Every surgical procedure involves pain in some form. In general, we try to minimize pain after surgical treatment of the longitudinal and transverse arches of the foot. Typically, the anesthesiologist will perform a pharmacological block before surgery to numb the pain in the foot for about 30 hours. After this time, the worst wave of pain is over and the transverse longitudinal flatfoot can be treated with the usual medications. We will do everything we can to relieve the patient of the pain.

- flat feet
- Types and forms of flat feet
- Longitudinal-transverse flatfoot: Who is suitable for surgical treatment?
- What happens before the operation?
- What is the risk of flat feet?
- Help yourself: 5 easy ways to combat flat feet.
- Method #1: Walking Barefoot
- Method 2: Therapeutic exercises
- Method #3: Massage
- CAUSES OF FLAT FEET IN ADULTS
- CAN FLAT FEET BE CORRECTED IN ADULTS?
- Movable form
- Rigid form
- Symptoms of Flat Feet
- types of flat feet
- Longitudinal flatfoot
- Clubfoot in children
- Types of acquired flatfoot
- Causes and risk factors for flat feet
- Symptoms and manifestations of flat feet
- types of pathology
- Causes of the disease
- Symptoms of Transverse Flatfoot
- Diagnosing flat feet
flat feet
Clubfoot is a form of foot deformity characterized by a lowering and flattening of the arch of the foot. It is caused by weakness and fatigue in the lower leg and foot muscles. The condition puts additional strain on the knees and has a negative impact on posture. The patient feels uncomfortable when walking and the gait is impaired.
The foot has two arches - a longitudinal and a transverse arch. Their main task is to maintain the balance of the body and provide cushioning when walking. When the arch muscles become weak and sag, flat feet occur.
- Excessive mobility, hypermobility of the joints;
- weakness of the lower leg and foot muscles, ligaments and bones;
- Spina bifida, cerebral palsy, plantar and soleus muscle paralysis, muscular dystrophy;
- congenital arch pathology (3 % cases);
- Arthritis; other skeletal diseases;
- Rickets;
- Poliomyelitis and cerebral palsy.

Types and forms of flat feet
A distinction is made between congenital and acquired flatfoot. Also, this condition can be divided into the following types:
- Longitudinal flatfoot.This group of defects is characterized by deformation of the longitudinal arch. It causes the foot to contact the ground over a large area. With longitudinal arch flat feet, the foot is often stretched. It occurs in 20 % patients, most commonly in children.
- Transverse flatfoot – Flattening of the transverse arch, causing deformation of the toes, blisters and pain in the forefoot area.
- Longitudinal transverse flatfoot In this disease, the symptoms of both deformities occur.
- Condylar flatfoot – Alignment of the axis of the foot with the heel and toes pointing outwards and the middle pointing inwards. It occurs more often in children.
There are three degrees of flat feet:
In first degree flatfoot there is no visible deformation. The patient complains of rapid fatigue of the feet and pain when putting on shoes. Another external symptom is morning swelling.
In second-degree flatfoot, the symptoms are moderate. The arch of the foot loses its shape, becomes slack and the pain spreads to the ankles and shins, becoming more intense and frequent. The muscles in the foot lose flexibility, which affects gait.
In the third degree of flat foot, the symptoms are even more pronounced and the deformity becomes even more severe. The affected person has persistent pain in the legs and the limbs swell. There are also severe headaches and lower back pain. The ability to work is significantly restricted and even walking short distances is severely hindered.
Longitudinal-transverse flatfoot: Who is suitable for surgical treatment?
The method of surgical treatment of longitudinal-transverse flat foot depends on the severity of the problem. The indication for surgical treatment should be conservative, as the disease can be treated conservatively. Due to the dynamic situation of the arch of the foot, good results can be achieved with regular training and special exercises to build muscle.
Surgical treatment of longitudinal-transverse flat foot is recommended only if the patient suffers from severe pain in the foot for a long period of time and if the pathology affects the patient's quality of life. Chronic tendinitis or a rupture of the tibialis posterior tendon make surgery unavoidable. Spastic deformities of the hindfoot associated with ankle osteoarthritis also require surgery.
What happens before the operation?
Before the operation, the doctors Doctors at the Joint Clinic The doctors at the Joint Clinic carry out a comprehensive clinical examination. One of the main diagnostic signs of a longitudinal-transverse flat foot is a deviation of the forefoot to the side, which is caused by a change in the longitudinal arch of the foot and results in almost all of the toes being visible when the foot is viewed from behind. Doctors call this phenomenon Too many toes sign. In patients without foot abnormalities, all toes point forward. A standing x-ray clearly shows the bone deformity and can confirm the doctor's concerns.
Another indication of combined flatfoot is a test called the single heel rise sign, which provides information about the condition of the tibialis posterior muscles. To do this, the doctor observes the position of the foot from behind while the patient is standing. Injuries to the tibialis muscle are likely when the axis of the ankle tilts inward. Another method for diagnosing tibialis posterior is magnetic resonance imaging (MRI). A podometric examination is recommended to analyze the load on the foot during standing and walking.
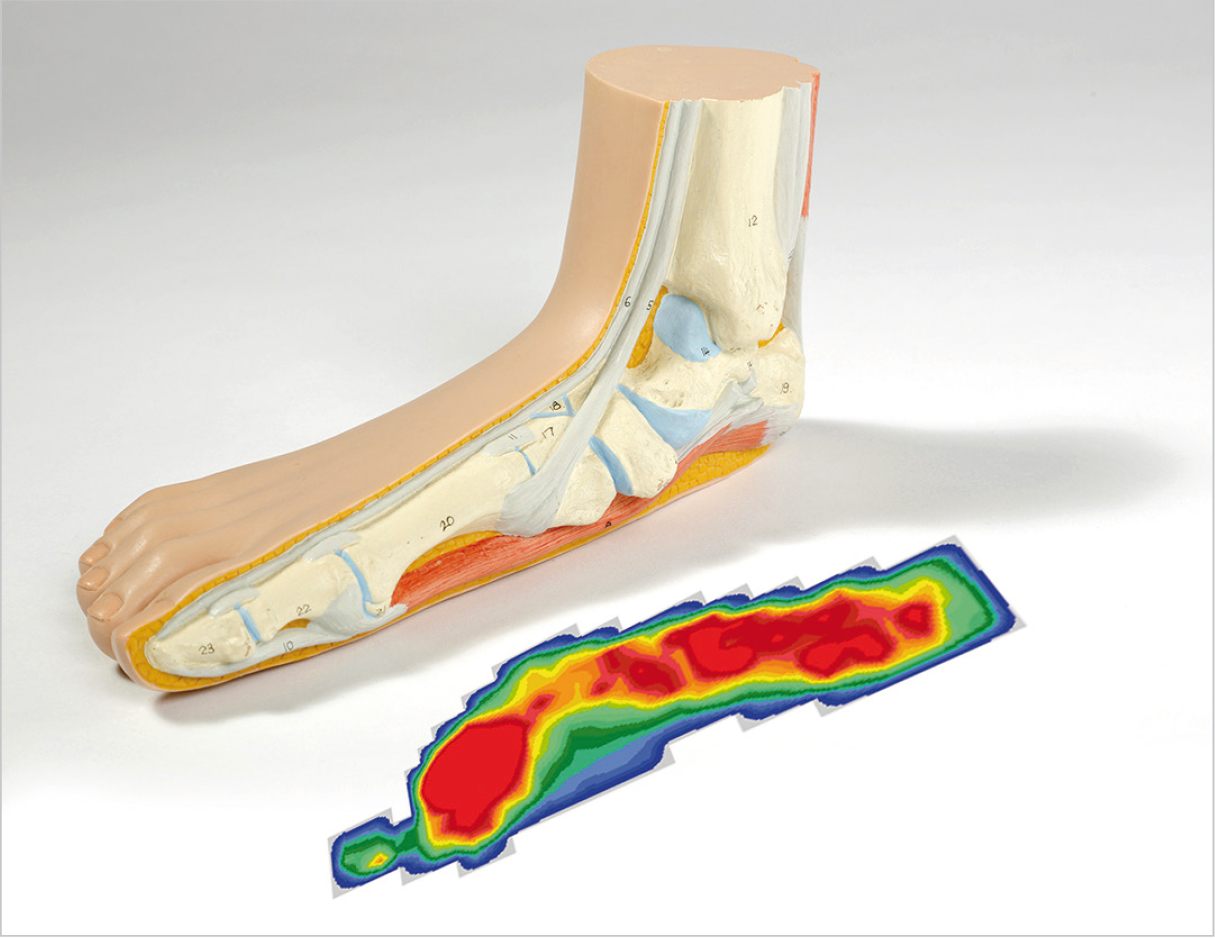
Longitudinal-transverse flat foot: measuring the size and condition of the foot (podometry). Anomalies in the longitudinal arch of the foot are determined by podometry: the pressure (area marked in red) is more evenly distributed than in a healthy person. If the longitudinal arch of the foot is normal, only the heel area and the fingertips are stressed. In this way, the longitudinal-transverse flat foot flattens the arch of the foot.
What is the risk of flat feet?
Flat feet hurt when walking, but this is not the biggest danger. But it can also have negative consequences:
- The ankles become deformed.
- Bumps appear on the foot
- Twisted or crossed toes
- Blood circulation in the lower limbs is impaired
- The feet become very swollen, painful and tired.
- Knee, hip and back pain occurs.
- Gait and posture may worsen.
- Clubfoot hurts when walking.
Help yourself: 5 easy ways to combat flat feet.
Remember the three-picture test from the beginning of this article? If the last two pictures apply to you, you should see your doctor as soon as possible. The sooner your podiatrist diagnoses the disease, the sooner you can take action and prevent the disease from progressing.
You can prevent flat feet or treat them yourself. There are several easy and relatively inexpensive ways to do this.
Method #1: Walking Barefoot
The absence of shoes allows the foot to form physiologically. This keeps the shape of the feet natural. In shoes, the foot does not receive enough freedom: it is squeezed by the walls of a tight shoe, when walking in stilettos, the toes twist, the pointed 'nose' of the shoe squeezes the toes into a heap and gradually deforms their joints. So if we wear shoes all the time, we have to 'eliminate' the foot problems: straighten the toes, fight the flat feet and put the joints in their correct position.
In addition, the barefoot foot receives a micro-massage through contact with the ground. In addition, blood circulation in the lower limbs is improved and the foot muscles are toned.
Let your feet relax! Walk barefoot on a textured surface more often:

Method 2: Therapeutic exercises
You can see a detailed gymnastics complex for flat feet from a podiatrist in our video.
Method #3: Massage
Massages are very effective when combined with physical therapy. Both massage and gymnastics are aimed at improving not only the foot muscles, but also the foot muscles in general. What are the benefits of foot massage for flat feet?
CAUSES OF FLAT FEET IN ADULTS
- Flat feet in childhood.
- Obesity causes many problems with the musculoskeletal system.
- Bad footwear. Unsupportive insoles, shoes that are too tight or too wide, high-heeled shoes - all of these lead to abnormal pressure distribution.
- Lack of regular exercise: walking, running barefoot.
- Prolonged standing on your feet.
- Foot Injuries: Sprains, torn ligaments, dislocations, broken bones in the past cause flat feet in adults.
- Connective tissue diseases.
- Lack of important elements: vitamins, minerals.
A healthy foot has two arches: longitudinal and transverse.
Depending on the disorder, these are differentiated:
- Longitudinal flatfoot – lack of physiological curvature on the inside of the sole. Usually visible at a young age. In severe forms, the foot tilts inwards and a valgus deformity of the ankle occurs.
- Transverse flatfoot occurs more often in adults. Ligament weakness leads to separation of the metatarsals and atrophy of the transverse arch. The severe form leads to a deformation of the metatarsophalangeal joint of the big toe - the well-known 'bony toe' or hallux valgus.
CAN FLAT FEET BE CORRECTED IN ADULTS?
Don't think that time is running out, don't accept foot and back pain! 'Dr. OST knows how to treat flat feet in adults! Unique non-surgical treatment methods using modern technologies can completely eliminate pain and correct gait and posture.
The cushioning properties of the foot can only be restored through a systemic approach. Orthopedists distinguish between a mobile and a rigid form of flat foot. The former is caused by weak ligaments, the latter by abnormal foot structure. The type of deformity determines the choice of treatment tactics for adults with flat feet.
Movable form
Programs for strengthening muscles and ligaments are effective for mobile flat feet:
- LFC. A competent rehabilitation therapist selects exercises for adults with flat feet after reviewing scans, plantography and visual inspection.
- Assessment by an osteopath, manual therapy and various types of therapeutic massage to improve blood circulation and muscle reactivation.
Rigid form
Treatment of longitudinal and transverse flat feet in adults with the rigid form is more difficult. It is effective in relieving pain and stopping pathological changes.
- Orthopedic insoles based on a breathable Turbocast material;
- taping;
- Individually adapted orthopedic insoles.
- To help, UWT can be performed, which helps make muscles and ligaments more flexible and mobile.
Symptoms of Flat Feet

In the initial stages, flat foot does not show any obvious degenerative changes. Later, as the disease progresses, unpleasant symptoms appear, causing discomfort even with grade 2 longitudinal flatfoot. Often, patients with flat feet complain of pain in the foot and the inability to endure prolonged physical activity. Cramps and burning in the lower leg, which are not accompanied by prolonged malaise or hypothermia, are also symptoms of flat feet.
- Enlargement of the bones of the big toe;
- stubborn calluses and corns;
- deformations of the toes;
- bad posture;
- back pain;
- Joint pain.
types of flat feet
The classification of flat feet is based on several criteria. Depending on the location, a distinction is made between transverse, longitudinal and combined flat feet.
Longitudinal flatfoot

This is a degenerative and progressive disease characterized by the prolapse of the longitudinal arch. This leads to a change in the structure and cushioning properties of the foot. As the pathology progresses, the loads are redistributed to other parts of the supporting apparatus, which contradicts nature and leads to health problems. The resulting abnormalities contribute to pathological changes in muscle tissue. As a result, the venous drainage and blood supply system no longer function fully. Longitudinal flatfoot is a chronic disease of the musculoskeletal system that progresses slowly, but always under the influence of various factors.
- Grade I The degenerative changes in the initial stage are minor. Prolonged daily physical activity leads to evening fatigue in the lower limbs. Another common symptom is swelling of the feet. Over time, dysbasia, or a gait disorder, develops. The height of the arch of the foot in flat feet grade I varies between 25-35 mm, which corresponds to an angle of 131-141°, while the normal value is 125-130°.
- Grade II The pathological process is moderately pronounced. The pain sensations intensify and extend to the foot region, also affecting the lower limbs. The muscles become weaker and gradually lose mobility. In flatfoot grade II, the sole height is 24-17 mm and the angle of inclination is between 141-155 degrees.
- Grade III. The foot deformity becomes clearly visible. The pain from prolonged exertion extends to the waist and becomes more persistent. Patients are often plagued by severe headaches. There is discomfort and other difficulties when walking, even for short distances. The arch height is less than 17mm and the foot angle exceeds 155 degrees.
Clubfoot in children
The cushioning function of the foot, which absorbs shocks when walking, running and jumping, is ensured by its anatomical structure. There are two pressure arches in the sole of the foot - a longitudinal and a transverse arch.
A toddler whose skeleton is still developing does not yet have an arch. The baby's foot is protected from injuries and overloads by a special fat pad, and in the first months of life all baby feet, without exception, are flat. By the third or fourth year of life, the natural support completely dissolves. Before this happens, only an experienced pediatric orthopedist can determine whether a child has flat feet. Regular check-ups are carried out, the first at 1 month of age, the next at 6 months and 1 year of age, and every year thereafter. As soon as the one-year-old child is able to stand on his feet and walk independently, parents should be particularly attentive.

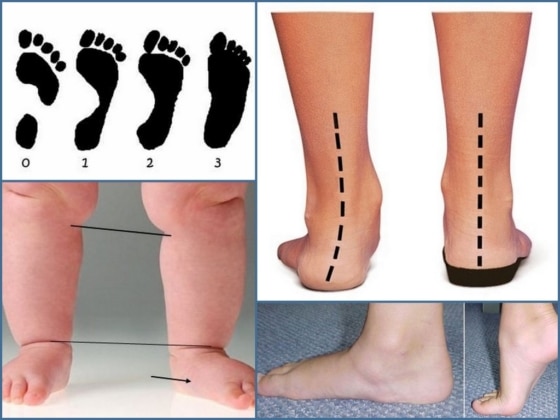
The most common congenital foot deformity is the so-called valgus deformity, in which the feet, placed parallel to each other, resemble the letter X: the heels and toes point outwards and the middle of the foot points inwards. This defect can be diagnosed at birth or during an initial examination by a pediatrician. Some parents are horrified by the word 'innate' because they believe that it is difficult or even impossible to correct this defect, while others believe that there is no such thing as a defect. Both views are wrong.
Congenital pediatric flatfoot can be successfully treated conservatively and with support:
Timely intervention plays a big role. Advanced flat feet are difficult and sometimes impossible to treat. In childhood, when the skeleton is still growing, the risk of adverse consequences increases if the situation is delayed.
Types of acquired flatfoot
Acquired transverse and longitudinal flatfoot in children develops between the ages of 5 and 14. Longitudinal flatfoot is more common than transverse flatfoot: it accounts for more than 70 % of all cases. Foot deformity occurs in the middle and late stages of the disease, but the first symptoms of flat feet in children appear much earlier. This includes:
- Poor foot position – photos of flat feet in children illustrate this symptom most clearly;
- Fatigue and pain in the feet after physical activity – walking or running;
- Uneven wear of the heel in the shoe - closer to the inside edge.
These symptoms should alert parents and prompt a visit to an orthopedist. If a foot deformity is detected, the doctor will recommend therapeutic measures. The most important element is therapeutic massage and exercises, which should be done regularly at home. The correction of flat feet in preschool children takes place in kindergartens, where educators are involved in hardening children and doing special exercises that help prevent the disease.
Flat feet can be diagnosed at home without resorting to sophisticated diagnostic equipment. To find out if your child has flat feet, you should:
- Lubricate the soles of the feet with a greasy cream;
- Take a clean white sheet of paper;
- Place the child's foot on the paper and press the sole against the paper as hard as possible;
- Carefully remove the foot from the paper and draw a straight line on the inside of the foot from the heel to the base of the big toe.
A line is drawn perpendicular to this line from the point where the foot is most flexed. If the footprint is less than half the vertical length at the narrowest point, everything is normal, but if it is larger, it is the beginning of a flat foot.
Causes and risk factors for flat feet

Among other things, the following play a decisive role in the development of this condition. Heredity and lack of physical activityThis means a sedentary lifestyle. Under the influence of these and other unfavorable circumstances, the muscles and ligaments that support the foot are weakened, The foot becomes deformed and loses its cushioning ability.. A distinction is made between transverse and longitudinal flat feet, depending on which arch of the foot is pathologically changed (lowered). A combined flat foot, i.e. a combination of both forms, is often diagnosed.

It should be noted that Transverse flatfoot – is only a problem for adults, children do not suffer from it. Some children are born with devalved feet, which is physiologically normal, but often they have flat feet, which manifests itself in a much more physiological way. In such cases, the situation should not be underestimated, a podiatrist should be consulted, and this condition should be corrected from an early age, as soon as the child begins to walk (at about one and a half years of age). Therapy usually consists of wearing orthosesand special exercises as well as therapeutic massages. The diagnosis of flat feet may not be made until the age of seven. Early treatment can prevent gait disorders and the worst consequences of flat feet: increased pressure on the joints and the appearance of early osteoarthritis.
In addition to heredity and a significant lack of exercise, the following causes can contribute to the development of flat feet:
- excessive weight;
- Frequently wearing shoes that are too tight and uncomfortable, high heels;
- Effects of previous trauma: sprains, fractures, soft tissue injuries in the foot;
- osteoporosis, rickets;
- muscle paralysis of the foot;
- Excessive and prolonged stress on the feet (athletic training, heavy physical work, long standing, stress associated with pregnancy, etc.).
Symptoms and manifestations of flat feet
Regardless of your concerns, you should not engage in self-diagnosis and treatment as this will not produce the necessary positive results and may even be dangerous. If you suspect that you have flat feet, you should consult an orthopedist who, after an examination, will diagnose the foot deformity or, if another pathology is detected, refer you to another specialist (some of the signs of flat feet can also be symptoms of varicose veins or other illnesses). So what are the signs to suspect flat feet?
- tired legs or pain in the feet after standing for long periods or other physical activities;
- Swelling, heaviness and cramps in the calves are likely;
- shoes slipping on one side;
- pain in the knees, hips and lower back;
- The need to purchase larger shoe sizes than before.

With longitudinal flatfoot The pain in the feet is persistent, the feet are swollen and pressure on them can cause pain in some cases. The pain can also be felt in the lower extremities, and the spine can also be affected. Transverse flatfoot is characterized by deformation of the forefoot and toes, pain in the forefoot, blistering, and problems choosing and wearing shoes.
The development of longitudinal flatfoot occurs in three stages. In the first stage, there are minor changes in the shape of the feet, but the feet may be sore and swollen after heavy physical exertion, but are back to normal in the morning. In the second stage, the foot changes shape more drastically, flattening significantly and the arches of the feet begin to flatten. The pain is intense, affecting the ankle and spreading to the upper joints, knee and hip, with fatigue and pain occurring with prolonged walking. In the third degree, the foot is severely deformed and walking in normal shoes is completely impossible, the constant pain makes the affected person unable to work and sit, and the quality of life suffers.
types of pathology
A distinction is made between congenital (very rare) and acquired flat feet.
According to another classification, there are two types of flat feet
- Longitudinal arch – the longitudinal arch is flattened, making the foot elongated;
- Transverse – the transverse arch is flattened, making the foot wider;
- Combined or longitudinal-transverse vault - both vaults are disturbed.
Depending on the cause of the lesions, a distinction is made between static flatfoot (in 82 % cases), ricochet, paralysis and traumatic flatfoot.
Causes of the disease
Foot deformity can be caused by various factors:
- Trauma (fracture of the foot or ankle, damage to the arch of the foot);
- muscle paralysis of the feet, which may develop after polio;
- Rickets – the bones become soft and malleable, causing them to deform under the weight of the body;
- Weakening of the musculoskeletal system so that it is no longer able to hold the arch of the foot in the correct position.
- congenital anomalies;
- lack of exercise, sedentary lifestyle;
- age-related changes;
- unsuitable footwear (narrow toes, high heels);
- Excessive pressure on the foot due to excess weight, pregnancy or work (hairdressers, salespeople).
Symptoms of Transverse Flatfoot
Symptoms of transverse flatfoot
– The most common are: Pains in the feet, Burning, cramps. in the muscles of the lower leg, fatigue Tiredness in the feet at the end of the day. In advanced stages, knee pain, hip pain and back pain may also occur, leading to the development of osteoarthritis these joints can lead.
The forefoot visually enlarges, creating a so-called crooked foot. As a result of the abnormal load distribution caused by flat feet, it often occurs Deformity of the first toe The first toe is often curved into a valgus position. There is often an exophyte in the area of the big toe joint, which patients refer to as'Bunion' or 'bump''describe on the foot. The 2-3-4 toes, which are heavily stressed, take on a hammer toe shape. As the disease progresses, the changes continue in the form of forefoot deformity, which leads to a violation of the biomechanics of all parts of the musculoskeletal system involved in walking.
Diagnosing flat feet
Diagnosis of flat feet requires an examination by a podiatrist. An x-ray examination of the feet. And an analysis of the patient's gait. If necessary, the range of examinations can be expanded.
Treatment of paraplegic flatfoot should be carried out by a traumatologist after a thorough diagnosis. Treatment depends on the severity of the flat foot. Treatment of transverse flatfoot can be surgical or conservative (without surgery).
Conservative treatment of transverse flatfoot is comprehensive and includes reducing foot loads, selecting orthopedic shoes, orthopedic aids to normalize biomechanics and reducing excess weight. In the case of bursitis or osteoarthritis of the first metatarsophalangeal joint, anti-inflammatory and pain-relieving medications are used to relieve the inflammation. In some cases, immobilization, physical therapy, and massage are used to reduce increased muscle tone and therefore pain. Conservative treatment aims to relieve pain and slow the progression of paraplegic flatfoot.

Preparing for surgery
Cross-sectional flatfoot

surgery
In transverse flatfoot

- Which ligaments strengthen the transverse arch of the foot?.
- Determining the number of longitudinal arches in the human foot.
- The longitudinal arch of the foot is.
- The longitudinal arches of the foot begin at the bone.
- Transverse arch of the foot Latin.
- Valgus flatfoot (valgus flatfoot).
- Which doctor treats flat feet?.
- Transverse orthopedic insoles.

