PTFS injuries cause similar symptoms to other ligament injuries. In acute partial tears, the ligament is hypoechoic with some intact fibers. In acute full-thickness ruptures, the fibers are discontinuous or absent and are replaced by a heterogeneous hematoma (Figure 17). Tears are recognized as echogenic foci near ligament attachments. Dynamic imaging can help distinguish a partial tear from a full tear.
- Musculoskeletal ultrasound examination: lower limb injuries. Part 2
- Tear of the soleus muscle
- causes of pain
- treatment options
- Endoscopic fibular deepening
- Periarticular tendinopathy on ultrasound examination of the lower limbs
- Subluxation and dislocation of the fibular tendon during ultrasound examination of the lower limbs
- symptoms
- causes
- Why does the fibula nerve become inflamed?
- Treatment of fibula nerve inflammation
- General information.
- Anatomy of the sagittal nerve
- Causes of fibular nerve neuropathy
- Stretching-guru.ru
- Long thigh muscle
- Summary
- More information on this topic
- Leonid Klimov
Musculoskeletal ultrasound examination: lower limb injuries. Part 2
A tear of the medial head of the calf muscle, known as tennis leg, most commonly affects middle-aged athletes who report severe midfoot pain during active ankle flexion and simultaneous knee extension.
When assessing symptoms of a suspected rupture, the physician should consider the alternative diagnosis of deep vein thrombosis, which may also be associated with symptoms.
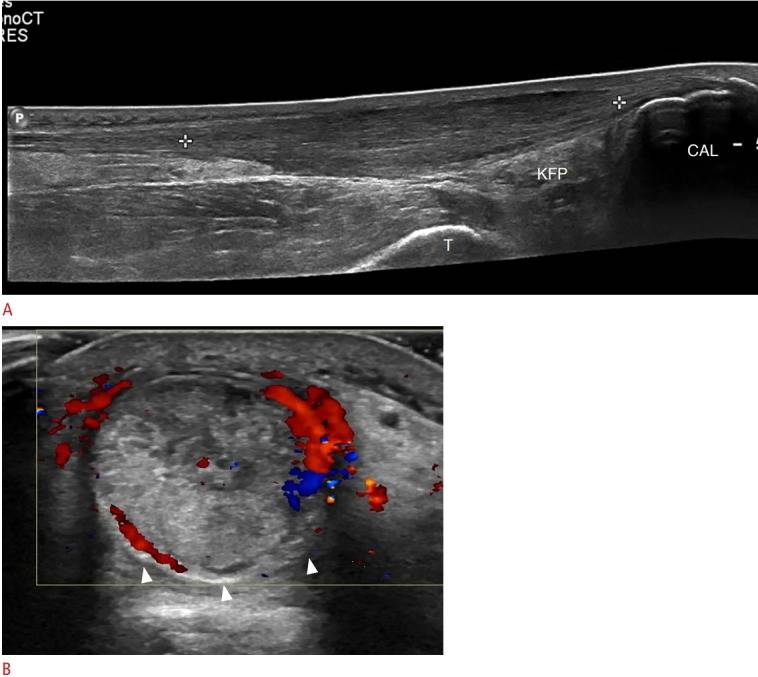
The medial head of the calf muscle is best assessed in the longitudinal plane. Ultrasound features of the tear include disruption of the normal, alternating linear, hyperechoic and hypoechoic appearance of the distal muscle-tendon junction, with hypoechoic hemorrhage replacing the normal conical appearance of the distal aspect (Figure 10).
Large tears are characterized by retraction and heterogeneous fluid extending proximally between the medial head of the calf muscle and the soleus.
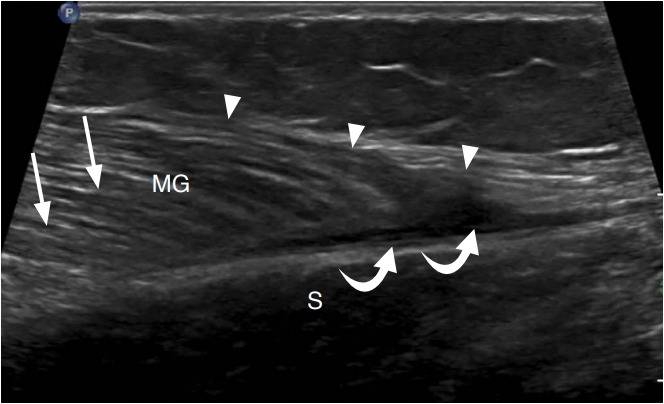
Figure 10. A 30-year-old woman with a tear of the medial head of the calf muscle (tennis leg).
Ultrasound of the long axis of the tibia to the distal medial head of the calf muscle (MG) shows an irregular and hypoechoic distal myoendinous junction (arrowheads) with a small hypoechoic hematoma (curved arrows) between the MG and the camebio-osseous muscle (S). Compare with the normal appearance of the muscle (arrows).
Tear of the soleus muscle
Patients with a rupture of the soleus tendon describe a sudden onset of pain in the calf muscle, which they experience as a shock or direct blow, similar to an injury to the medial head of the calf muscle.
The patellar muscle begins along the posterior superior aspect of the lateral condyle of the thigh and the muscle extends inferiorly and medially along the posterior aspect of the knee. The long and thin longitudinal tendon, located between the longitudinal head and medial head of the calf muscle, terminates either at the calcaneus adjacent to the posteromedial aspect of the Achilles tendon or at the Achilles tendon itself.
Ultrasonography diagnoses a soleus tendon rupture by the absence of a normal soleus tendon with heterogeneous hypoechoic fluid in the form of a hematoma at a suspected site between the soleus muscle and the medial head of the calf muscle (Figure 11).
Figure 11. A 32-year-old woman with a soleus dissection.
Ultrasound examination of the long axis of the tibia to the medial head of the calf muscle (MG) shows a heterogeneous hypoechoic hematoma (arrowheads) accompanying the medial head of the calf muscle and the cambium muscle (S). The soleus tendon was not identified.
The short fibula muscle is responsible for 63 % of the force required to straighten the foot. Together with the long fibula, it is also involved in plantar flexion. [2][3] The oculomotor muscles work together to provide dynamic stabilization of the lateral side of the ankle during loads associated with sudden inversion. [3]
Ankle and foot injuries are common in physical therapy, with injuries to the lateral aspect of the ankle clearly predominating. The most common short fibula injuries involve the tendon and include tendinopathy, dislocation/subluxation, sprain, and dissection. [1] Short fibular tendon injuries are most commonly caused by inversion or supination forces. If the lateral ankle is dislocated, the short fibula muscle can tear and cause swelling of the lateral side of the ankle. [1] In a supination-adduction injury, the short fibular tendon can also be damaged, causing it to pull on the base of the fifth metatarsal, resulting in a burst fracture called a Jones fracture. [1]
When examining a patient for a short calf muscle injury, the general position of the tibial and hindfoot structures should first be assessed. Patients with varus position of the hindfoot have a higher risk of tuberculi muscle injury. To select orthopedic treatment, the flexibility and ability to correct varus should be assessed. [3]
Upon observation, peroneus muscle dysfunction is often evidenced by swelling just behind the fibula and along the lateral surface of the heel bone. Patients typically have pain in the posterolateral region of the ankle that increases with activity and decreases with rest. The tendon may be sensitive when palpated. Range of motion testing may reveal pain with resisted extension, passive extension-extension, or resisted first radius plantar flexion. Active circular movements of the ankle joint can in turn cause tendon subluxation. Specific tests, such as the periosteal muscle compression test, should be performed to assess for pain, grinding, and clicking at the posterior border of the distal fibula during vigorous extension and dorsiflexion of the ankle. [3]
causes of pain
Thigh pain can occur at rest (at night or in the morning after sleeping), while walking or running, with or without exercise; they may be accompanied by bruising, swelling, grinding, clicking, burning, numbness, tightness; sharp, stabbing, pulling, stabbing, dull, burning, expanding, throbbing, holey; affects only the right leg, only the left leg or both legs; upper part near the head of the fibula, lower part near the ankle or along the entire length of the muscle.
Possible causes of pain in the tuberculosus muscle include:
- Injury to the piriformis muscle (peroneus muscle);
- contusion of the fibula;
- spasm of the peroneal muscle;
- myocarditis of the peroneal muscles;
- poststraining syndrome;
- tendinosis or tendonitis;
- Trigger points.
treatment options
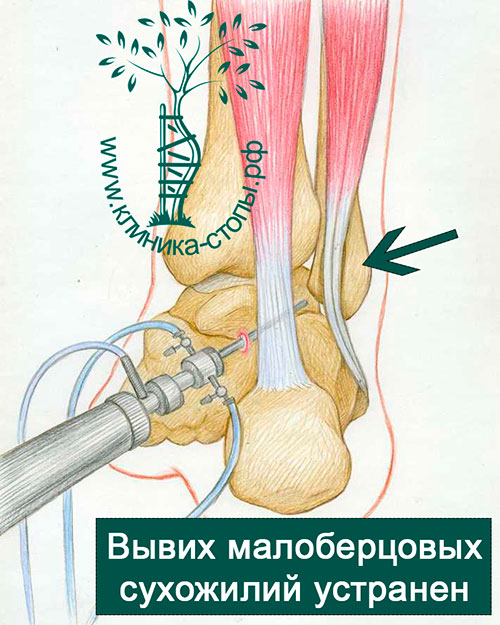
Various studies and our experience show that conservative treatment leads to rather unpredictable results and a high rate of tendon re-dislocations.
Surgical procedures produce excellent results and are therefore considered the mainstay of treatment.
There are several surgical options to stabilize and prevent further tendon subluxations and dislocations, the most effective of which is bone grafting to deepen the tendon groove.
Currently, these operations are performed endoscopically (arthroscopically) through multiple skin punctures.
Open procedures are characterized by a higher risk of calf nerve damage, a painful postoperative scar, and infectious complications. Due to plaster immobilization in the postoperative period, the rehabilitation period may be longer, while endoscopic procedures allow immediate functional healing.
Endoscopic fibular deepening
The operation is performed on an outpatient basis under spinal anesthesia. It begins with two skin incisions of 4 mm each. A special endoscope, called an arthroscope, is used to examine the tendons of the fibula. It transmits the images from the joint to monitors in the operating room. Under direct arthroscopic control, the groove is deepened using a special bone drill connected to a shaver.
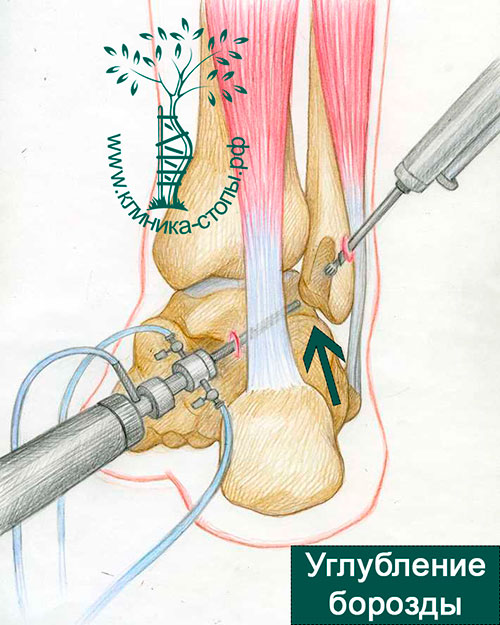
The arthroscopic surgical technique enables stable positioning of the hamstring tendons in the newly created groove and an excellent cosmetic result.
Periarticular tendinopathy on ultrasound examination of the lower limbs
A common cause of posterolateral ankle pain is the hamstring tendon, which is prone to excessive trauma. While the long fibulamus, which arises proximally from the fibula and tibia, has its muscle-tendon junction long before the ankle joint, the short fibulamus, which originates distally from the fibula, tapers distally to the lateral malleolus, where the tendon is located posteriorly in the sulcus retromalleolaris runs. The short fibula muscle normally contacts the fibula between it and the long fibula muscle, which probably explains its propensity for injury at this location. The tendons are held in position behind and distal to the lateral malleolus by an upper and lower holder. Distally, the tendon runs anteriorly on both sides of the bony process of the heel bone, the so-called humeral tubercle, until the short tendon attaches to the base of the fifth metatarsal and the long tendon inserts in an arc along the sole of the foot at the base of the first metatarsal and the middle phalanx .
On ultrasound, peroneal tendinosis appears hypoechoic with possible enlargement of the tendon. An anechoic gap indicates a partial rupture of the tendon. An anechoic gap that extends to the surface of the tendon, usually the short fibula, is called a partial longitudinal tear. A full-thickness tear is a tendon rupture with retraction. Ultrasound-guided tendonitis can range from a rupture with anechoic fluid in the tendon sheath to mixed echogenicity, although hypoechoic tendonitis with increased vascularization predominates.
Subluxation and dislocation of the fibular tendon during ultrasound examination of the lower limbs
Abnormal movements of the fibula muscle tendon can cause clicking, pain, and damage to the tendon. This condition is best assessed with ultrasound during dynamic imaging with flexion and extension of the ankle. The subluxation and dislocation of the fibular tendons is a result of damage to the superior holder that normally holds the tendons along the posterior aspect of the fibula in the retromalleolar groove. When the suspensory apparatus on the uchi of the lower extremity is damaged or torn, it may take the form of a hypoechoic or discontinuous line, with or without a torn fragment on the fibula, which is retracted during movements. During flexion and retraction movements, one or both tendons of the humerus muscle may partially shift forward and sideways from their normal position (subluxation) or completely shift (retraction) and return to rest, which can result in tendonitis and tendon rupture.
A tendon subluxation occurs when the tendons of the rectus muscle and longus muscle of the humerus move abnormally toward each other, causing a snapping sensation while lying lower than the intact upper extremity. This condition may be associated with a longitudinal tear of the short fibula, in which the tendon of the long fibula moves between the two bundles of tendons of the short fibula under stress. Intramedullary subluxation is associated with an abnormally convex posterior border of the anterior ankle and a deep short fibula with the muscle-tendon junction extending distally from the lateral malleolus.
symptoms
Trigger points in the long fibula transmit the pain to the outside of the ankle joint (Fig. 10.13).
The pain is usually concentrated on and under the lateral malleolus (malleolus - Latin malleolus - is the outer bone of the ankle or the protruding end of the fibula). Sometimes the pain is located in the middle third of the shinbone, on the outside and along the outer edge of the foot (not shown). The entire ankle is usually sensitive to pain, whereas if a ligament is torn the sensitivity is localized. Pain and tenderness in the ankle are often mistaken for signs of arthritis.
A common misdiagnosis is trigger point tendinitis in the fibula muscle, which is characterized by weakness of the ankle joint. Additionally, nerve compression by this muscle can cause numbness in the lower leg, ankle, and upper foot. The weakness of the muscle makes it difficult to lift the foot. With nerve compression, weakness may not be accompanied by pain. These symptoms are similar to those of a compressed nerve in the spine due to disc damage.
Before conclusions can be drawn about the spine, the trigger points in the eye muscles must be eliminated, although in some cases both conditions can occur.
causes
Excessive walking, running and climbing are prerequisites for trigger points in the long fibula muscles. Walking is especially bad for these muscles if you have one leg shorter than the other, flat feet, or Morton's foot (more about Morton's foot in the relevant chapter).
Sleeping on your stomach or back with your feet elevated puts your muscles in a shortened state. If you don't care too much about cleanliness, try folding the duvet so that your legs and toes have more room. High-heeled shoes put strain on the muscles in the lower legs, causing shortening and stiffness. In high-heeled shoes, the weight of the body rests on the toes, and the periosteal muscles are in a state of contraction, maintaining balance.
Stockings or therapeutic socks compress muscles and contribute to trigger points. Crossing your legs while sitting puts pressure on the ankle nerves, causing numbness and muscle weakness. The squatting position has the same effect on the nerves and vessels, and in addition leads to pathological tension of many muscles, including the thigh muscle group. Trigger points arise in all cases when a certain unnatural position is held for too long.
Why does the fibula nerve become inflamed?
- Poisonings Through various substances.
- injuries Injuries to the lower leg.
- diabetes – One of the complications of this disease is damage to small vessels and impairment of blood flow to various nerves, including the ankle nerve.
- Vasculitis – An inflammatory process in the vessel wall.
- circulatory disorders Due to continued pressure. Often occurs in people who like to sit with their legs elevated.
- Dysproteinemia – A condition in which the ratio of different types of proteins in the blood is unbalanced.
- tunnel syndrome – Nerve inflammation is caused by compression of the nerve trunk between bones and ligaments. The 'tunnel' in which ankle nerve compression most commonly occurs runs near the head of the fibula.
Have you noticed numbness or problems moving in your leg? See a neurologist – How early you see your doctor can determine the effectiveness of your treatment.
Treatment of fibula nerve inflammation
The principles of treatment are the same as for inflammatory processes in other nerves:
- Preparations with B vitamins – help to improve the functioning of the nervous system.
- Medicines to improve blood circulation in the small vessels.
- Drugs to improve metabolic processes in nervous tissue and the transmission of nerve impulses.
- Physiotherapy.
- Massages.
- therapeutic exercises.
If the inflammation of the nerve is the result of tunnel syndrome, anesthetic solutions and preparations of adrenal hormones (glucocorticoids) are injected into the compression site of the nerve to suppress the inflammation. In severe cases, the doctor may recommend surgery to relieve compression of the nerve trunk.
If the inflammatory process is caused by trauma and treatment is ineffective within 1-2 months, the neurologist will recommend additional examinations and surgical treatment.
The effectiveness of treatment for nerve inflammation depends on how early it is started. You should not delay visiting the doctor for too long. An experienced neurologist awaits you at Medica24 International Medical Center.
The oculomotor nerve is a mixed nerve (it contains both sensory and motor fibers) and, together with the tibial nerve, provides movement and muscle feeling in the lower leg. In the case of an inflammatory process – nerve inflammation – these functions are disrupted. The following characteristic symptoms occur:
Motor disorder. Inability to straighten the foot and toes or externally rotate the foot. The foot is constantly panting and turned slightly inwards. This is referred to by the Latin term pes equinovarus. There is a 'buttercup gait' (step): When stepping, the affected person lifts their foot up so as not to hit the ground with their toes. It is not possible to lift your toes and stand or walk on your heels.
Sensitivity disorder. Decreased sensitivity to touch of the skin and pain on the outside of the lower leg, hind foot.
General information.
Peroneal neuropathy or ankle nerve neuropathy occupies a special position among peripheral mononeuropathies, which also include tibial nerve neuropathy, femoral nerve neuropathy, sciatic nerve neuropathy, etc. Because the oculomotor nerve is composed of thicker nerve fibers with a thicker myelin sheath, it is more susceptible to damage during metabolic disorders and hypoxia. This probably explains the relatively high incidence of sagittal nerve neuropathy. According to some reports, femoral neuropathy occurs in 60 % of trauma patients treated with surgery and splinting or casting. Only 30 % of these patients have neuropathy due to primary nerve damage.
It should also be noted that neurologists often deal with patients who have neuropathy of the fibula nerve, even after surgery or immobilization. This complicates treatment, prolongs it and worsens the results, because the earlier therapy is started, the more effective it is.
Anatomy of the sagittal nerve
The oculomotor nerve (n. Peroneus) branches off from the sciatic nerve at the level of the lower third of the thigh. It is mainly composed of fibers from the LIV-LV and SI-SII spinal nerves. After crossing the popliteal fossa, the ankle nerve exits at the head of the same bone, where its common trunk divides into a deep and a superficial branch. The deep peroneal nerve runs to the front part of the tibia, descends, passes to the back part of the foot and divides into an internal and an external branch. It innervates the muscles responsible for extension (dorsiflexion) of the foot and toes and for pronation (elevation of the outer edge) of the foot.
The superficial peroneal nerve runs along the anterolateral surface of the tibia, where it gives off a motor branch to the peroneal muscles, which are responsible for pronation of the foot while simultaneously flexing the sole of the foot. The superficial branch of the peroneal nerve runs in the medial third of the tibia. The oculomotor runs under the skin and divides into two dorsal cutaneous nerves: the middle and medial. The first innervates the lower third of the tibia, the dorsal surface of the foot and the interdigital spaces III-IV, IV-V. The second is responsible for the sensation of the medial side of the foot, the dorsum of the first toe and the spaces between the toes II-III.
Causes of fibular nerve neuropathy
There are several groups of triggers that can initiate the development of fibular nerve neuropathy: trauma to the nerve, compression of the nerve by the surrounding musculoskeletal structures, vascular disorders leading to ischemia of the nerve, and infectious and toxic lesions. Ankle neuropathy of traumatic origin can be caused by a knee bruise and other knee injuries, a tibial fracture, an isolated fibula fracture, a sprain, a tendon injury or dislocation of the ankle ligament, iatrogenic nerve damage during tibial reduction or knee or ankle surgery.
Compression neuropathy (so-called tunnel syndrome) of the nerve. The peroneal nerve is most often affected at the level of its junction with the head of the fibula - superior tunnel syndrome. It can occur in connection with professional activities, e.g. B. berry pickers, carpenters and others whose work requires long squatting. This neuropathy can also occur after sitting for long periods of time with one foot on the other. When the ankle nerve is compressed where it enters the foot, inferior tunnel syndrome occurs. This can be caused by wearing shoes that are too tight. Compression of the nerve during immobilization is often the cause of compressive peroneal neuropathy. In addition, compression of the peroneal nerve can be secondary to vertebrogenic neuropathy, that is, due to changes in the musculoskeletal system and reflex myofascial disorders caused by diseases and curvatures of the spine (osteochondrosis, scoliosis, spondylarthrosis). Iatrogenic compression-ischemic peroneal neuropathy can occur following compression of the peroneal nerve as a result of malalignment of the leg during various surgical procedures.
The rarer causes of periarticular neuropathy include systemic diseases accompanied by connective tissue proliferation (deforming arthrosis, scleroderma, gout, rheumatoid arthritis, polymyositis), metabolic disorders (dysproteinemia, diabetes mellitus), severe infections, intoxications (including alcoholism, drug addiction) and local Tumor processes.
Stretching-guru.ru
Spinning – for absolutely everyone, at any age and regardless of the level of mobility! However, without preparatory exercises, spinning is not only difficult, but also risky: you can overstretch your muscles and injure yourself.
So here are the best exercises for mastering the longitudinal and transverse twine that will stretch your muscles and joints gently and painlessly.
Long thigh muscle

Latin name Name fibula, rod, shaft; longus, long.
The insertion direction of the tendon of the longus fibularis muscle supports the transverse and lateral longitudinal arch of the foot.
Place of origin: Upper 2/3 of the lateral surface of the fibula. Lateral condyle of the tibia.
attachment point: Lateral side of the medial side of the ischium. Base of the first metatarsal.
Activities: Stretches the foot. Participates in plantar flexion of the ankle.
Unnamed: Superficial oculomotor nerve of L4, 5, S1.
vascular supply: Arteria oculi via posterior tibial artery (from the popliteal artery).
Main functional movement: Example: Walking on an uneven surface.
This article was written on wikipedia
Do you have a question?
If you still have any questions or misunderstandings after reading this article, ask us in the comments below or write to us in the official Facebook group. You will definitely receive an answer as soon as possible.
Summary
As mentioned earlier, this humble muscle group is often forgotten when it comes to the pseudo-tasks of big biceps or powerful buttocks. But the fibulae play a key role in stabilizing the foot and ankle. It would be a mistake to ignore them!
. We would like to remind you that you should consult your doctor or trainer before making any changes to your exercise program.
If you have any questions about the material you have read, you can contact our experts using the contact form or arrange a FREE CONSULTATION. We'll be happy to answer them!
More information on this topic
Exercises for the legs
The common goal of all workouts is health. Training your legs has many benefits and affects the entire body. The leg muscles help the heart ensure good blood circulation.
Exercises for the lower legs
Why it is important to choose calf exercises depending on muscle fiber type and goals. Techniques and exercises for the lower leg muscles.
Exercises for the foot
This article covers the basics of the anatomy and biomechanics of the foot and ankle, prevention of injuries to this area, and exercises for these anatomical structures.
Stretching the legs
Increase your flexibility by performing leg stretches based on how you feel, not how far you can stretch.
Back pain between the shoulder blades, causes
Pain between the shoulder blades is a fairly common problem. People with back pain between their shoulder blades can have different causes for the same symptom.
Manufacturer of sports nutrition in Russia
The list of the best sports nutrition manufacturers today is not very long. It is very difficult to gain consumer trust, as reputation is known to be formed over the years.
Leonid Klimov
Author of the article | Rehabilitation therapist
Read more:- Syndrome of the tibial nerve.
- Long primer.
- The long fibula muscle hurts.
- Tibialis posterior muscle.
- peroneus muscle.
- Innervation of the lower leg muscles.
- Tendon of the tibialis anterior muscle.
- Long flexor muscle.
