This approach gives good results even with severe arthrosis and is more effective in the postoperative period, since the treatment is based on manual work on the joint capsule, and the operation is an addition to it.
- Osteoarthritis of the big toe
- Joint-sparing surgery for minor trauma
- SYMPTOMS OF HALLUX LIMITUS / HALLUX RIGIDUS
- surgical treatment
- I PPS implant overview
- The topicality of the problem
- How is the lesion defined?
- diagnosis and treatment
- Rehabilitation after surgery
- Cost of Hallux Rigidus treatment
- Organ-sparing surgery
- Metatarsophalangeal Joint Arthrodesis
- Joints that need surgery most often:
- Methodology for limb assessment prior to arthrodesis.
- Causes of hallux rigidus
- What are the treatment options for hallux rigidus?
- Contraindications for partial replacement of the metatarsophalangeal joint
- Duration of treatment and rehabilitation after partial denture
Osteoarthritis of the big toe
Osteoarthritis of the metatarsophalangeal joint, or hallux rigidus, is defined by doctors as degeneration and destruction of the joint of the big toe. Hallux rigidus develops as a result of a long-term, progressive, deforming inflammation of the metatarsophalangeal joint.
The disease is manifested by severe stiffness, deformation of the big toe and pain when walking.
The precipitating factor for the development of arthritis can be trauma to the joint, constant stress on the joint, or a systemic disease. Sometimes the cause of osteoarthritis cannot be determined.
Hallux rigidus is characterized by restricted movement of the first toe due to arthritic changes. The normal amplitude of big toe dorsiflexion is about 50-60 degrees, while the hallux rigidus limits the range of motion to 5-15 degrees. These movements are accompanied by significant pain. The hallux rigidus leads to a complete immobilization of the thumb.
Hallux rigidus is the second most common disease of the big toe. First and foremost is the valgus deformity of the thumb, the hallux valgus. Statistically, one in forty-five people over the age of fifty suffers from hallux rigidus. Both feet are often affected at the same time, especially in rheumatoid arthritis and gout.
Researchers have identified several causes for the development of hallux rigidus. The first is inflammation and detachment of the articular cartilage of the big toe after trauma or as a result of a rheumatic disease. Hallux rigidus can occur as a complication after surgery to correct a valgus deformity of the first toe (hallux valgus).
The tarsometatarsal joint consists of the first metatarsal bone and the main phalanx of the thumb.
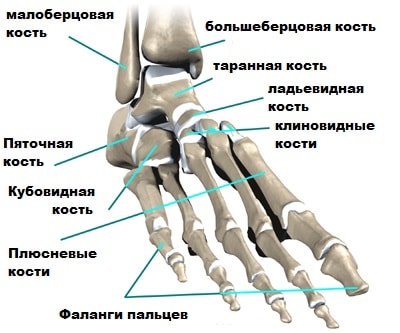
Like any other joint in the body, it is covered with articular cartilage.
The articular cartilage covers the ends of the bones and is very smooth, shiny, and whitish in color.
Joint-sparing surgery for minor trauma
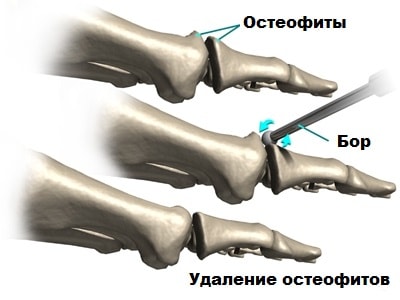
In some cases, exostoses, or growths around the joint, prevent the finger from flexing. These growths cause problems with walking and prevent the thumb from pushing off the ground normally when walking.
A healectomy is joint-preserving surgery that removes the bony outgrowths around the joint, particularly at the tip, which increases range of motion and reduces pain.
This surgery is also complemented by an osteotomy of the first metatarsal to decompress (relieve pressure) the articular surfaces relative to each other. The aim of the operation is to shorten the first metatarsal, thereby reducing the pressure of the metatarsal on the big toe and thus reducing the pain syndrome.
After shortening, the bone is fixed in its new position with intra-articular screws. Surgery is more commonly performed in younger patients when there is a chance to extend the life of the joint.

SYMPTOMS OF HALLUX LIMITUS / HALLUX RIGIDUS

Pains. In the early stages of the disease (Hallux limitus), the pain in the joint occurs only sporadically – with great exertion. The longer the problem is ignored, the more frequent and severe the symptoms become. The pain quickly becomes an inseparable companion when walking. In advanced stages, the pain persists even when the patient's legs are at rest. Limited mobility In the early stages of arthrosis (Hallux limitus), the mobility of the joint is minimal. With severe osteoarthritis (hallux rigidus), however, it becomes increasingly difficult to move the finger - especially to lift it. In the long term, osteoarthritis makes it almost impossible to move the finger. Claudium is inevitably painful. Patients with severe arthrosis of the metatarsophalangeal joint unconsciously put weight on the outer edge of the foot when walking. This in turn leads to the formation of painful blisters around the 4th and 5th metatarsals and under the phalanges of the first toe. deformation of the joint. The head of the first metatarsal thickens due to the presence of bony spikes (exostoses). The deformation becomes more and more pronounced over time. inflammation. When osteoarthritis worsens, swelling, redness of the skin and an increase in temperature around the joint are sometimes observed. It doesn't take long in the clinic to diagnose the disease. The podiatrist examines the foot and also takes X-rays of the forefoot in a straight and lateral projection. If arthrosis is present, the x-rays will show narrowing of the joint space and the presence of bone exostoses.
In order to slow down the progression of the disease and to make life easier for patients with osteoarthritis of the metatarsophalangeal joint, orthopaedists recommend wearing wide, comfortable shoes with stiff soles. In addition, custom-made orthopedic insoles and various types of silicone glide shoes should be used.
surgical treatment
The choice of treatment depends on the severity of the disease and is determined by the orthopedist.
In the early stages of osteoarthritis, joint-preserving operations are performed: cheilotomy (removal of osteochondral outgrowths) and decompression osteotomies of the first metatarsal and the proximal phalanx of the first toe (shortening of these bones). These operations eliminate the pain syndrome, preserve the joint surfaces and restore joint mobility. In the case of severe arthrosis (Hallux rigidus), saving the joint is unfortunately pointless. In recent years, the endoprosthesis has been used to treat hallux rigidus. Unfortunately, the results are not always satisfactory. The best treatment for advanced osteoarthritis so far is
I PPS implant overview
Seeburger design, first metatarsal head shell (1964)

Downey Proposal
Downey's articulated ball and socket
Implant (1965)

Swanson's design, single stem silicone semi-implant (1967)
Cutter's metatarsophalangeal prosthesis (1971)
Weil modification of the Swanson semi-implant (1977)
Koenig two-component total implant (1988)

The topicality of the problem
- The incidence of deforming osteoarthritis of the first metatarsophalangeal joint is not declining;
- Impairment of the normal function of the I. PPS leads to gait disturbances and impairment of the support function of the foot in general;
- High rate of unsatisfactory results with conventional treatment methods (resection arthroplasty, arthrodesis);
- patient dissatisfaction with the results of surgical treatment;
- Impairment of foot roll in PFS arthrodesis.
- Symptoms of inflammation of the skin or deep tissue of the foot at the time of the operation or in the past (suppurative arthritis, osteitis in the forefoot area).
- Trophic changes due to chronic vascular diseases (obliterating atherosclerosis, varicose veins of the lower extremities, lymphedema).
- Severe somatic diseases that are a contraindication to surgical intervention.
- Psychiatric Disorders.
- pregnant women.
How is the lesion defined?
The symptoms and treatment of deforming arthrosis of the metatarsophalangeal joints of the foot depend on the stage of development and localization of the clinical pathology. The progression of neurological damage is gradual. The initial stage is characterized by a steady thinning of the cartilage layer of the joint or joints and a lack of synovial fluid. With the clinical progression of the disease, clear signs of damage appear.

Before starting the foot treatment, the patient must be examined clinically and diagnostically. Disease stages with clear radiological classification and a number of symptomatic features:
| disease stage. | symptoms and signs | Radiological signs |
| stage 1 | Fatigue quickly after long periods of walking or running, feeling of heaviness in the legs and occasional grinding. The disease does not have an acute course | The interphalangeal joint shows a slight narrowing of the articular stroma and tufts of small villi. |
| grade 2 | The mobility of the joint is restricted; Swelling and redness of the soft tissues are visible | Beginning of joint laxity with bony hypertrophy. The joint space is significantly narrowed |
| grade 3 | Severe deformity of the foot, limping and persistent, acutely painful or rigid posture day and night | The joint head is loose, the joint space is barely visible, and there are numerous bony outgrowths (osteophytes). |
diagnosis and treatment
In the treatment of deforming arthrosis, the radiological findings and the diagnostic equipment are of particular importance. CT or MRI scans, ultrasound and biochemical tests provide a more meaningful picture.
It is important to make the correct diagnosis at the earliest possible stage of the pathology - this will greatly facilitate treatment.
Timely treatment can significantly slow down the inevitable degenerative destruction of the joints. Depending on the degree of pathology, therapeutic conditions are selected. Grade 1 is easier to treat.

At this stage of clinical development, the following measures are effective:
- administration of drugs in pharmacological combinations;
- treatment with physiotherapy;
- remedial gymnastics;
- spa treatment;
- folk medicine.
In the initial stages of the disease, the administration of painkillers and anti-inflammatory drugs is required. Such treatment is justified when there is an inflammatory reaction in the synovial membrane when fluid accumulates in the joint cavity.
In contrast, in stage I deforming arthritis of the feet, synovitis is almost absent. Treatment with folk remedies, therapeutic exercises and contact massage under constant medical supervision is enough.
The initial development of deforming arthritis of the feet takes years without progressing to a subsequent chronic inflammatory phase. However, treatment and monitoring is essential.
The disease is neglected when the next critical stage of aggravation - grade 2 deforming osteoarthritis - occurs, in which a fine line separates the ultimate destruction of joint composition (grade 3 deforming osteoarthritis).
At this stage, the acute pain occurs more and more frequently. The patient receives higher doses of painkillers in combination with nonsteroidal anti-inflammatory drugs.
Rehabilitation after surgery
For 14-20 days, the patient wears the postoperative VALGO shoe, specially developed in Italy for forefoot surgery.
On days 14-20, the patient is clothed. The postoperative bandage is removed.
As soon as the bandage is in place, the most important phase of treatment begins – rehabilitation. To this end:
- Physiotherapy and physical therapy are prescribed;
- Injections of plasma (PRP therapy) and prosthetic synovial fluid continue to facilitate sliding in the joint.
Such a health problem can be effectively countered by timely contacting the doctors of our clinic. We look forward to your visit and remind you that free remote consultation is possible for patients from other cities.
Cost of Hallux Rigidus treatment
The final price of the operation is determined during the consultation and depends on
- the severity of osteoarthritis and the extent of foot deformity;
- the extent of the surgery (whether 2, 3, etc. toes are involved) and so on.
- The operating surgeon
The operation of the metatarsophalangeal arthrosis of the first toe takes 15-20 minutes. You can walk immediately after the operation.
- Member of the Italian Medical Order
- Member of the Italian Society of Orthopedic Traumatology (SIOT)
- Member of ALOTO (Association of Orthopedic Traumatologists of Lazio)
- Member of the Society for Rehabilitation (SIMFER)
- Active member of the Foot Surgeons Association (SISPEC)
orthopedic surgeon. Surgical correction of foot deformities using the percutaneous PBS method. Ideologue and partner of the VALGO project.
Member of the Order of Italian Doctors. Full member of the Italian Society of Orthopedic Traumatology (SIOT). Member of ALOTO (Society of Orthopedic Traumatology of Lazio).
Surgical correction of foot deformities using the percutaneous PBS method. Complex treatment of patients with foot pathology.
Organ-sparing surgery
In some cases, exostoses, or growths around the joint, prevent the toe from flexing. These growths cause problems with walking and prevent the thumb from pushing off the ground normally when walking.
A healectomy is surgery to remove bone growths around the joint, particularly at the top of the joint, thereby increasing range of motion and reducing pain.
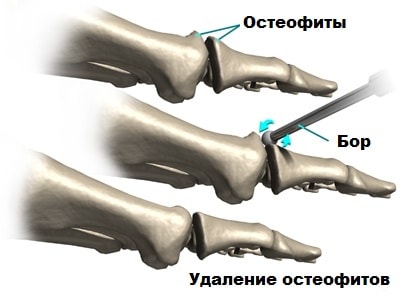
It is also performed in combination with a metatarsal osteotomy to relieve the joint surfaces (pressure relief). The goal is to shorten the first metatarsal, which reduces the pressure of the metatarsal on the big toe, which also reduces pain. After shortening the bone, it is fixed in its new position with intra-articular screws. This procedure is more commonly performed on younger patients when there is a chance to extend the life of the joint.

Metatarsophalangeal Joint Arthrodesis
Many surgeons prefer arthrodesis of the metatarsophalangeal bones, a procedure that significantly reduces pain. The aim of the operation is to fuse the metatarsophalangeal joints and the phalanx in a functionally favorable position.

During the operation, the articular surfaces are excised, fused in a functionally favorable position and secured with screws. After the operation, the thumb no longer moves. Postoperative pain is significantly reduced. Full bone fusion usually occurs within three months.

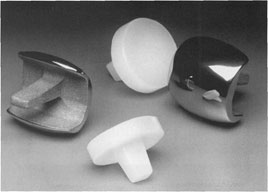
Endoprosthesis of the 1st metatarsophalangeal joint.
The method of choice for treating osteoarthritis of the first metatarsophalangeal joint is total joint replacement, similar to knee or hip joints. In this operation, the joint surfaces are removed and replaced with artificial joint surfaces, usually made of metal.
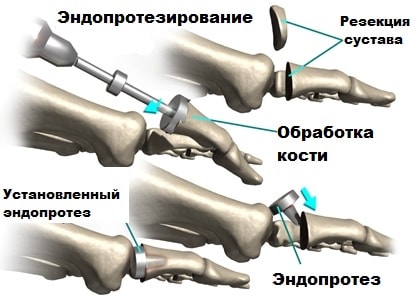
After this operation, not only is the pain reduced, but the mobility of the joint is retained. A disadvantage of this surgery is probably the short lifespan of the prosthesis. Over time, the prosthesis can become loose and affect mobility, which may require a second surgery. It is worth noting that according to a number of scientific studies, patients experience functional results after 1st limb arthroplasty.

Joints that need surgery most often:
The operation can be performed using various methods, the selection of which is planned individually.
The operation is not performed without anesthesia. General or spinal anesthesia can be used. The surgeon determines the most appropriate position for the damaged joint.
He then removes the altered cartilage tissue and moves the movable bone joint into the correct position.
With the help of a special assembly kit, the joints are fixed in such a way that further loosening can no longer be endured.
In surgical practice, it has been shown that women are more prone to deformities of the metatarsophalangeal joint of the big toe.
The average age of the operated patients is 64 years.
The minimum age is 45 years and the maximum age is 80 years.
Among the main reasons for performing arthrodesis of the metatarsophalangeal joint I include the presence of:
Methodology for limb assessment prior to arthrodesis.
X-rays of both lower limbs with feet are mandatory for all patients. A stress x-ray of the deformed feet and a lateral projection of the foot to be operated on are also required.
The operated patients are monitored by an orthopedist for a period of one year.
Known techniques for artificial joint immobilization are:
1. compressive intra-articular arthrodesis. In this case, the doctor removes the articular cartilage, the growth cartilage is not changed in any way.
3.mixed arthrodesis. Here the cartilage is removed. Grafts or special metal fixations are used for fixation.
4. compression arthrodesis. It can be open or closed. In this case, the joint surfaces are compressed.
With a professionally performed procedure, the patient can already walk in shoes on the second day without pressure on the forefoot. After 45 days, patients can safely wear normal shoes.
Causes of hallux rigidus
In many cases, the cause of hallux rigidus disease is unknown. Possible causes can be genetic factors, micro-injuries, incorrect or excessive strain on the foot.

© orthoped-kinik.co.uk
- Pain in the base of the big toe
- Stiffness of the big toe when walking, especially during rolling movements
- Swelling and redness of the metatarsophalangeal joint
- increase in cold weather
- Later complaints in the knee and hip joints due to incorrect loading.
What are the treatment options for hallux rigidus?

The endoprosthesis of the big toe metatarsophalangeal joint has proven itself very well in recent years, both in terms of function and durability. © orthopaed-kinik.com
Depending on the degree and stage of the disease, treatment begins with conservative measures such as stretching, anti-inflammatory drugs - including injections into the joint -, physical therapy and orthoses. Orthokinetic treatments are often helpful in the case of inflammatory irritation of the big toe.
In the surgical treatment, a distinction is made between joint-preserving interventions, such as the removal of bone deposits (cheilectomies) or changes in the joint structure, and conversion operations, such as resection arthroplasty according to Mark or arthrodesis (stiffening of the metatarsophalangeal joint of the big toe).
Arthrodesis of the metatarsophalangeal joint is still preferred in young, active patients because of the good long-term results.
Contraindications for partial replacement of the metatarsophalangeal joint
In advanced stages of Osteoarthritis of the metatarsophalangeal joint treatment with a partial hip replacement is unlikely. Abnormalities of the articular surface over the metatarsal bone are not an absolute contraindication, but may prompt the doctor to decide to treat the joint by immobilization (arthrodesis). Other foot injuries or valgus deformities cannot be corrected with the use of a metatarsal prosthesis. To correct these abnormalities, surgical correction of the conditions must first be made.
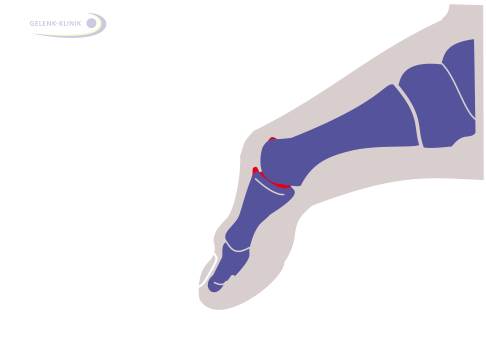 The metatarsophalangeal joint of the big toe is in an advanced stage of arthrosis and there are osteophytes in the joint cavity. © dr Thomas Schneider
The metatarsophalangeal joint of the big toe is in an advanced stage of arthrosis and there are osteophytes in the joint cavity. © dr Thomas Schneider 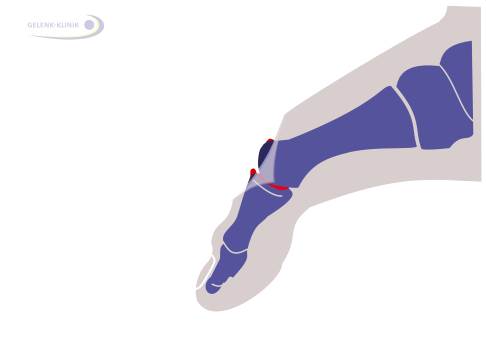 The doctor opens the joint with an incision. © dr Thomas Schneider
The doctor opens the joint with an incision. © dr Thomas Schneider
First, the orthopedist opens the joint with a 3 cm long incision on the back of the thumb. He then removes the osteophytes that have formed in the hallux rigidus. To see the joint space, the doctor stretches the joint slightly. Then he shortens the main joint of the thumb by a few millimeters.
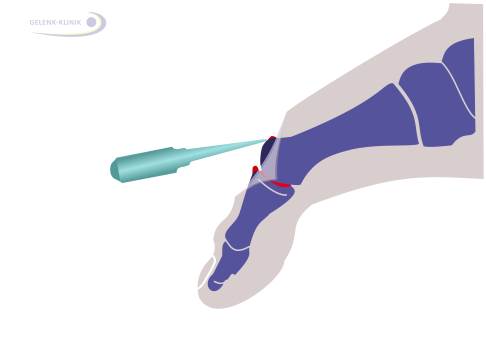 The surgeon removes the excess bone tissue. © dr Thomas Schneider. © dr Thomas Schneider
The surgeon removes the excess bone tissue. © dr Thomas Schneider. © dr Thomas Schneider 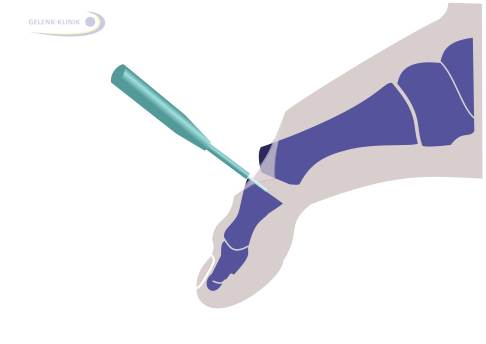 After removing the osteophytes, the surgeon eliminates the articular surface and cartilage defects. © dr Thomas Schneider
After removing the osteophytes, the surgeon eliminates the articular surface and cartilage defects. © dr Thomas Schneider
Duration of treatment and rehabilitation after partial denture
In the first few days after the hallux rigidus operation, the operated foot should be elevated and cooling compresses applied. The next day, the patient is advised to start light exercise. Taking anti-inflammatory drugs speeds up wound healing. Special orthopedic shoes with a firm sole should be worn for four weeks. Six weeks after the operation, the implant is permanently cemented into the bone.
The specialists in the joint clinic for the treatment of hallux rigidus are Dr. Thomas Schneider and Dr. Martin Rino. If you have any questions, the staff at the Joint Clinic in Germany will be happy to help and help you plan your trip.
Read more:- metatarsophalangeal joint.
- First metatarsophalangeal joint of the foot (metatarsophalangeal joint).
- Deflection of the first toe.
- Shapar joint.
- Stages of hallux valgus.
- chalgus valgus.
- The long section of the big toe.
- Arthrodesis of the subtalar joint.
