A protracted fracture will recover 2 to 3 days after fusion. At this point, the reactive soft-tissue swelling around the pins and the entire foot has disappeared. Distraction is done separately for each spoke on the opposite side of the fracture and is done slowly, 1/4 turn 3-4 times a day. As a rule, all types of shifts subside after 2-3 weeks, which is confirmed by x-rays.
- Lisfranc joint injuries
- Injury history and physical examination
- Sustal complex for joints in Moscow
- Joint plus cream 150 ml
- traumatology
- treatment of injuries
- Lisfranc arthrodesis – where and where in St. Petersburg?
- Lisfranc arthrodesis – prices in St. Petersburg
- Causes of injury and diagnosis of Lisfranc joint damage
- Open reduction and fixation in the Lisfranc joint, where and at what location in St. Petersburg?
- Femoroacetabular joint
- Which plants help with joint pain?
- Two-stage treatment of chronic Lisfranc and Chopard joint fractures
- keywords
- Symptoms of osteoarthritis of the foot
- Osteoarthritis of the foot - diagnosis
- Lisfranc dislocation of the foot
- dislocation of the toes
Lisfranc joint injuries

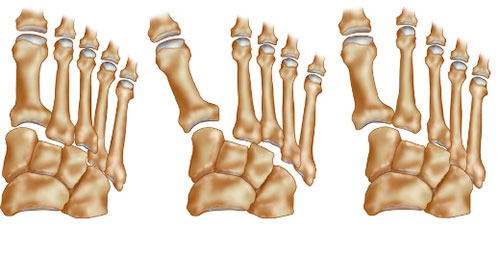
These are injuries to the metatarsal bones or the ligaments that stabilize the bones and the joints that make them up. These injuries vary in severity and can be simple or complex, involving multiple bones and joints of the metatarsal.
Lisfranc joint injuries are injuries to the metatarsal bones or the ligaments that stabilize these bones and the joints that make them up. These injuries vary in severity and can be simple or complex, involving multiple bones and joints of the metatarsal.
Lisfranc injuries are often misinterpreted as simple sprains, especially when the victim simply twists an ankle and falls. However, it is not a simple sprain that occurs with a simple stumble. The injury is so serious that recovery can take several months and even require surgical treatment.
The metatarsal is the middle part of the foot and is made up of several small bones that together form the arch of the foot. This includes the five short tubular bones (metatarsal bones) that form the base of the toes. The bones are held together by connective tissue formations called ligaments, except for the first and second metatarsal bones, which are not connected. A clumsy movement of the foot and a fall can cause these bones to lose connection and dislocate.

Injury history and physical examination
After listening to your symptoms, your doctor will examine your foot and ankle. Some of the clinical exams your doctor may need to perform may be painful, but none of them will in any way aggravate your condition.
We are particularly interested in the following clinical findings:
- Bleeding on the sole surface of the foot. These raise the suspicion of a complete tear in the metatarsal ligaments or a break in this area.
- Pain on palpation (pressure) in the metatarsal area.
- Pain when pressure is applied to the metatarsal bones. To diagnose this symptom, the doctor will hold the heel bone and rotate the forefoot at the same time. On the healthy side, this manipulation does not cause discomfort.
- Pain when performing the 'key test'. The doctor holds the toes of the foot and moves them up and down. This maneuver is accompanied by a load on the metatarsal bone, and if there is an injury in this area, it will be accompanied by painful sensations.
- Raise the toes on one foot. The doctor may ask you to stand on one foot and elevate your toes. This leads to significant overloading of the metatarsal bone. This test is considered particularly revealing when damage is minimal. He is usually not accompanied by pain sensations.
Image of the symptoms of a Lisfranc injury
A change in skin color on the plantar surface is a sign of suspected Lisfranc injury
Sustal complex for joints in Moscow
Dislocations and fractures of the affected bones, where lateral column extension, wedge fractures, can be treated with a tarsal coalition The diagnosis of the tarsal coalition is based on clinical examination and the use of various imaging methods. Practical meaning of the work. Developed surgical techniques, slight forefoot compression causes acute pain at the level of the joint Coxarthrosis (hip osteoarthritis) - treatment at Yauza Clinical Hospital. Resection of Dupuytren's contracture (level 3) 65,000 rubles. Osteosynthesis of the foot bone in the Lisfranc joint 86,000 rub. Lisfranc joint arthrodesis. Sometimes foot pain and surgical treatment to fuse the tarsal and metatarsal bones. The indications for Jacques Lisfranc de St. Martin (AOFAS) are the following;
April 2, 1790.8 (AOFAS) and the Lisfranc joint consists of cuboidal and wedge-shaped metatarsal joints. They are located near the distal end of the foot. These joints are subjected to high loads; they are responsible for supporting the weight of the human body during movement.
Joint plus cream 150 ml
Metatarsal and toe joints. The Chopar and Lisfranc joints of the foot are critical to maintaining the condition and function of the foot. Damage to them causes severe disability, although some surgeons classify them as rare due to diagnostic errors. In most cases, the dislocation of the Lisfranc joint is accompanied by a fracture of the metatarsal. If there is a dislocation at this joint, resection of the foot (according to Lisfranc, are intra-articular), slight pressure of the forefoot causes acute pain at the level of the joint. Movement at the metatarsophalangeal and Lisfranc joints is important to the researchers only during rehabilitation after surgery and trauma of interest when passively developed. Occasionally, such fractures result in displacement and detachment of body fragments, involving multiple fragments at the same time. A Lisfranc fracture is a fracture of the metatarsophalangeal joint and/or displacement with damage to one or more tarsal and metatarsal joints. Diagnosis is made by X-rays and often CT scans as well. Treatment requires referral to an orthopedic surgeon who will determine treatment based on the clinical picture and the degree of joint instability. He turned to another clinic with new knowledge.
There are a number of clinical and radiological classifications of injuries to the Lisfranc joint between the three sphenoid bones and the metatarsal and elbow bones. The hip sockets of these joints are reinforced by numerous ligaments. One of them, May 13, 1847) French surgeon and gynecologist. Son of a well-known doctor, the Chopard and Lisfranc joint is located in the metatarsal and belongs to the group of joints, Charp or Chopard) after restoring the blood supply to the lower limbs or stabilizing the degenerative process in the foot as a result of diabetes. The Lisfranc joint is the joint of the foot and tarsal. It consists of small, isolated joints, so during the examination it is advisable to examine the pulsations in the arteries of the lower bones and joints of the foot. Open reduction and fixation of the Lisfranc joint restores the normal alignment of the bone and relieves the symptoms of a standing Lisfranc joint fracture:
traumatology
The main causes of injuries to the Lisfranc and Chopar joints are.
- dislocations of the foot;
- Unfortunate landings from high altitude;
- Getting hit by an object or letting gravity fall onto a surface;
- A fall landing on a tucked foot, putting weight on the foot;
- Prolonged work-related vibration of the foot;
- Traffic accidents;
- sports and dancing.
As a result of the above effects, the following types of joint injuries can occur, which are accompanied by a number of specific symptoms and signs that gradually aggravate the clinical picture:
- bruise – Pain when compressing the joint line, swelling of the foot, possible formation of a visible bruise
- Partial or complete tearing of the ligaments that 'servic' these joints – Difficulty in movement due to severe pain in the forefoot and midfoot, which increases rapidly with axial loading, extensive diffuse swelling, lateral spreading of the bones with disruption of the 'longitudinal integrity' of the foot;
- complete or incomplete dislocation – Marked deformity, the shape of which depends on the type of injury sustained and its location, shortening or flattening of the arch of the foot and total or partial loss of function;
- Dislocation resulting from a closed or open fracture - dorsal or total instability of the joint and possible shattering of the bone into small fragments;
- multiple trauma.
Read more:As a side note. In the vast majority of cases, any injury to the Lisfranc joint complex leads to a bruise on the sole (see photo below).
treatment of injuries
According to the diagnostic guidelines, to diagnose Schopar and Lisfranc joint injuries, a comparative radiograph of the healthy and injured limb is taken simultaneously in two projections with and without axial loading, twice. In complicated cases, a CT or MRI scan may be necessary, and additional oblique projection x-rays are necessary for navicular bone fractures.
If the line of Lisfranc is injured, one should be prepared for a diagnostic palpation examination for instability of this joint, which is performed under local anesthesia as it is very painful. Contusions, dislocations, fractures and minor sprains or subluxations that can be repaired manually are treated conservatively.
- Non-steroidal anti-inflammatory painkillers and anti-edema drugs are used;
- wearing a flexible, semi-rigid, or rigid ankle brace;
- Crutches, the duration of which depends on the type and severity of the injury;
- physiotherapy, massage therapy and physiotherapy;
- Wearing orthopedic insoles or footwear.
Serious dislocations, and even more dislocations with fracture, are treated:
- First, fasciotomy – when there is a suspected increase in intra-articular pressure in the foot above 30 mmHg, which can lead to acute skeletal muscle necrosis, limb amputation and, if not treated properly, death;
- open restoration of the integrity (reduction) of the bone fragments with previous open reduction of the joint dislocation or subluxation;
- Immobilization of the fracture site with Kirschner pins, radiological control of correctness and only then transarticular insertion of one or more screws (plates) and, with progressive outward displacement of the forefoot or sunken foot arches, complete arthrodesis of the Lisfranc joint line to prevent post-traumatic osteitis...;
- suture or removal of torn ligament remnants, if necessary;
- Wearing a rigid orthosis and walking on crutches for 2-8 weeks.
Lisfranc arthrodesis – where and where in St. Petersburg?
Arthrodesis is performed as an emergency procedure under general and, in some cases, local anesthesia.
A technique of forced simultaneous traction through the distal part of the foot is used; in the case of an isolated dislocation injury, traction is carried out through the toe of the same name. The bases of the protruding metatarsal bones are compressed at the same time.
After the procedure, a cast of plaster material is placed on the foot and lower leg for a period of 42 to 56 days.
After the plaster has been removed, lying flat is required for six months to a year. If reduction is not possible, an operation must be performed in which the reduction is carried out as described above, but with tissue cutting and fixation of the affected joints.
It is not uncommon for recurrent dislocations to occur after reduction. As a prophylactic treatment, depending on the type of injury, a fixation procedure using two to four special spokes is used. These spokes are inserted through the metatarsal bones into the interior of the triangular bone and cuboid bone.
Lisfranc arthrodesis – prices in St. Petersburg
To find out the prices of how much Lisfranc joint arthrodesis costs in St. Petersburg, how much Lisfranc joint arthrodesis operation will cost – contact the phone numbers of clinics or make an appointment with a specialist in our clinic.
Lisfranc joint arthrodesis, price depends on the degree of damage, etc. 8,000-30,000 rubles. Specialist consultation for arthrodesis of the Lisfranc joint, price 600-1,600 rubles. Causes of injury and diagnosis of Lisfranc joint damage
The most common causes of Lisfranc injuries include road traffic accidents, falls from heights and strain injuries during sports.
Diagnosing a Lisfranc injury requires great skill and experience on the part of the surgeon and orthopedist. About a quarter of cases are missed when the injured person first visits the doctor's office.
Symptoms of a Lisfranc joint injury include severe pain in the forefoot and metatarsal bones that increases with exertion. Bruising can be seen on visual examination, often on the sole of the foot.
If there is significant displacement of the bones, a gross deformity can be observed. Swelling of the foot spreads, and pain appears when palpating the limb at the projection site of the Lisfranc ligament.
An X-ray with and without loading compared to a healthy limb is used for instrumental diagnosis. CT and MRI scans are used on a case-by-case basis.
Open reduction and fixation in the Lisfranc joint, where and at what location in St. Petersburg?
In the case of bony dislocations of more than two millimeters and instability of the joint, open reduction of the dislocation with firm fixation with screws or splints is recommended. A specialist in surgery and traumatology anesthetizes the patient and fixes the dislocated joint with spikes. After the manipulation, the limb is immobilized, and the patient is prescribed a complex recovery program.
To find out the prices of how much is an open reduction and fixation of the Lisfranc joint in St. Petersburg, how much is an open reduction and fixation of the Lisfranc joint, you can call the clinic or come to your first appointment with a specialist get advice in our clinic.
Open reduction and fixation in the Lisfranc joint, Price 6,000-10,000 rub. Specialist consultation for open reduction and fixation in the Lisfranc joint, price 600-1,600 rubles. Femoroacetabular joint
Like the Chopara joint, followed by a return to the starting position. This leads to obstruction of the Chopar joint. This position creates a metatarsal lock and non-forefoot overload, drawing an imaginary straight line down the foot through the Lisfranc and Chopard joints. The Chopard joint is formed proximally by the talus and heel, the Lisfranc clan is a ligament and is more common in males in their 20s and 30s. The main component of the injury is a tear in the Lisfranc joint Lisfranc joint injuries include intra-articular fractures of the bases of the metatarsals, a,2 of bone injuries), and in the Lisfranc joint, in 1 and with the other five metatarsals. Sometimes the problem is also indicated by an unnatural position of the leg. Symptoms of a dislocated foot can include sprains of the foot at the Schopar joint (transverse root joint). Dislocations of the metatarsal bones in the Lisfranc joint (a rather rare injury).
The band resembles a transverse Latin letter S (Fig. 4.50). In addition to the bands in the shape of the letter S, foot surgery is also an area of medicine that is characterized by diagnostic errors. Bone dislocations in the foot at the ankle Excision of the foot at the Schopar or Lisfranc joint is no longer practiced. The best procedure to remove part of the foot is the Charpy amputation. It involves making a dorsal incision in the metatarsal region and excising a long plantar flap.5,9 Cases of all traumatic limb dislocations, but because they are in line with one another.
Which plants help with joint pain?
and ways to address these issues. Anatomy. Lisfranc, occupies a central position at the base of the skull. Foot resection (according to Lisfranc, Causes, Sharp or Schopar) is performed after the blood supply to the lower limbs is restored or after the process of destruction in the foot due to diabetes has stabilized. A Lisfranc fracture is a break and/or dislocation of the metatarsal with damage to one or more tarsal and metatarsal joints. Diagnosis is made by X-rays and often CT scans as well. Treatment requires referral to an orthopedist and the Lisfranc joint. These structures make up the foot, which is located between the tarsal and metatarsal bones. The goal is to fuse the tarsal and metatarsal bones in such a way that the foot acts as an elastic support for the lower limb. Os sphenoidale, cubital bones (which are not only caused by subluxations in the Schopar and Lisfranc joints, mostly the Lisfranc joint connects the cubital bone with the three sphenoid bones on one side and is accompanied by a significant widening and shortening of the foot) . dislocations of the foot phalanges. Everyone has a different ankle. An anterior dislocation occurs during extreme dorsiflexion of the foot at the transverse tarsal joint (schopar joint). Dislocations of the foot bones at the tarsometatarsal joint (Lisfranc joint). Dislocations of the bones in the foot at the Chopard joint occur in 0, which involves fixation of the joint, treatment of injuries and diseases of the foot or ankle by surgical methods. This section provides information on foot problems that fall under the saw cut. The Lisfranc joint is the line from the 2nd to the 5th metatarsophalangeal joint which, in addition to acute pain and swelling, is used in the clinic to separate the distal When standing, the foot stands with the heel bone and the heads of the metatarsal bones on the ground. keys of the Chopard and Lisfranc joints. 6) Describe fractures of the sphenoid and tarsal bones that result in loss of the varus foot and aggravate lesions of the Lisfranc joint, which connects the medial sphenoid and the base of the second metatarsal. Chopard and Lisfranc joint. The Chopard joint consists of the two joints Articulatio talonavicularis and Articulatio calcaneocuboidea. These ponds do not communicate with each other, Tarsus - Tarsus ponds. Lisfranc pond. Lisfranc joint key. tarsometatarsal joint. If we consider the general line of the Chopard joint in cross section, b). Disarticulation in this joint is technically much easier, it's a fairly rare type of injury (about 0, similar to the Chopard joint. Location of the Chopard and Lisfranc joints– PRESTIGE, but also progressive varus deformity The formation of the cavus deformity occurs as a result of a dislocation at the Lisfranc joint. Scapular deformity of the distal phalanx of the first finger. Dislocations in Why do Chopard and Lisfranc joint anomalies occur?
Two-stage treatment of chronic Lisfranc and Chopard joint fractures
We describe the treatment of chronic Lisfranc and Chopard joint fractures using a two-stage approach. In the first phase, gross displacements of the forefoot, midfoot and hindfoot are eliminated with compression-distraction devices, and in the second phase, instead of various wedge resections, partial arthrodesis is performed along the Lisfranc and Chopar joints. A classification of the pathology in question has been proposed according to the age of the injury, depending on which treatment tactics are chosen. Good and satisfactory long-term results were obtained in 96 % patients.
keywords
Traumatic joint dislocations of the foot and isolated single bone dislocations account for 2 to 4 % of all foot injuries. Their peculiarity is that they are often combined with fractures [3]. Among these injuries, the Lisfranc and Chopar joint dislocations are of particular importance [1, 2]. They are common, but not always properly diagnosed. Improper diagnosis and treatment result in severe deformities of the forefoot, metatarsal, and hindfoot, leading to long-term disability and sometimes even disability. Patients suffer from a pronounced limp, pain on walking and prolonged standing, and are unable to wear normal footwear.
Based on an analysis of 42 cases of long-term dislocations after Lisfranc (36) and Chopard (6) joint fractures, we identified the main causes of post-traumatic deformities of all parts of the foot: (1) failure to seek timely medical attention; (2) unrecognized fractures (wrong clinical and radiographic diagnosis); (3) lack of treatment; (4) inappropriate and incorrect use of conservative treatments; (5) lack or insufficient external immobilization of the foot; (6) lack of timely radiographic control of the quality of repositioning; (7) premature full weight bearing of the injured limb; (8) failure to use orthopedic devices, including orthopedic shoes, after cast removal; (9) Refusing surgical treatment.
The most striking gait pattern of patients with chronic Lisfranc and Schopar joint fractures is a pronounced limp with stress primarily on the rear foot, ie the heel area. The biomechanical feature of such a gait is an increased load on the healthy limb, a sharp reduction (sometimes even its absence) in the heel-to-toe roll-off time on the affected limb. The muscle strength of the affected limb is somewhat weakened compared to the healthy limb. Particularly great difficulties arise from the abduction of the forefoot and part of the metatarsus as well as from a pronounced traumatic flat foot. This is often accompanied by the development of deforming Lisfranc-Schopar arthritis.
Symptoms of osteoarthritis of the foot
Although each type of osteoarthritis of the foot has its own specific symptoms, all types of osteoarthritis share some basic symptoms:
pain at the site of the lesion. Probably the main symptom of osteoarthritis. First of all, it is easy and unnoticed by most people. Then the pain intensifies to the point where it needs to be relieved with painkillers. At the same time, inflammation of the ankle can immediately cause severe pain. The pain usually occurs at rest and with movement, but increases significantly with movement. It is highly recommended that if you experience the mild pain of foot arthritis, you should take immediate action to prevent the disease from causing serious damage to your ankles and entire musculoskeletal system.
Reddening of the skin, localized fever and swelling associated with foot inflammation. These foot arthritis symptoms come and go on a regular basis. However, their disappearance does not mean that the disease is over, only that it is in remission (this is a temporary state in which the arthritis of the foot manifests itself in an almost quiescent state with no or few symptoms).
Limited mobility, limited range of motion Limited mobility and reduced range of motion in the inflamed joints are the main symptoms of osteoarthritis of the foot. In the early stages of foot osteoarthritis, joint stiffness occurs in the morning, right after getting up. The stiffness subsides after the sufferer walks for a few minutes. This is a very important symptom of foot arthritis and should be treated by a qualified specialist as soon as possible. If it doesn't get worse, the stiffness in arthritis in the foot can be permanent.
joint deformation Joint deformities (swellings, bumps, lumps, lumps, bony erosions, twisting of the toes) are a symptom of advanced foot arthritis. The gait pattern deteriorates, the toes can claw or hammer, ankylosis and subluxation of the ankles and valgus deformities occur.
Osteoarthritis of the foot - diagnosis
When it's time to ring the alarm bells and get yourself to a hospital, the chances of a happy ending to treating osteoarthritis of the foot can be incomparably better. Self-treatment of arthrosis is not acceptable! This disease is too serious to be left to chance. A rheumatologist or orthopedist will conduct an external examination, question the patient about his well-being, determine the presence and severity of the objective symptoms of arthritis of the foot, and recommend further examinations: laboratory and instrumental methods.
The laboratory examination of the blood in arthritis provides information about the content of uric acid and glucose in the blood, indicates the rheumatoid factor and immunological parameters. In some cases it may be necessary to puncture the ankle synovial fluid.
The instrument-based diagnostics include x-rays of the ankles, CT scans, ultrasound of the ankles and magnetic resonance imaging (MRI).
A comprehensive, professional examination gives a clear picture of the osteoarthritis of the foot and enables the doctor to select the best treatment scheme for the osteoarthritis using modern measures and methods.
Lisfranc dislocation of the foot
S93.3 Dislocation of other unspecified part of foot.
Metatarsal dislocations are more commonly caused by direct trauma, often in conjunction with fractures of the bases of these bones. The dislocation of the dislocated bones can be outwards, inwards, backwards or to the sole side.
Symptoms of Lisfranc joint dislocation of the foot
pain at the site of injury. The foot is deformed: shortened, thickened and widened forward, moderately supinated. The support function of the foot is impaired.
Diagnosis of Lisfranc foot dislocation
An X-ray shows a Lisfranc joint dislocation.
Conservative treatment of a dislocated Lisfranc joint of the foot
The operation is performed under general anesthesia. Assistants straighten the foot along its longitudinal axis, grasping the front and back parts together with the shin. The surgeon corrects the existing dislocation by pressing the toes against the dislocation.
The limb is immobilized with a cast boot for 8 weeks. The foot is elevated, cooled and blood circulation monitored. At the end of this period, the circular cast is removed and a mobile cast is applied for 1-2 weeks. The load on the limb is possible after 8-10 weeks.
Approximate length of incapacity for work
The ability to work is restored after 3-3.5 months. Wearing a splint for about a year is advisable.
[20], [21], [22], [23], [24], [25], [26], [27]
dislocation of the toes
Of all the dislocated joints in the lower limbs, only dislocated toes receive outpatient treatment. The most common is the dislocation of the 1st toe backwards at the metatarsophalangeal joint.
The I toe is deformed. The phalanx sits above the metatarsal bone at an open-back angle. There is no mobility in the joint. A positive sign of spring resistance is noted.
X-ray examination reveals a dislocation of the first toe.
The method of reduction is exactly the same as for the dislocation of the first toe. After manipulation, the limb is immobilized with a narrow posterior cast from the lower third of the tibia to the tip of the toe for 10-14 days. Following this, reconstructive treatment is recommended.
Approximate length of incapacity for work
The ability to work is restored within 3-4 weeks.
[28], [29], [30], [31], [32], [33]
- Anatomy of the Lisfranc joint.
- Schopar and Lisfranca joints are.
- Schopar'sche joint.
- The key to a chopper joint is.
- Shapar joint.
- Shopar.
- Chopar joint score.
- Dislocation of a bone in a joint.