The time it takes for tissue to heal depends on the severity of the sprain. For example, if you sprained your ankle, you can walk again in 1-2 weeks, complete healing takes 6-8 weeks, and you can return to exercise in 8-12 weeks. For muscle sprains, the recovery time varies greatly. Sometimes it only takes a few weeks, sometimes it takes a few months.
- Torn tendon
- Clinical signs of tendon rupture
- degrees of severity
- How we treat sprains
- What to do after a sprain: First aid.
- Treatment of sprains by a doctor
- types of pathology
- symptoms
- SURGICAL TREATMENT
- Standard treatment includes:
- Dorsiflexion of the foot
- Muscle tissue of the sole of the foot
- Specificity of massage
- Varus deformity of the lower limbs
- This is how tendon injuries to the toes and feet are diagnosed
- Treatment
Torn tendon
A tendon is a connective tissue formation that is part of the structure of the striated muscle and ensures its attachment to the bone. A tendon tear occurs in the area where the muscle joins or attaches to the bone. In the latter case, a tear occurs in the adjacent bone or muscle.
The tear of the Achilles tendon or other tendons is the result of contraction and overstretching of the muscle. But there are also cases in which direct trauma is the decisive factor.
A torn tendon in your leg or hand can be treated at CELT's multidisciplinary clinic. Our specialists will work to ensure that you recover as quickly as possible and return to a normal life.
Clinical signs of tendon rupture
One of the most common injuries is a rupture of the Achilles tendon in the heel. In other cases, a tear of the shoulder tendon, a tear of the quadriceps femoris tendon at the kneecap, or the triceps brachii tendon at the elbow are common. Injuries such as extensor tendon tears are not uncommon in our clinic.

The symptoms of the injury depend on the injured tendon and the extent of the damage. Symptoms of an Achilles tendon rupture can include mild pain and swelling of the ankle in Grade 1 or severe pain and swelling of the joint.
In general, the symptoms of a torn Achilles tendon are as follows:
degrees of severity
There are three degrees of severity of ligament strain:
- Grade I – mild pain due to rupture of a few fibers of the ligament.
- Grade II – moderate pain, swelling and disability.
- Grade III – severe pain due to rupture of the ligament and subsequent instability of the joint.
A muscle strain is a traumatic injury to the muscle fibers themselves or the muscle-tendon junction and is divided into three levels of severity:
- I – moderately difficult.
- II – moderate, with weakness and painful contraction of the injured muscle.
- III – complete rupture of the muscle-tendon junction, which is characterized by severe pain and the inability to contract the affected muscle.
How we treat sprains
Treatment of total and partial ligament injuries is aimed at restoring the integrity and mechanical strength of the ligament.
In some cases, a tight bandage is required to immobilize the joint.
The cornerstone of treatment is early pain relief and anti-inflammatory therapy of soft tissue injuries, particularly in the setting of co-existing myositis. For this purpose, hirudotherapy, foot reflexology and apitherapy are used.
Leech treatments are great for reducing swelling and inflammation.
Special massages help restore mobility to damaged muscles.
In some cases, physical therapy and dry heat are required.
Kinesiotherapy is essential if the spine is severely overloaded.
Patients with acute injuries (dislocations, fractures) are admitted at least 3 weeks (21 days) after the injury.
What to do after a sprain: First aid.
As soon as possible after the injury, the injured body part should be left alone. In mild cases, it is enough to stop physical activity and sit or lie down with the injured limb in an elevated position. For example, you can place a pillow or rolled blanket under the sprained leg, hang the arm on a support, etc.
If there is severe pain or joint destruction, greater immobilization is required. In such cases, a splint made of improvised materials (cardboard, cardboard) is applied or the injured limb is tied to the body in a position that is as painless as possible.
After or at the same time as immobilization, it is advisable to cool the injured area. Ice, a bag of cold water and finally a wet towel should be used. You can buy a cold spray at the pharmacy. It is often used in first aid kits at sporting events. The cold stops internal bleeding more quickly, narrows the vessels, delays the development of inflammation and slows down swelling. In addition, cooling reduces pain. If the pain is severe, non-steroidal anti-inflammatory drugs in tablet or injection form as well as paracetamol can be used.
- Warming and rubbing the injured area. Heat and massage are indicated only on the 3rd and 4th days after the sprain to improve blood circulation and accelerate the resolution of the hematoma and swelling and the healing process. Immediately after the injury, these treatments have the opposite effect.
- Alcohol consumption. Increases bleeding and swelling and slows tissue regeneration. Alcohol is only acceptable when medical attention is difficult to obtain and there is nothing to relieve the severe pain.
- Continue working or exercising despite the pain. Stretched ligaments or muscles need rest to recover as quickly as possible. Only after a certain period of time can special exercises be carried out so that you can return to life as quickly as possible.
Mild sprains disappear without special treatment. If the injury only causes a little pain or swelling and you can move independently without major restrictions, you can avoid seeing a doctor. To speed up your recovery, you should rest the injured body part. The pain in the first few days also contributes to this, reminding you to protect the joint or the strained muscles. Avoid physical labor or lifting weights. For leg sprains, it is advisable to use a cane or crutches while walking until the pain subsides significantly.
Treatment of sprains by a doctor
If a fracture is suspected, if there is severe pain and swelling or a large hematoma under the skin and in the elderly, it is advisable to see a doctor within the first few hours after the injury. The sooner the better.
In severe sprains with torn ligaments, conservative treatment is ineffective and surgery is necessary. If a fracture has occurred in addition to the dislocation, the gradually increasing swelling prevents the surgeon from restoring the normal alignment of the bones and immobilizing the limb well. Time is against us here, which makes treatment more difficult.
If you have a sprain, you can see a surgeon at a primary care office or go to a trauma center. In both centers you can be treated without an appointment: the emergency room usually treats emergencies, but if you go to the health center you must tell the receptionist that you are dealing with 'acute pain'. An x-ray of the injured area can be taken immediately in the emergency room. X-ray machines are not always available in the health center. If your condition does not allow you to seek medical attention yourself, call an ambulance.
The doctor will help you relieve pain and prescribe medication that you can take yourself. As a rule, it is recommended to take paracetamol if the pain is severe. If this doesn't help, you may need a prescription pain reliever. Your doctor may also prescribe a nonsteroidal anti-inflammatory drug (NSAID) in cream or gel form, such as: B. ketoprofen. This should be applied to the area of the sprain and then washed off immediately.
Ketoprofen increases the skin's sensitivity to light. Direct sunlight or artificial light (e.g. solarium) should be avoided during treatment and for two weeks afterwards. Oral NSAIDs (e.g. ibuprofen tablets) also help reduce swelling and inflammation.
In some cases, a cast or bandage is applied to a dislocation, as is the case with fractures. Physiotherapy is usually recommended from the 2nd to 3rd day to speed up the healing process. The most common treatments are UHF, later ozokerite, compresses with medicinal substances, therapeutic massage, therapeutic exercises, electrophoresis with dissolving, anti-inflammatory and analgesic agents. If ligaments or muscles are torn and conservative treatment is ineffective, the doctor may recommend surgical treatment. During a surgical procedure, the injured tissue is sutured and then a plaster cast is applied until the suture is completely attached.
types of pathology
Tendonitis can affect tendons of any size - the inflammation occurs in the tissues of the fingers, hand, foot, elbow or knee. The classification of pathology used by orthopedists takes into account the location of the focus of the disease. Doctors distinguish the following forms of the disease:
The lateral form of the pathology develops in the tendons adjacent to the wrist muscles (short and long extensor muscles, brachioradialis, etc.). The patient feels pain spreading along the outer surface of the elbow joint. Over time, professional and amateur athletes develop a weakness in their hand. Sufferers have difficulty performing basic tasks such as wringing laundry, lifting a cup, or shaking hands.

In the medial form, the tendons that attach to the flexor muscles of the forearm, elbow and hand are affected. It is diagnosed 7-10 times less often than lateral tendinitis and develops in people who regularly make rotational movements of the hand. The risk groups include golfers, seamstresses, professional logisticians, gymnasts, tennis and baseball players. The main symptom is a stabbing pain on the inside of the elbow joint.
Patellar ligament tendonitis is diagnosed in people who frequently perform jumps. The microinjury is caused by brief, intense strain on the quadriceps muscle. At the initial stage of pathology, pain syndrome occurs after the patient stops physical activity. Later, the pain occurs during physical exertion or when the patient is at rest.
Shoulder tendonitis affects the tissue adjacent to the rotator cuff muscles. The pain occurs with any activity that requires shoulder mobility. Acute attacks can occur at night. The increase in inflammation leads to severe swelling.
symptoms
The symptoms of the disease appear gradually. In the initial stages, the patient feels pain during maximum physical exertion. At other times, the damaged tendon does not cause any discomfort in a child or adult. Over time, the pain syndrome becomes more intense and the slightest movement causes discomfort. If left untreated, it can result in the patient being unable to perform everyday activities such as washing dishes, getting dressed, fastening buttons, and tying shoelaces.
The skin near the inflammation becomes red and swollen. There may be a local increase in temperature. Palpating the tendon increases sensation. Sudden movements of the injured limb may cause a cracking or popping sound.
SURGICAL TREATMENT
There are two different surgical techniques for treating Achilles tendon disease: open and endoscopic.
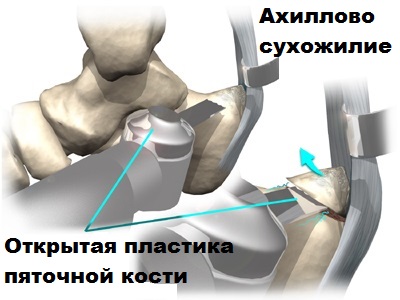
Open operations are becoming increasingly rare in this area and are often complicated, so we will not go into detail here.
Endoscopic surgery is preferred because of less pain, short recovery time after surgery, good cosmetic results and the possibility of a quick return to sports.

The operation is performed under the guidance of an arthroscope through several punctures in the skin in the Achilles area. The image from the arthroscope is transmitted via a video camera to a monitor on which the surgeon can see the inflamed capsule and the bony hypertrophy (osteophytes) of the heel bone. Osteophytes and inflamed tissue in the tendon area are removed using a special shaver device.

Cold plasma can also be used to more gently isolate and remove abnormal tissue in the Achilles tendon area. After the operation, the patient can immediately walk with almost full weight. After a few days, the patient begins training to restore mobility to the foot. The stitches are removed after two weeks.

Physiotherapeutic treatment accelerates rehabilitation.
In our opinion, arthroscopic surgery is a reasonable, minimally invasive alternative to open surgery. The extremely small skin incisions made during arthroscopy compared to open surgery prevent wound healing problems, unsightly scarring and nerve damage.
Standard treatment includes:
- Non-steroidal anti-inflammatory drugs to relieve swelling and pain;
- Short-term corticosteroids;
- cold compresses to relieve pain and swelling;
- rest to reduce stress on the joint;
- Antibiotic therapy if a bacterial infection is present.
If the joint is severely damaged, synovitis can sometimes only be treated with surgery.
Should fluid be sucked out of the knee joint? Opinion of a practicing orthopedist and traumatologist:
Synovitis is often diagnosed in people with osteoarthritis. The damaged cartilage surfaces become inflamed and fluid accumulates in the joint. Osteoarthritis treatment should not be started under these conditions. The inflammation should be treated and only then should intra-articular synovial fluid injections or other less effective therapies be administered.
Dorsiflexion of the foot
The muscle fibers of the hindfoot are located beneath the connective tissue and extensor tendons.
| Designation | Position | function |
| Short tendon | It begins at the anterolateral edge of the calcaneus, runs along the dorsum of the foot and ends at phalanges 2 and 5. | Extends the 2nd and 5th toes |
| Extensor shortus The short tendon of the big toe | Runs from the heel bone to the tendon of the big toe | Extends the big toe |
Muscle tissue of the sole of the foot

The fibers located in the sole of the foot form three muscle groups:
- Medial. They are responsible for the movement of the big toe.
- Laterally. Responsible for the motor activity of the little toe.
- Medial. They control the flexion of all toes.
The muscles of the plantar surface of the foot belong to each of these muscles, which have specific functions.
They are found in the deep fibers in the spaces between the metatarsals, the ligaments and the feet.
Specificity of massage

The massage should be performed with one hand. 2.
2. One hand should bend the knee and hold the shin. 3.
3. The palm of the other hand should press on the child's foot, causing dorsiflexion of the foot. This stretches the heel tendon and eliminates sole flexion.
5 Press your lower leg against the table with your palm and secure it around the ankle. With the other hand, grasp the foot so that the palm rests on the sole of the foot and perform slight passive dorsiflexion of the foot. At the same time, apply pressure to the side edge of the foot. 6.
At the same time, perform a pressure point massage in the ankle area.
7. Next step: Fix the foot in the ankle joint with one hand and gently stretch the forefoot outwards with the other hand.
8. Turn your foot outwards.
Stroking, shaking and vibrating are helpful. This reduces muscle tension in the back and middle parts of the lower limbs. To strengthen the weakened front and side groups, use more vigorous massage techniques on the lower leg and foot. Rubbing, kneading and moderate tapping are carried out.
Varus deformity of the lower limbs
In childhood, a varus curvature of the leg can be treated conservatively. The position of the shinbone is normalized with orthopedic shoes and special exercises. Massages are used as an additional therapeutic measure.
If there is a lower leg curvature, the massage is carried out as follows:
3. Buttocks massage: circular or cross stroking, rubbing, kneading, percussion.
4. Thigh massage. Stroking, rubbing, kneading, stroking again.
5. continue to the knees. A variety of stroking movements are carried out. Then rubbing and pressing the lateral condyles. 6.
6. Gently massage the lower leg. Stroke, rub, knead, shake. Then massage the calf muscle area. Massage the side of the calf muscle more intensely. The Achilles tendon is bypassed.
This is how tendon injuries to the toes and feet are diagnosed
First, an orthopedic injury specialist will perform an orthopedic exam. Key elements include assessing joints connected by tendons, palpating tendons for pain or defects, assessing tendon flexibility, and checking foot strength. The doctor will also check the range of motion in the area of pain. Sometimes stiffness or weakness may be noticed in the joint area. The orthopedist uses tests to determine the extent of the damage, e.g. b.
- Arthrocentesis
- Magnetic resonance imaging of the foot
- Ultrasound examination of the foot
- X-rays of the foot and toes
- CT scan of the foot.
Treatment
Treatment varies depending on the patient's condition and includes
- Sprains: Rest, ice, compression and elevation followed by exercise provide relief. Sprains rarely require surgery.
- Torn tendon: Rest and anti-inflammatory medications will ease the discomfort while the torn tendon heals. If there is a tear, surgery may be required.
- Tendonitis: Tendonitis can improve with rest, ice or heat, anti-inflammatory medications, splints, and exercise. Sometimes surgery followed by physical therapy is necessary.
- Tendinosis: The doctor recommends rest, ice or heat, splinting, exercise and physical therapy
- Tenosynovitis: Rest, splinting, and anti-inflammatory medications relieve symptoms of tendonitis. However, some patients require surgery.
- ligaments and tendons of the foot.
- tendons of the foot.
- Shin extensor muscles (tibialis extensor muscles).
- tendons of the ankle.
- Heel bone tendon sac in Latin.
- soleus muscles of the foot.
- Lamb Muscle Soreness.
- How long it takes for the ligaments to heal.
