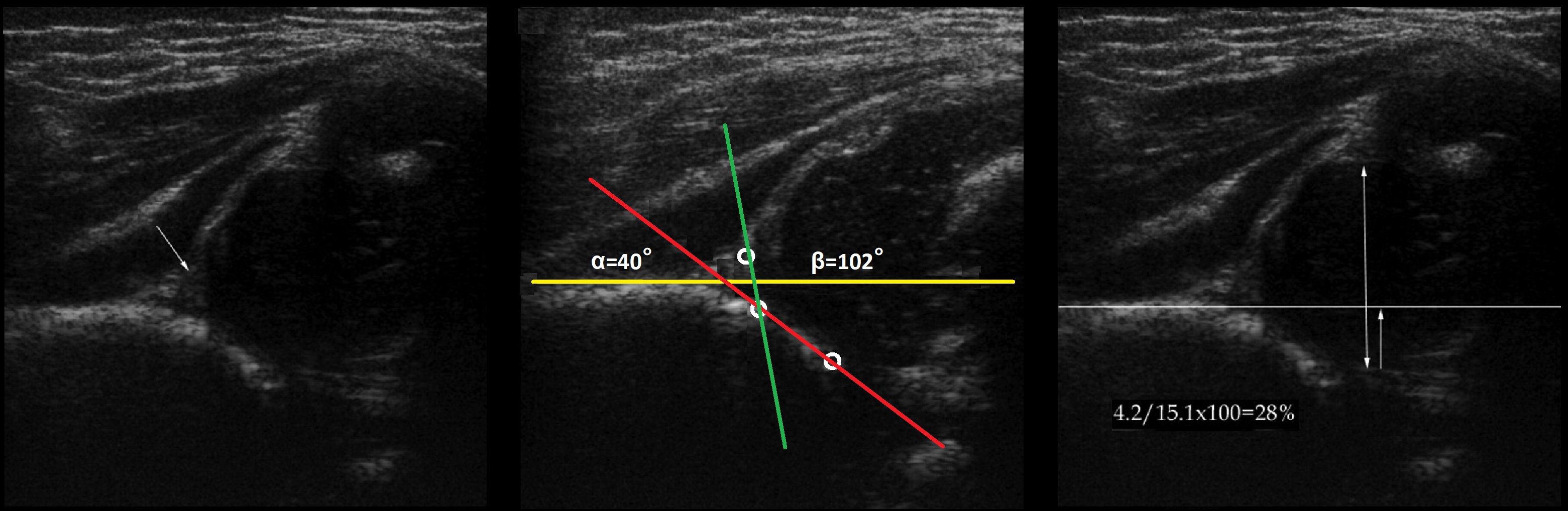
objective. In the ultrasound of the hip joint: ∠α=40°, ∠β=102°; bony covering of the head Conclusion: Severe dysplasia (type 3a) of the hip joint, subluxation.
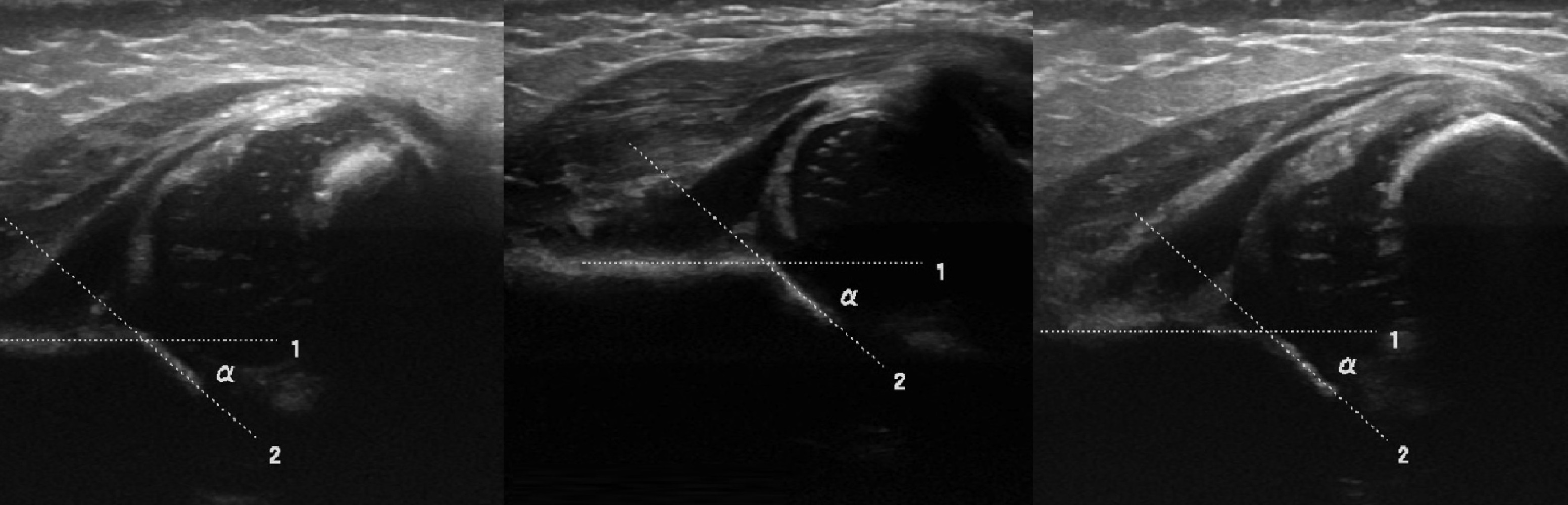
objective. In the ultrasound examination of the hip joint with ∠α conclusion: severe dysplasia (type 3a) of the hip, subluxation.
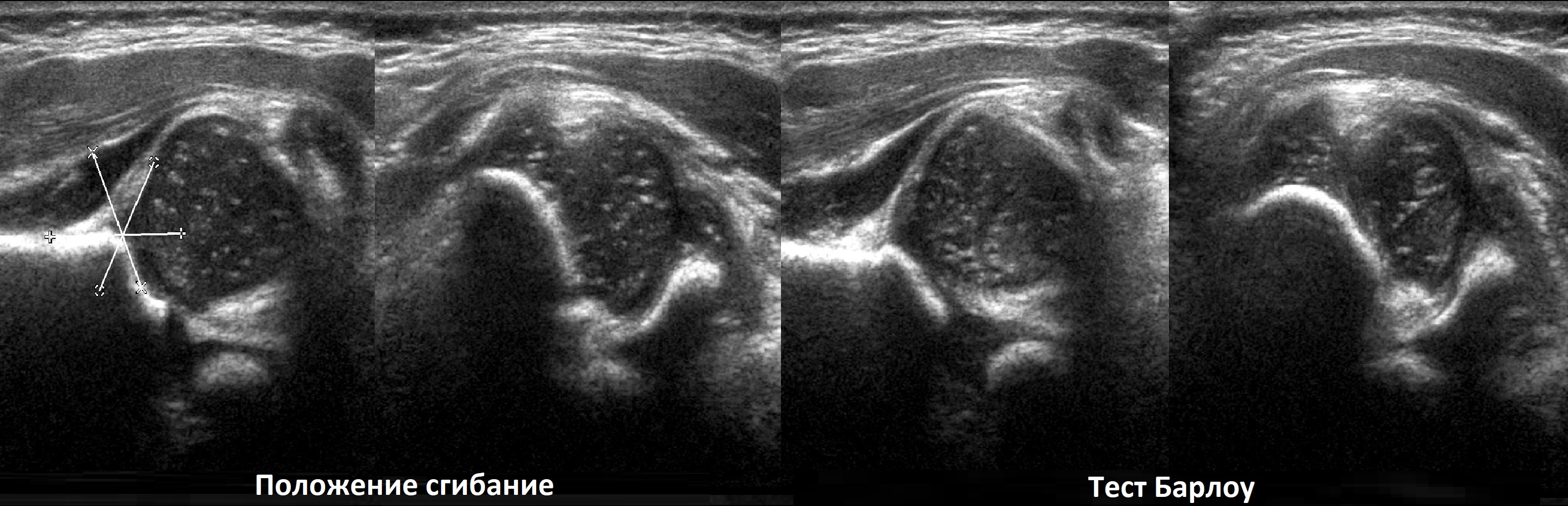
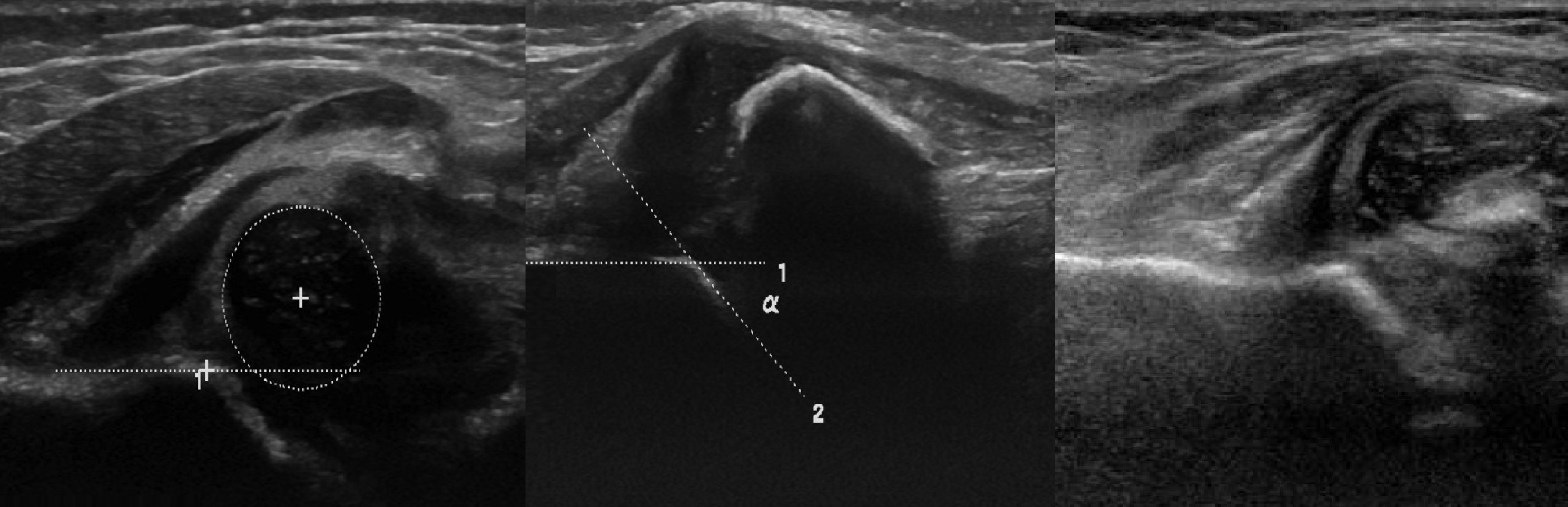
objective. Concomitant type 4 hip dysplasia: the head is laterally and superiorly displaced, the bony roof covering is minimal (1); Barlow's test revealed an empty acetabulum (2), the cartilaginous roof is wrapped in the acetabulum preventing repositioning of the acetabulum (3).
CLINICAL PICTURE OF CORRUGATOR SYNDROME
local symptoms
- nagging, drawing, rubbing pains in buttocks, sacroiliac and hip joints, aggravated by walking, standing, adducting, and squatting
- the pain subsides slightly when lying down or sitting with your legs apart
- when the gluteus maximus muscle is well relaxed, a dense and painful area can be felt under the muscle (Bonnet-Bobrownikov sign)
- when palpating the tip of the sternocleidomastoid muscle, pain is detected on the back surface of the leg (Wilenkin's sign)
- Painful tip of the ischial bone: The probing finger hits it and slides intensively from the ischial tuberosity upwards medially.
- Often there is tonic tension of the sternocleidis muscle in combination with this condition of other pelvic floor muscles – coccygeus, internal obturator muscle, levator recti, etc. This is called pelvic floor syndrome; Symptoms of vascular and sciatic nerve compression in the popliteal region.
- Pain when compressing the sciatic nerve is dull and cerebral with a pronounced vegetative coloring (shivering, burning, stiffness).
- The pain radiates to the whole leg or mainly to the area of innervation of the shin and ankle nerves.
- It can be triggered by heat, weather changes or stressful situations.
- The Achilles reflex and superficial sensitivity may be impaired.
- The fibers that make up the tibial nerve are predominantly affected.
Some manual tests are helpful in diagnosing wrinkled muscle syndrome:
- Pain when palpating the upper part of the internal trochanter (the insertion point of the sternocleidomastoid muscle)
- Pain on palpation of the lower sacroiliac joint – projection of the pectoral insertion point
- Pain reproduction during passive hip flexion with simultaneous inward rotation (Bonnet-Bobrovnikoff sign)
- Sacroiliac band test that allows simultaneous diagnosis of the sacroiliac and hip ligaments.
- Tapping on the buttocks (on the painful side) - this causes pain that spreads to the back of the thigh.
- Grossman syndrome - tapping on the lower lumbar or upper sacral process with a mallet or folded fingers causes the gluteus muscles to contract
TECHNIQUES FOR DIAGNOSIS OF PIRIFORMIS SYNDROME
Transrectal palpation of the sternum, characterized by a hard, extremely painful sting, is considered the most reliable method of diagnosing coronary syndrome. The sternum can also be palpated through the gluteus medius in the supine position.
Infiltration of the sternum with novocaine is an important diagnostic test, and the resulting positive changes can be evaluated. A definitive diagnosis can be made when clinical signs improve after isometric relaxation of the sternum.
Causes of hip subluxation
In early infancy, hip dysplasia most commonly causes femoral head subluxation. However, do not think that in adulthood you will be safe from such an injury if it does not occur in childhood. Not at all. With congenital or acquired dysplasia of the cartilage tissue of the hip joint in infancy, there is a risk of various pathological changes in this bone joint.
First of all, it is important to understand that dysplasia does not go away. The thinning of the cartilage layer in the affected areas persists for life. The alignment of the feet is abnormal, the femoral heads are not physiologically aligned in the acetabulum, and compensatory torsion and rotation of the pelvis often occurs.
None of these anomalies are noticeable because they are not visible from the outside. Therefore, doctors do not pay attention to the existing risk factors during medical examinations.
Coxarthrosis hip subluxation often occurs in old age, since not only the articular cartilage but also the bone tissue is destroyed. The fixation decreases and the ligaments and tendons are deformed.
Other possible causes of hip subluxation include:
- Excessive body weight, which puts increased pressure on the articular surfaces and provokes a displacement of the articular surfaces towards each other;
- foot deformities in the form of flat feet and club feet;
- A valgus or varus curvature of the tibia or thigh;
- Deformations of the femoral neck;
- heavy physical work with constant strain on the muscles of the back and lower limbs;
- deforming arthrosis of the knee joint;
- spinal curvature and poor posture;
- Osteochondrosis of the lumbosacral spine, in which the patient is forced to spend a long time in an unnatural forced posture;
- dystrophy or atrophy of muscle fibers;
- Scarring of ligament and tendon fibers after sprains and tears;
- hip arthroplasty;
- stretching of the joint capsule;
- Fractures and breaks of the femoral head, femoral neck or acetabulum.
How to recognize a hip subluxation (signs and symptoms)?
The first signs of a hip subluxation are stiffness, limitation of movement, and pain when performing certain movements. For example, a hallmark symptom of a hip subluxation may be the inability to sit up straight without support from other objects. The person is unable to pull the leg back relative to the trunk. Or it is impossible to move the leg to the side. Any restriction in mobility is a symptom of hip subluxation.
The clinical signs of hip subluxation due to trauma tend to be false. The characteristic symptoms of a sprain or tear of ligament and tendon fibers, fracture of a bone, etc. come to the fore. However, it is worth remembering that any injury can adversely affect the joint capsule. Characteristically, with traumatic etiology, the subluxation is almost always not fixed. It is an unstable condition that is very difficult to diagnose. However, an unstable position of the femoral head is a very dangerous condition.
How to diagnose hip subluxation at home:
- Sit in a chair with your knees apart; if you feel something is bothering you, see your doctor;
- Squat down, if this is not possible, you need help;
- Lie on your back and bring your bent knees to your chest; if you can do this, there is no subluxation in that plane.
This is only part of the diagnostic functional tests. You can do the others together with your orthopedist in our chiropractic clinic during your first free visit.
We strongly encourage you to see an orthopedist if you experience recurrent pops in the hip joint, tightness in the surrounding muscles, legs that tire easily, inability to perform certain movements, stiffness and mobility that causes pain.
symptoms

The symptoms of a pelvic tilt can be mild or severe and can seriously affect the body's ability to function. If the deformity is moderate, the affected person may feel unsteady when walking or fall frequently.
The most common symptoms are pain:
When the pelvis is misaligned for a long period of time, the body corrects and compensates for the disturbed biomechanics and asymmetry, and the muscles, tendons and ligaments adapt accordingly. Therefore, it may take time to heal. In addition, abnormal pelvic position can be difficult to correct as the pathological movement pattern develops over time. The longer the pelvic tilt persists, the longer it takes for normal muscle balance to be restored.
diagnosis and treatment
pelvic tiltA physical examination of the patient can usually provide a good diagnosis. Imaging procedures such as X-rays or magnetic resonance imaging (CT) are indicated if changes in the spine or hip joints have to be diagnosed.
There are different possibilities Treatment options for pelvic valgus The possibilities depend on the cause of the pelvic tilt. For example, when treating pelvic torsion, it is necessary to reduce muscle damage. This can be achieved through various physiotherapeutic techniques and the administration of NSAIDs. If the pelvic torsion is caused by different limb lengths, individual orthotics or surgical treatment are required.
In any case, the treatment of pelvic valgus is effective only in combination with the treatment of the pathogenetic factors that lead to a change in the position of the pelvis and a violation of biomechanics (physiotherapy, massage, chiropractic, physical therapy). LFC is the leading treatment for pelvic tilt, especially when the cause of the pelvic tilt is a muscular problem.
Use of the material is permitted with an active hyperlink to the permanent article page.
Read more:- external rotation of the hip.
- Inward subluxation of the foot.
- shortening of the hip.
- What is joint rotation?.
- The parts of the human leg are named.
- Photo of the right leg.
- Legs of different lengths in a child.
- Which doctor treats the hip joints.
