To be honest, this name has always confused me. It depends where you count from, doesn't it? However, the anatomists of antiquity came up with such a name, so we must remember this muscle as the third fibula.
- Musculoskeletal Ultrasound: Lower Limb Injuries. Part 2
- Tear of the soleus muscle
- structure
- function
- function
- posture and balance
- When the peroneal muscles are overly tight.
- With excessive tension and weakness of the periosteal muscles
- Stretching-Guru.ru
- Long thigh muscle
- symptoms
- causes
- treatment options
- Video about our clinic for traumatology and orthopedics
- Lateral shin muscle group
- 1. long shin muscle (musculus fibularis longus)
- Human Fibula Anatomy Information:
- Which doctors should you visit for a fibula examination:
- Types of fibula fractures
- Symptoms of a fibula fracture
- Diagnosis of femoral neuropathy
- Treatment of femoral neuropathy
Musculoskeletal Ultrasound: Lower Limb Injuries. Part 2
A tear in the medial head of the calf muscle, known as 'tennis foot', most commonly affects middle-aged athletes who experience a sharp pain in the mid-shinbone region when ankle flexion is active while knee extension is active.
When evaluating symptoms to suspect a rupture, physicians should also consider the alternative diagnosis of deep vein thrombosis, which may also present with symptoms.
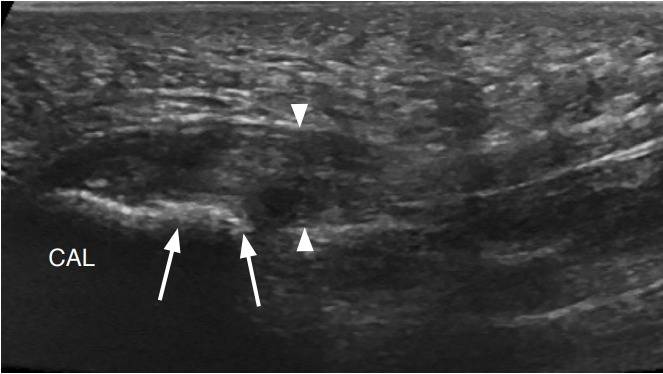
The medial head of the calf muscle is best assessed in the longitudinal plane. Ultrasonographic features of the tear include disruption of the normal alternating linear hyperechoic and hypoechoic appearance at the distal muscle-tendon junction, where hypoechoic bleeding replaces the normal conical appearance of the distal aspect (Figure 10).
Large tears are characterized by retraction and heterogeneous fluid extending proximally between the medial head of the calf muscle and the soleus.
Figure 10. : A 30-year-old woman with a tear of the medial head of the calf muscle (tennis leg).
Ultrasonography along the long axis of the tibia to the distal medial head of the calf muscle (MG) shows an irregular and hypoechoic distal myotendinous junction (arrowheads) with a small hypoechoic hematoma (curved arrows) between the MG and the cambial muscle (S). Compare with the normal appearance of the muscle (arrows).
Tear of the soleus muscle
Patients with a soleus tendon rupture describe a sudden onset of pain in the calf muscle that they feel as a blow or direct impact, similar to patients with a medial calf muscle head injury.
The soleus muscle begins at the posterior superior aspect of the lateral condyle of the thigh and extends downward and medially along the posterior aspect of the knee. The long and thin longitudinal tendon that sits between the soleus and the medial head of the calf muscle terminates either at the calcaneus adjacent to the posteromedial aspect of the Achilles tendon or at the Achilles tendon itself.
Ultrasonography diagnoses a soleus tendon rupture by the absence of a normal soleus tendon with heterogeneous hypoechoic fluid in the form of a hematoma at a suspected site between the soleus muscle and the medial head of the calf muscle (Figure 11).
Figure 11 : 32-year-old woman with plantar fasciitis.
Ultrasonography of the long axis of the tibia to the medial head of the calf muscle (MG) shows a heterogeneous hypoechoic hematoma (arrowheads) accompanying the medial head of the calf muscle and the cambium muscle (S). The soleus tendon was not observed.
structure
It arises from the head and the upper two-thirds of the lateral surface of the shaft of the fibula, from the deep surface of the fascia, and from the intermuscular space between it and the muscles of the anterior and posterior legs; sometimes also by some fibers from the lateral condyle of the tibia. Between its attachments at the head and the shaft of the fibula there is a gap through which the common peroneal nerve passes to the anterior part of the leg.
It terminates in a long tendon that runs behind the lateral ankle in a common groove and tendon of the peroneus muscle; this groove is converted into a canal by the superior fibula, and the tendon is contained within it in a common mucous membrane.
The tendon then passes at an anterior angle through the lateral side of the foot, beneath the perineal tubercle and tendon of the fibula muscle, and beneath the sheath of the inferior portion of the preserved fibula.
It crosses the lateral side of the elbow, and then runs along the underside of that bone in a groove which becomes the fibula canal through the long plantar ligament; the tendon then crosses the sole of the foot at an angle and inserts on the lateral side of the base of the first metatarsal and on the lateral side of the medial sphenoid bone.
Sometimes it also attaches to the base of the second metatarsal.
The tendon changes direction in two places: first behind the lateral ankle, second at the elbow; in both cases the tendon is thickened, and in the latter case a sesamoid fibrocartilage (sometimes a bone) usually forms in its substance.
function
The tendons of the long and short fibula of the foot, together with the posterior tibialis muscle, counteract the anterior tibialis muscle and posterior fibular muscle (peroneus tertius), which form the dorsiflexors of the foot.
The long fibula also supports the sole of the foot and is an important factor in maintaining the transverse arch due to the oblique course of the tendon through the sole of the foot.
The eye muscles, which have their fixed point at the bottom, serve to keep the foot on the instep.
This is especially true in the one-leg stand, where the dominant body weight tends to throw the leg inward; the long fibula counteracts this tendency by pulling the leg laterally.
function
The short and long fibula have the function of flexing the plantar (plantar) muscle (with the inner edge of the foot pointing down and the outer edge pointing up) and also retract the foot laterally.
The third fibula, in conjunction with the other muscles, elevates the lateral (outer side) edge of the foot.
All three peroneal muscles play an important role in the dynamic stabilization of the foot and the entire ankle. These muscles are essential when walking on uneven or rocky surfaces. By fulfilling their function of stabilizing the ankle, they protect us from potential ankle injuries (such as a sprained ankle).
posture and balance
Everything in the human body is interconnected and interdependent. Problems in the ankle area can affect the entire biomechanical chain of our body (knee, pelvis, spine). Let's look at some examples:
When the peroneal muscles are overly tight.
The foot is then in excessive pronation. In this position, the inner edge of the foot is lower than the midline. It's easy to determine: look at the sole of your shoe and if you're rubbing the inside edge of your heel, there's a good chance that muscle group is overstretched.
This condition often leads to ankle injuries and chronic conditions (such as tendinitis). The head of the fibula can also shift under prolonged stress, which leads to a change in the biomechanical movement sequences and the development of pain in the knee, hip and lumbar spine.
Relaxation of the periosteal muscles can be achieved through a combination of myofascial massage and mobility exercises of the lower leg and ankle.
With excessive tension and weakness of the periosteal muscles
– The long fibula stabilizes the foot. When weakened, it can cause pain in the foot.
– The peroneus muscle group helps us to land after a jump. If they are weak, dislocations or even tears of the ankle ligaments are possible.
In this case, we recommend that you seek advice from your doctor or trainer on the best way to incorporate periosteal strengthening exercises into your exercise regimen.
Stretching-Guru.ru
Spinning - possible for all age groups and independent of the degree of mobility! However, without preparatory exercises, sitting down to twist is not only difficult, but also risky: you can overstretch your muscles and injure yourself.
Below are the best longitudinal and transverse thread mastery exercises that will gently and painlessly stretch your muscles and joints.
Long thigh muscle

Latin name name fibula—rod, shaft; longus—long.
The direction of insertion of the long fibula tendon supports the transverse and lateral longitudinal arches of the foot.
Place of origin: Upper 2/3 of the lateral surface of the fibula. Lateral condyle of the tibia.
attachment point: Lateral side of the medial side of the ischium. Base of the first metatarsal.
Activities: Stretches the foot. Participates in plantar flexion of the ankle.
Unnamed: Superficial oculomotor nerve of L4, 5, S1.
vascular supply: Arteria oculi via posterior tibial artery (from the popliteal artery).
Main functional movement: Example: Walking on an uneven surface.
This article was written on wikipedia
Do you have a question?
If you still have any questions or misunderstandings after reading the article, please ask us in the comments below or write to us in the official Facebook group. You will receive an answer as soon as possible.
symptoms
Trigger points in the long fibula transmit pain to the outside of the ankle (Fig. 10.13).
The pain is usually concentrated on and under the lateral malleolus (malleolus - Latin malleolus - is the outer bone of the ankle or the prominent end of the fibula). Sometimes the pain is also located in the middle third of the shinbone on the outside and along the outer edge of the foot (not shown). The entire ankle is usually sensitive to touch, while if a ligament is torn, the sensitivity is localized. Pain and tenderness in the ankle are often frightening signs of arthritis.
A common diagnostic error is tendonitis of the trigger points of the calf muscle, which is characterized by ankle weakness. In addition, the compression of nerves by this muscle can cause numbness in the lower leg, ankle, and upper foot. Muscle weakness makes it difficult to lift the foot. If the nerves are pinched, the weakness may not be accompanied by pain. These symptoms are similar to those of a pinched nerve in the spine due to disc damage.
Before any conclusions can be drawn about the spine, the trigger points in the peroneal muscles must be treated, although in some cases both conditions can be present.
causes
Excessive walking, running and climbing are necessary conditions for the development of trigger points in the long peroneal muscles. Walking is particularly damaging to these muscles if one leg is shorter than the other, if you have flat feet or Morton's foot (read more about Morton's foot in the dedicated section).
Sleeping on your stomach or back with your feet propped up puts your muscles in a shortened state. If you're not too tidy, try folding down the covers to give your legs and toes more room. High-heeled shoes put a strain on the lower leg muscles because they shorten and stiffen them. In high-heeled shoes, the weight of the body rests on the toes, and the periosteal muscles are in a state of contraction to maintain balance.
Stockings or therapeutic socks compress muscles and contribute to trigger points. Crossing your legs while seated puts pressure on the ankle nerves, causing numbness and muscle weakness. The squatting position has the same effect on the nerves and vessels, in addition to causing pathological tension in numerous muscles, including the hamstrings. Trigger points develop in all cases in which an unnatural posture is maintained for too long.
treatment options
Surgical intervention may be indicated when conservative management is ineffective for conditions such as tendonitis, partial tendon rupture, tendinitis, and tendinopathy of the fibula tendon.
So far, only open procedures have been performed. Cast immobilization is often required in the postoperative period to prevent the ankle from stiffening and allow the wound to heal.
Thanks to improvements in equipment and the development of new micro-instruments, it is now possible to perform such interventions endoscopically. This type of intervention has several advantages: it is better tolerated by patients, causes less postoperative pain and allows for early functional treatment and monitoring of the patient in an outpatient setting.
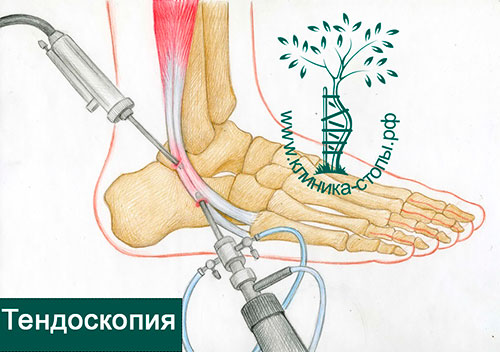
Minimally invasive endoscopic tendon surgery is called tendoscopy. It is performed through two skin punctures, one inserted through an endoscope connected to a video camera and the other through microtools that allow various manipulations on the tendon.
During the procedure, it is possible not only to diagnose the problem, but also to repair it using special tools. The operation is performed on an outpatient basis under general, regional or local anesthesia.
Video about our clinic for traumatology and orthopedics
Lateral shin muscle group
1. long shin muscle (musculus fibularis longus)
Imagine that we have removed the skin and subcutaneous fat from the cadaver, as well as the superficial fascia, the vessels and everything else so that we have the muscles in front of us. In this case, the first anatomical formation we see on the lateral side of the tibia is the hamstring longus.
This fairly powerful muscle covers the lateral edge of the tibia. It's also the long fibula that the lateral contours of upper part of the tibia so that it can be seen in a living human being.
In Sinelnikov's atlas there is an excellent drawing where you can admire this muscle:
I chose Gray's atlas to show this muscle from the posterior side:
I paste both images without my underlining and highlighting:
This is a very good fix to try to find the already dissected muscle on the plates without pointers and underlining.
The beginning: Head and upper 2/3 of the lateral surface of the fibula, lateral condyle of the tibia;
Approach: Tubercle of the first metatarsal, base of the second metatarsal (sole);
Function: Elevation of the lateral edge of the foot.
Human Fibula Anatomy Information:
calf bone, fibula (Greek regope), is a thin and long bone with thickened ends. The upper (proximal) epiphysis forms the head, caput fibulae, which articulates with the lateral condyle of the tibia via a flat, round articular surface, facies articularis capitis fibulae. A bony prominence, the apex capitis fibulae, projects posteriorly and laterally upward from this surface.

The shaft of the fibulae is triangular and slightly twisted along its long axis. The diaphyseal rim of the bone that faces the tibia and serves to attach the membrana interossea cruris is called the margo interossea. The lower (distal) epiphysis of the fibula thickens and forms the lateral malleolus, malleolus lateralis, with a smooth articular surface, facies articularis malleoli.

Which doctors should you visit for a fibula examination:
Are you worried about something? Would you like to learn more about the fibula or do you need an examination? You can make an appointment with dr. – Clinic Eurolaboratory is always there for you! The best doctors will examine you, advise you, provide the necessary care and diagnose the problem. You can also doctor at home. clinic Eurolaboratory is open for you around the clock.
How to contact the clinic:
The phone number of our clinic in Kiev is (+38 044) 206-20-00 (multichannel). The clinic receptionist will arrange with you a convenient day and time to visit the doctor. Our coordinates and directions can be found here. For more information about all of the clinic's services, visit the clinic's website.
If you have been examined before Be sure to take the results with you to your doctor's office. If you have not yet done any examinations, we will carry out the necessary work in our clinic or with our colleagues in other clinics.
It is important that you take a close look at your general health. There are many diseases that do not manifest themselves in our body at first, but, unfortunately, are treated too late. It is enough if you go to the doctor several times a year Go for a medical check-up several times a yearIt's important to get checked up several times a year, not only to prevent a serious illness, but also to maintain a healthy body and mind.
If you want to ask your doctor a question, use the online guide, where you will find answers to your questions and read Self Care Tips. If you are interested in opinions about clinics and doctors, you will find the information you need in the forum. Also register on the medical portal Eurocoolto keep up to date with the latest fractured fibula news and information on the site, which will then be automatically sent to your mailbox.
Types of fibula fractures
Types of fibula fractures include:
- Lateral Fibula Fracture – occurs when the fibula is broken at the ankle joint;
- Proximal fibula head fracture – located at the top of the fibula near the knee joint;
- Avulsion fracture - a fracture in which the tendon tears off part of the bone on the attachment side;
- Stress fractures result from repeated trauma while running or walking;
- Fibula fractures are common in athletes, especially those involved in running, jumping, soccer, and basketball.
Symptoms of a fibula fracture
Pain and swelling are some of the most common symptoms of a fibula fracture. Other signs and symptoms include:
People with a fibula fracture should see a doctor for a diagnosis. The diagnostic process includes:
- Objective investigation. – The doctor pays attention to conspicuous deformations;
- X-ray – serves to determine a broken bone or a dislocation;
- MRI ( MRI ) – provides a more detailed examination and can provide detailed images of the internal bones and soft tissues;
- Computed Tomography ( COMPUTED TOMOGRAPHY (CT SCAN) ) and other techniques can be performed to make an accurate diagnosis and assess the severity of a fibula fracture.
Diagnosis of femoral neuropathy
The diagnostic algorithm for peroneal neuropathy is based on anamnesis, which can provide information about the development of the disease, and a thorough examination of the motor and sensory function of the peripheral nerves of the affected limb. The muscle strength of the individual lower leg and foot muscles is assessed with special function tests. Superficial sensitivity is analyzed with a special needle. In addition, electromyography and electronography are used to determine the degree of nerve damage based on the speed of action potentials. More recently, nerve ultrasound has been used to study the structure of the nerve trunk and adjacent structures.
Traumatic neuropathy requires a consultation with a trauma surgeon, an ultrasound or x-ray of the knee joint, an x-ray of the tibia, and if indicated, an ultrasound or x-ray of the ankle. In isolated cases, a diagnostic Novocain nerve block can be performed.
Peroneal neuropathy requires differential diagnosis with LV-SI radiculopathy, hereditary recurrent neuropathy, Charcot-Marie-Tooth disease, PMA syndrome (peroneal muscular atrophy), ALS, polyneuropathy, other lower limb mononeuropathies, brain tumors and medullary tumors.
Treatment of femoral neuropathy
Patients with peroneal neuropathy are treated by a neurologist. The surgical treatment is decided by a neurosurgeon. One element of treatment is elimination or reduction of the causative agent of the neuropathy. Conservative treatment uses the anti-inflammatory and analgesic effects of drugs from the group of NSAIDs (diclofenac, lornoxicam, nimesulide, ibuprofen, etc.). This group of drugs is combined with B vitamins, antioxidants (thioctic acid) and drugs that improve nerve blood flow (pentoxifylline, nicotinic acid). Prescribing ipidacrine, neostigmine is aimed at improving neuromuscular transmission.
Pharmacotherapy is successfully combined with physiotherapy: electrophoresis, amplipulse therapy, magnetotherapy, electrostimulation, ultraphonophoresis, etc. Regular physiotherapy is necessary to restore the function of the muscles innervated by the peroneal nerve. peroneus are innervated, regular physical therapy is essential. Orthoses are recommended to correct pes valgus to fix the foot in the correct position.
Surgical treatment is indicated when nerve conduction is completely disrupted, conservative treatment is unsuccessful, or nerve conduction returns. Depending on the clinical situation, neurolysis, decompression of the nerve, suture or plication are possible. For chronic neuropathy, in which the muscles innervated by the oculomotor nerve lose their electrical stimulation, surgery to relocate the tendon is done.
Read more:- Long fibula muscle.
- The long section of the big toe.
- lower leg muscles.
- The long fibula muscle hurts.
- Tibialis posterior muscle.
- fibula.
- How long it takes for the ligaments to heal.
- tibia and fibula.
