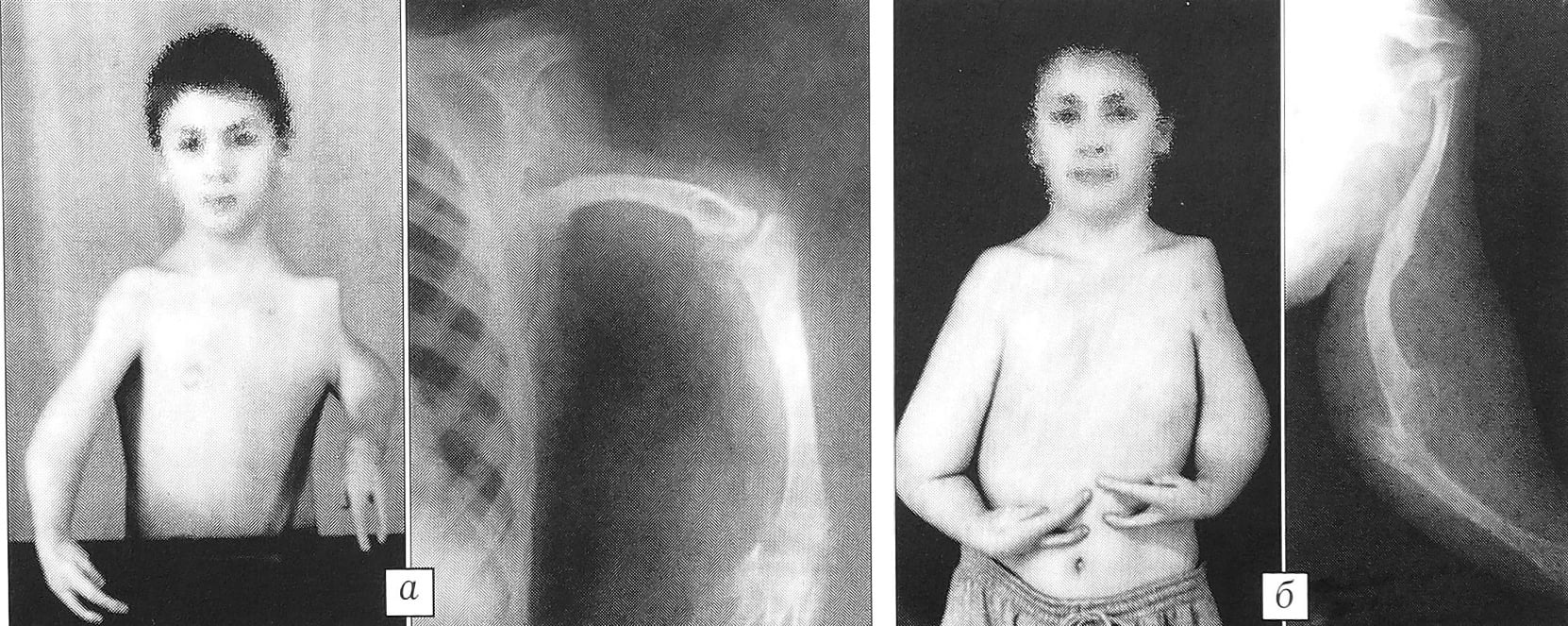
Figure 2: Appearance and radiographs of the 9-year-old patient FS with proximal congenital ectromelia of the left upper extremity. a - before surgery; b - 3 years after surgical repair of left humeral defect.
- Melanoma – a skin cancer (melanoma)
- Risk of occurrence
- Surgical treatment of proximal congenital ectromelia of the upper limbs in children
- keywords
- MATERIAL AND METHODS
- Longitudinal ectromelia of the tibia m/f.
- We had surgery at 4 months old (Turner) and then had a cast for 4 months. Our stories and those of children with aplasia, hypoplasia, other limb and spine anomalies. Stories of Children with Musculoskeletal Abnormalities Forum for parents of children with limb aplasia and hypoplasia
- Longitudinal ectromelia of the tibia m/rz.
- Surgical management of proximal forms of congenital upper limb ectromelia in children
- keywords
- MATERIAL AND METHODS
- Treatment
- Control of complications
- lifestyle
- Can there be complications?
- Causes of Spinal Extrusion
- Stages of development
- Rules of life
- prognosis and prevention
- Treatment of cartilage damage
- Stages of conservative treatment
- Stages of surgical treatment
- Movement
Melanoma – a skin cancer (melanoma)
This cancer is characterized by aggressive and rapid growth. If melanoma is not diagnosed early, it can lead to the formation of metastases and worsen the course of the disease. Recently, skin cancer of all stages is being detected in people all over the world. Statistics show an increase in the number of newly discovered melanomas.
The causes of skin cancer are not fully understood. Oncologists point out predisposing factors that trigger tumor growth. Melanoma is difficult to diagnose in its early stages due to the imprecise clinical picture of the disease. Therefore, there is a late need for medical care. A cancer diagnosis at an early stage increases the chances of a favorable treatment outcome.
Risk of occurrence
Predisposing factors play an important role in the development of skin cancer. Predisposing factors include:
- Prolonged exposure to the sun and frequent sunburns;
- Genetic predisposition. If skin cancer runs in the family, the risk of developing it in the next generation increases;
- fair skin with lots of birthmarks and freckles and red hair. This skin is characterized by a low melanin content in the cells;
- advanced age. It is believed that the risk of developing skin cancer increases with age. However, oncologists have noted that the incidence of this disease is increasing in younger age groups;
- Occupational hazard. Some jobs involve constant contact with carcinogenic substances. Long-term interactions of toxins with the skin increase the risk of developing cancer.
The presence of at least one of these risk factors requires regular visits to the doctor for preventive examinations.
Surgical treatment of proximal congenital ectromelia of the upper limbs in children
Three cases of proximal congenital ectromelia of the upper limbs (in two 4-year-old children and a 9-year-old) are presented. The symptom complex of this rare malformation is described, which includes defects in the long bones - shoulder and forearm - and radial aplasia of the hand. A comprehensive surgical treatment program for ectromelia has been proposed, which includes restoring shoulder length and creating a missing shoulder joint by microsurgical transplantation of a fragment of the outer edge of the scapula, eliminating the deformity of the forearm by centering the hand, restoring bilateral grasping function Polyclamping of one of the three-toed fingers or the transplantation of the foot to the position of the first ray of the hand includes. The treatment results of the three patients observed allow the developed program to be considered as an alternative to prosthetics.
keywords
Among the various forms of congenital malformations, the deformities are complex with a combination of the development of the upper limbs in children with the most underdeveloped hand and the long bones of the arm and forearm. Although they are referred to by the term dysmelia, they are not clearly defined in Russian literature. The names ectromelia, hemimelia and phocomelia have their own meaning, which does not facilitate the systematization of the pathology (1-7).
The most detailed classifications of these malformations are presented in foreign literature [8, 10]. Four main types are distinguished:
- distal forms of ectromelia, in which only the forearm and hand are affected;
- axial or proximal forms, in which the proximal parts of the limbs are affected;
- Phocomelia – with complete or almost complete absence of long bones;
- Amelia, characterized by the maximum severity of the defect, that is, aplasia of the upper limbs.
In addition, there are reports of the differentiation of ectromelia into longitudinal and transverse, which e.g. B. in the distal form of hypoplasia fits completely into the clinic of the radial and ulnar foot [7].
Most publications on the surgical treatment of patients with the pathology in question deal with surgical interventions for distal forms of ectromelia. For the proximal forms, either a categorical statement on the inadvisability of correcting the defect or a reconstruction with adaptation of the stump to a prosthesis is proposed [2, 6, 7].
MATERIAL AND METHODS
Patients with congenital upper limb malformations who have passed through the Microsurgery Department of GI NIDOI in recent years include. In the case of Turner syndrome, we were only able to identify three children in whom the deformity corresponded to the clinical picture of proximal ectromelia. The rarity of this malformation is confirmed by the literature, according to which its prevalence is 1.4 % (9). However, it should be noted that such patients are practically not referred to hospitals that mainly deal with surgical treatment.
Longitudinal ectromelia of the tibia m/f.
We had surgery at 4 months old (Turner) and then had a cast for 4 months. Our stories and those of children with aplasia, hypoplasia, other limb and spine anomalies. Stories of Children with Musculoskeletal Abnormalities Forum for parents of children with limb aplasia and hypoplasia

Forum for children with disabilities ' Forum for parents of children with limb aplasia and hypoplasia ' Stories of children with anomalies of the musculoskeletal system ' Longitudinal ectromelia of the tibia type m/beam
Longitudinal ectromelia of the tibia m/rz.
Total reports: 6
User Rating: 0
Greetings to all mothers and their little ones. I would like to join your friendly company!!!? My name is Irina, my son's diagnosis is the same as yours: m/radial longitudinal tibial ectromelia! We had surgery at 4 months old (Turner), then we wore a cast for 4 months! Now we are 1 year 8 months old, we have orthoses and 'nice shoes', we have a shortening of 4.5-5 cm. We cannot measure accurately because the knee cannot be straightened! Girls I really need your help and advice! I have read all the children's stories and almost all mothers write that their children were walking at 1.5 years old! My son can't even walk (let alone run) at 1.8 years old, this worries me a lot, I've already started to think that there's something wrong with my son ((((
We can't measure shortening accurately, not even in Turner, because his knee isn't fully straight and he walks with his knees bent! How is your child's gait and how is his knee? We were told the knee would need surgery later, but I was hoping for an extension and that was it. Thank you for being here.
Total message: 29
User Rating: 0
Forum registration date:
June 29, 2014.
Hello Irina, my name is Olga, we had the operation in January 2015, we still wear a cast, but I know some mothers who have children who actually walk in a machine, can you tell me what they say about it at Turner?
Total news: 29
User Rating: 0
Forum registration date:
June 29, 2014.
Irish, join us in contact, my website address:
Shmeleva (Dorozhkina) Olga Belgorod, I have friends Vika and Dasha, they will answer your questions, waiting, I also have classmates
Total news: 6
User Rating: 0
Total number of positions: 29
User Rating: 0
Forum registration date:
June 29, 2014.
Surgical management of proximal forms of congenital upper limb ectromelia in children
Three cases of proximal forms of congenital ectromelia of the upper limbs (in two 4-year-olds and a 9-year-old child) are presented. The syndrome of this rare malformation, which includes defects of the long bones - shoulder and forearm - and radial aplasia of the hand, is described. A comprehensive surgical treatment program for ectromelia is proposed, which includes restoring shoulder length and creating a missing shoulder joint by microsurgical transplantation of a fragment of the outer edge of the scapula, eliminating the deformity of the forearm by centering the hand, restoring bilateral grasping function Polycephalus of one of the three-toed fingers or the transplantation of the foot to the site of the first ray of the hand includes. The treatment results of the three patients observed allow the developed program to be considered as an alternative to prosthetics.
keywords
Among the various forms of congenital malformations, the deformities are complex with a combination of the development of the upper limbs in children with the most underdeveloped hand and the long bones of the arm and forearm. Although they are referred to by the term dysmelia, they are not clearly defined in Russian literature. The names ectromelia, hemimelia and phocomelia have their own meaning, which does not facilitate the systematization of the pathology (1-7).
The most detailed classifications of these malformations are presented in foreign literature [8, 10]. Four main types are distinguished:
- distal forms of ectromelia, in which only the forearm and hand are affected;
- axial or proximal forms, in which the proximal parts of the limbs are affected;
- Phocomelia – with complete or almost complete absence of long bones;
- Amelia, characterized by the maximum severity of the defect, that is, aplasia of the upper limbs.
In addition, there are reports of the differentiation of ectromelia into longitudinal and transverse, which e.g. B. in the distal form of hypoplasia fits completely into the clinic of the radial and ulnar foot [7].
Most publications on the surgical treatment of patients with the pathology in question deal with surgical interventions for distal forms of ectromelia. For the proximal forms, either a categorical statement on the inadvisability of correcting the defect or a reconstruction with adaptation of the stump to a prosthesis is proposed [2, 6, 7].
MATERIAL AND METHODS
Patients with congenital upper limb malformations who have passed through the Microsurgery Department of GI NIDOI in recent years include. In the case of Turner syndrome, we were only able to identify three children in whom the deformity corresponded to the clinical picture of proximal ectromelia. The rarity of this malformation is confirmed by the literature, according to which its prevalence is 1.4 % (9). However, it should be noted that such patients rarely come to hospitals that mainly deal with surgical treatment.
Treatment
Typically, an extra trabecula in the left ventricle does not require treatment, but if pain or discomfort occurs, treatment is necessary.
The following measures are used to support the affected person:
- A vitamin complex is prescribed, which the patient takes in the form of injections, capsules or tablets for a period of 1-3 months. This allows the heart to work normally again and the patient feels better.
- Magnesium and potassium supplements are prescribed. They have a positive effect on the functioning of blood vessels and the heart. It is not advisable to take these medications without a doctor's recommendation, especially in children. An incorrectly calculated dose can negatively affect the patient's mood and condition.
- The drugs are prescribed to stimulate metabolic processes. These medications improve the performance of the heart by improving appetite and heart muscle function.
If a child is diagnosed with a benign or malignant form of the disease, annual medical examinations should be carried out and the course of the disease monitored. This helps avoid complications while leading an active life.

Control of complications
Although the trabeculae in the left ventricle do not pose a threat to the child's health, if they are not treated properly, they can go from a benign (painless) form to a malignant form (requiring regular drug treatment). For this reason, upon detecting the disease, doctors immediately establish bans on the treatment of the patient. This includes:
- Extreme sports, athletic careers, strenuous gymnastics, excessive dancing, diving.
- Self-medication. The use of medications (including non-cardiac ones) and their dosage must be approved by a specialist. Many pharmacological drugs affect intravascular pressure and increase heart rate, which is unacceptable in this type of pathology.
- Intense physical and emotional exertion.
In addition, the doctor issues a certificate prohibiting the child from participating in school sports competitions and exempting him from certain sports. He will design the range of activities so that the child's additional left ventricular attachment can be trained and will not be affected in the future. The following activities are shown:

- Easy, short jogging.
- Walking on a rope.
- Mobilization exercises.
- Jumping with a skipping rope.
- Gymnastics exercises on the rope, on the wall bars, on benches, with a ball.
In addition, a baby with an extra thread will benefit from attending a massage course, eating properly, attending slow dances, resting more often and avoiding stressful situations.
The best way to deliver a healthy baby is to avoid factors that can negatively affect fetal development (throughout pregnancy). If the expectant mother has such a condition, it is worth taking it much more seriously. This can reduce the risk of an additional umbilical cord. If your baby has already been born with this pathology, you should keep a close eye on his well-being and follow any advice from your doctor so that your baby grows and develops in line with his peers.
lifestyle
A special lifestyle is not required for a child with an additional tendon. A sensible diet with fortified foods, long walks outdoors and normal physical activity is sufficient. There is no point in restricting your child to exercise or sport. Your child can actively run, jump and engage in any physical activity that is age-appropriate and practiced at the educational institution he or she attends. Swimming, figure skating and ice hockey are welcome.
As for vaccinations according to the national calendar, it can be said that the complementary chorda medica. is not a distraction and the child can be vaccinated according to their age.

As the child matures and enters the difficult phase of adolescence, it is important, among other things, that Avoid unhealthy habits and maintain a healthy lifestyle. If there are age-related cardiovascular symptoms (sweating, fatigue, palpitations, shortness of breath), the adolescent should be taken to a cardiologist and, if necessary, prescribed or injected with the above medications.
Of course, pregnancy is not a contraindication for girls with an additional chordoma. If several of the congenital heart anomalies are present, an ultrasound scan of the heart during pregnancy and monitoring by a cardiologist is recommended.
Military service is not a contraindication for young men. An abnormal heart rhythm and the development of heart failure, which is also rare with an additional cardiac cord, are an exception to military service.
A few more words about nutrition for children and adults with structural or functional heart anomalies. Fatty, fried, salty and smoked foods should be avoided if possible. Fresh fruits and vegetables, natural juices, fermented milk products and low-fat fish should be preferred. Red and black caviar, apricots, sultanas, tomatoes, carrots, bananas and potatoes, rich in substances useful for the heart muscle, are welcome. In addition, grain products such as various breakfast cereals should be included in the daily menu. Of course, the child should not eat chips, canned carbonated drinks or any fast food, as this can lead to obesity, and excess weight is very bad for the heart muscle and vascular wall in the future.
Can there be complications?

There are usually no complications following an abnormal chordee. If the patient is at risk of cardiac arrhythmias for any reason, thromboembolic complications (pulmonary embolism, ischemic stroke, etc.) may occur. Cardiac arrest with fatal ventricular conduction disorders (ventricular fibrillation and paroxysmal ventricular tachycardia) can also occur.
The prognosis for children with additional struts in the left ventricle is favorable in both childhood and adulthood.
Causes of Spinal Extrusion
- trauma
- Obesity and other endocrine disorders
- Hypodynamics
- Tumors on the spine
- Previous spinal infections
- excessive physical activity
- congenital malformations of bones and connective tissue
- Chronic alcohol and nicotine intoxication
- Diseases that are associated with immunosuppression (impaired immune reaction)
It is often asymptomatic and its clinical manifestations are due to nerve ending involvement.
Lumbar disc extrusion is accompanied by:
- Lower back pain that radiates to the lower limbs, often in response to physical exertion
- Spatial dependence of back pain on body position – the pain decreases when lying down and increases when bending over
- Muscle weakness in the legs
- Paresthesias (sensory disturbances)
If the V. lumbar and I. sacral roots are involved, pain occurs below the knee, in the foot and in the toes. Discomfort on the front and outside of the thighs is typical of nerve trunk IV involvement.
Thoracic disc extrusion can disguise itself as a somatic disease of internal organs - angina, gastritis, intestinal dyskinesia, peptic ulcer, etc.
Convexity of the cervical spine is manifested by neck pain, dizziness, numbness in the back of the head and weakness of the arm muscles.
Stages of development
The degenerative process begins with the gelatinous nucleus (nucleus pulposus), which is usually a gelatinous mass with high viscosity and elasticity. The chondrocytes ensure constant metabolism: These structures synthesize and split proteoglycans for the matrix of the nucleus pulposus, which retains water and collagen in the fibrous ring. A healthy intervertebral disc maintains a certain level of pressure.
Abnormal mechanical axis tension due to the combined effects of adverse heredity, age, inadequate metabolic transport, and trauma leads to chondrocyte breakdown and nucleus pulposus degeneration. This structure loses moisture. Dehydration leads to a decrease in intravertebral pressure, and the mechanical stress is transferred to the fibrous ring, where microcracks, up to rupture, form. Part of the disc falls out through the tear as the load on the spine increases, and a fragment larger than the base of the disc falls out by extrusion.
Rules of life
If a child is found to have an extra tendon, it does not make the child sick. Parental concern about the presence of a 'malformation' can lead to isolating the child from 'possible difficulties' - but by this behavior the parents, who want to protect their child, prevent their child's socialization and make them sick themselves.
However, there are some restrictions: Competitive sports with high physical exertion are not permitted.
The rules for dealing with a person with an extra tendon in the left ventricle of the heart are simple, and following them will help avoid complications:
- Stick to a work and rest schedule.
- Make sure you get enough sleep, at least 8 hours.
- Eat a balanced diet.
- Avoid fatty, fried foods and fast food.
- Do physical, hardening exercises.
- Avoid stressful situations.
- Avoid heavy physical work.
- Get a firming massage once a year.
- Take your medication as prescribed by your doctor.
- Get annual physicals and checkups with a cardiologist.
Children with extra left hamstring strain can benefit from clubs and activities. The choice of sports club should be made after consultation with the cardiologist and taking into account the child's wishes and abilities. Appropriate activities for this child include:

- ballroom dancing;
- athletics (non-professional);
- wall climbing;
- Short distance hiking and camping.
It is also worth protecting your child from extreme activities that involve danger, risk and adrenaline:
This diagnosis does not exempt you from military service. A young person who develops complications in the form of persistent cardiac arrhythmias and circulatory failure cannot be recruited.
prognosis and prevention
No measures have yet been developed to prevent the development of threads in the heart cavities. Doctors have not yet learned how to alter the human genetic code.
However, pregnant women should give up bad habits, especially smoking, avoid contact with harmful chemicals, and eat a healthy diet.
In most cases, the prognosis for an additional left ventricular string is favorable. The body adapts to the presence of the anomaly as it ages, and it does not become noticeable or cause any discomfort.
The prognosis is somewhat less favorable if there are multiple tendons in the compartment and the cords are arranged transversely.
Treatment of cartilage damage
To prevent the acute form from turning into a chronic one, treatment should be initiated immediately. If treatment is initiated too late, the tissue begins to suffer significant damage and turn into shreds. The destruction of the tissue leads to degeneration of the cartilage, which in turn results in osteoarthritis of the knee and immobility.
Stages of conservative treatment
The conservative method is used in the acute, untreated stage at an early stage of the disease. Conservative therapy consists of several steps.
- Eliminate inflammation, pain, and swelling with nonsteroidal anti-inflammatory drugs (NSAIDs).
- If the knee joint is blocked, repositioning is carried out using manual therapy or traction.
- Therapeutic gymnastics.
- Therapeutic massage.
- Physiotherapy.
- Treatment with chondroprotectors.
- Treatment of the joint with hyaluronic acid.
- Treatment with folk remedies.
- Treating pain with analgesics.
- Applying a plaster cast (on the recommendation of the doctor).
Stages of surgical treatment
Surgical intervention is only performed in extreme cases when the tissue is damaged to the extent that it can no longer be repaired or when conservative methods have failed.
The surgical techniques to repair a cartilage tear consist of the following procedures:
Movement
So, knee injuries are an injury that is much more common than other injuries. Several types of meniscus injuries are known in traumatology: anterior horn tears, posterior horn tears and medial tears. These injuries can vary in size and shape, and there are several types: horizontal, transverse, oblique, longitudinal and degenerative. The tear of the posterior horn of the medial meniscus is much more common than that of the anterior or middle horn. This is because the medial meniscus is less mobile than the lateral meniscus and therefore more pressure is placed on it during movements.
Cartilage damage can be treated either conservatively or surgically. The treating doctor will decide which method is best for you based on the extent of the injury, its form (acute or chronic), the condition of the cartilage in your knee and the type of tear (horizontal, radial or combined).
Your doctor will almost always try conservative treatment and only attempt surgery if that treatment is not effective.
Treatment of cartilage injuries should be started as soon as possible, otherwise chronic injuries can lead to complete destruction of the joint tissue and immobilization of the knee.
To avoid injuries to the lower limbs, twisting, sudden movements, falls and jumps from a height should be avoided. Physical activity is usually contraindicated after meniscus treatment. Dear readers, that's it for today. Share with us your experience with meniscus injuries in the comments, how did you solve your problems?
Read more:- ectrodactyly.
- How to determine leg shortening.
- Description of the human foot bone.
- flatfoot μb.
- Toe movement in children.
- A child begins to have clubfoot between the ages of 1 and 5.
- Causes of tiptoe walking in babies.
- Why are a teenager's toes crooked?.
