In compensated or subcompensated cases, conservative treatment is carried out. The main antimicrobial agent is selected depending on the identified infectious agent. Therapy of bacterial tonsillitis is based on the use of penicillins, macrolides and cephalosporins. If it is a viral disease, antiviral drugs are prescribed. In case of secondary infection, antibiotic therapy is additionally carried out. If the infection was caused by fungi, antifungal drugs are used.

- How Anesthesia and Narcosis Work: Myths, Concerns, Side Effects
- duration of rehabilitation
- General principles of rehabilitation
- Method for diagnosing sprains
- What can a trauma surgeon do?
- treatment and rehabilitation
- Symptoms of knee instability
- Osteoarthritis and instability of the knee joint
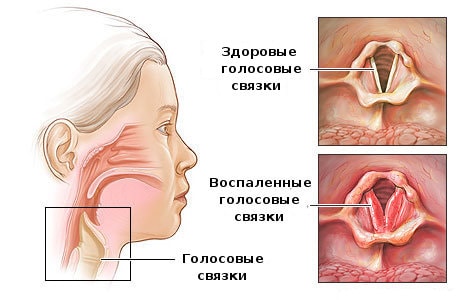
- Causes of laryngitis
- Acute laryngitis
- Chronic laryngitis
- Laryngitis in children
- Advantages of the treatment blocks.
- Types of therapeutic and diagnostic blocks
- topical
- Segmental
- vertebral
- spinal blocks
- surgical treatment
- complications
How Anesthesia and Narcosis Work: Myths, Concerns, Side Effects
No, these are two different things. Anesthesia is a condition in which the patient is put by doctors. The aim is to make the patient unconscious, ie fall asleep, so that the skeletal muscles relax and anesthesia occurs.
Anesthesia is a part of anesthesia in which the patient loses his ability to feel pain. And depending on what ingredients are used, the process can vary. For example, opiate analgesics - the well-known morphine - act on the corresponding receptors in the body and block the pain response. Local anesthetics such as B. lidocaine, reversibly block the conduction of the nerve in the vicinity of which they are injected.
What types of anesthesia are there?
One of the most common forms of anesthesia is intravenous anesthesia. It is usually used for short-term operations (no longer than half an hour). A number of substances are administered intravenously to the patient, e.g. B. Hypnotics (to induce drowsiness). These can be combined with painkillers, often using narcotic painkillers, which on the one hand numb and on the other increase the sedating effect.

Endotracheal anesthesia is usually used for longer operations. The anesthetics are in gaseous form and are injected into the body through a special tube. The drug travels through the lungs to the blood and from there to the central nervous system, which induces sleep. One of the oldest and still most commonly used gaseous anesthetics is nitrous oxide (laughing gas). It is usually supplied to the device from special bottles. The advantage of this type of anesthesia is that it is fully controllable and relatively safe; the person is completely relaxed, which allows the surgeon to perform all complex procedures.
The modern gas anesthetics are volatile liquids. In the anesthesia machine, they are poured into a vaporizer, a special device that delivers the drug to the patient in doses. This process is controlled by the anesthetist. Depending on the operation, doctors may also use a combination of the two agents.
An alternative to spinal anesthesia can be epidural anesthesia, in which a local anesthetic is injected into the epidural space of the spine through a special catheter. Depending on the type of procedure (thoracic or abdominal cavity), the anesthetist will determine where the drug will be administered. In addition to administering the local anesthetic, the anesthetist may also administer an opioid analgesic to enhance the effect of the anesthetic in the epidural space. Sometimes, at the patient's request, the epidural catheter can remain in anesthesia for a period of time (called extended epidural anaesthesia).
More complex and major interventions always require lengthy preparation by the anesthetist - placing a central venous catheter, administering infusion therapy, correcting blood coagulation and other important parameters. It is also important to know if the procedure is emergency or elective.
Can you tell me more about the difference between spinal anesthesia and epidural anesthesia?
In spinal anesthesia, the drug is injected into the subarachnoid space (the cerebrospinal fluid-filled cavity between the soft membrane of the spinal cord and the arachnoid) in the lumbar region. This is usually limited to a few injections. This numbs the soft tissues over the injection site and injects the drug just under the dura. This anesthesia lasts between two and six hours and is technically easier to manage.
In epidural anesthesia, the drug is injected into the space between the dura and periosteum of the vertebra, which contains connective tissue and venous plexuses. This space is closer to the skin than the spinal cord. Anesthesia is performed at any level of the spine. It is considered a technically more difficult manipulation.
I've read that epidural anesthesia can cause paralysis.
It's a common fear, but anesthesiologists assure me it's virtually impossible today. Such a complication can occur postoperatively due to improper care of the catheter, which leads to purulent epididymitis, which causes neurological symptoms with loss of function in the lower limbs. Or by improper actions of the anesthetist when epidural anesthesia is performed high up (there is a risk of accidental injury to the spinal cord). In most cases, however, epidural anesthesia is only associated with headaches, which appear a few days after the procedure.
duration of rehabilitation
'There is an effective and inexpensive remedy for joint pain. ' .
The length of the rehabilitation period depends on the type of injury. Ligaments are bands of connective tissue that connect bones together and serve to strengthen the joint and guide or limit movement in the knee. If they are partially torn, conservative treatment methods are used, while if they are completely detached from the bone base, surgical treatment is used. Sometimes a piece of bone tears off along with the ligament, which greatly complicates treatment and requires a long rehabilitation period.
For minor injuries, a plaster cast is applied for about 20 days, while the knee of older people is often immobilized with orthoses.
Rehabilitation lasts from 1.5 to 3 months, depending on the characteristics of the body. The age of the person also plays a role:
- In young people, the regenerative processes in the joints are much faster, they receive enough nutrients for all biochemical reactions;
- The ligaments of older patients regenerate more slowly because the production of collagen, the building block of all connective tissue structures, decreases with age.
When the ligaments detach completely from the bone, patients are eligible for plastic or surgical repair. In this case, the rehabilitation period is between 4 and 6 months.
Ligament reconstruction in the knee.
If there are no contraindications, patients are referred to a physiotherapist who, after immobilization, subjects them to physical therapy. The physical therapist will develop a series of exercises to build a strong muscular corset. This ensures that there is no unnecessary stress on the knee and that the ligaments can heal properly. The condition of the skeletal muscles is crucial for the function of the joint. When weakened, the entire burden of movement falls on the knee, leading to rapid destruction of the cartilage on the bone heads. Immobilization prevents muscles from contracting for a long period of time, which can lead to atrophy and the development of post-traumatic osteoarthritis of the knee. Rehabilitation doctors point out that 2 weeks is sufficient for the loss of muscle volume.
General principles of rehabilitation
Pharmacological drugs (NSAIDs, muscle relaxants, glucocorticosteroids) eliminate the symptoms of inflammation, so their use quickly becomes redundant. However, the following medications should be taken throughout the rehabilitation period:
- Balanced vitamin and micronutrient complexes - Vitrum, Centrum, Selmevit, Multitabs, Complivit. The B vitamins, the trace elements copper, sulfur, iron, molybdenum, calcium and phosphorus are essential for quickly restoring the integrity of torn ligaments. Fish oil, rich in polyunsaturated fatty acids (omega-3, omega-6) and fat-soluble vitamins, should be included in the treatment regimen;
- Chondroprotectors – Teraflex, Structum, Chondroxide, Arthra, Chondroitin-Acos. The only group of drugs whose active ingredients repair damaged cartilage, bones and connective tissue. After a week of use, chondroprotectors begin to have an anti-inflammatory, analgesic effect;
- Ointments with a warming effect – Skipidarnaya, Apisartron, Viprosal. Used in the first 2-3 weeks of rehabilitation to improve microcirculation, regeneration of small blood vessels damaged during injury.
As soon as the inflammatory process subsides, the patient can be treated with physiotherapeutic treatments. These include UHF therapy, laser therapy, magnetic therapy, electrophoresis with calcium solutions, anesthetics and analgesics. Although various physical agents (electrical impulses, heat, magnetic fields) act on the knee joint, the aim of all treatment measures is to improve blood circulation. The excretion of end and intermediate products of the inflammatory process is normalized, and the lack of nutrients and bioactive substances is eliminated. The regeneration of the ligaments is significantly accelerated and the likelihood of scarred connective tissue structures is reduced.
Method for diagnosing sprains
Already on the basis of the above symptoms, a qualified traumatologist can diagnose a sprain. However, the diagnosis cannot be limited to an objective examination of the leg:
- To exclude the risk of a fracture or fracture, an X-ray examination of the leg is mandatory;
- An ultrasound scan of the damaged joint may be necessary to determine the extent of the dislocation;
- Sometimes an MRI scan is done (if treatment of the leg has been delayed and pain persists, the ligaments should be checked for torn nerve fibers).
There are 3 degrees of severity of the dislocation. At grade one, the main symptom is pain, there may be no bruising, swelling, or other signs. Grade two is characterized by restricted movement and visible signs of ligament strain. Grade three does not preclude invasive surgery (if there is a fracture or chipped bone).
What can a trauma surgeon do?

In the case of a sprain, treatment is usually limited to conservative methods.
At stage I, the pain in the leg should be treated. Immediate relief is important at this stage - the injured leg should be kept still, elevated across the body and the ligaments treated with some coolness.
- Stage II is bed rest, minimal physical exertion on the leg, and possibly the use of painkillers and anti-inflammatory drugs. A bandage or splint (toe) may be needed.
- Stage III - Supporting the damaged tape. In the first days after a sprain, these methods are not allowed to be used, but after 4-5 days, foot massage, physiotherapy, relaxation therapy, aquatherapy and LoF are possible.
Sprains take a long time to heal – up to 3-5 weeks. With persistent pain in the leg, injections with NSAIDs and narcotics are possible. Practice shows that sprained ligaments of the big toe and hip joint are the most painful. The ligaments in the knee take the longest to heal. With them, it is important to prevent the progression of the inflammation of the connective tissue in the leg.
treatment and rehabilitation
Injuries to the knee joint are treated conservatively:
- Immobilization of the injured knee;
- symptomatic drug therapy to reduce inflammation and pain;
- rest for 6-8 weeks;
- Physiotherapy to regenerate the tissue and to stimulate the necessary metabolic processes.
After the doctor's opinion, the patient is prescribed massage, therapeutic exercises and other treatments that do not involve the risk of damaging the reconstructed knee.
If the diagnosis reveals a fracture of the kneecap with a complex displacement, a complete rupture of the meniscus and ligaments, as well as a blockage of the joint capsule, surgical intervention with a longer and more complicated rehabilitation path is required.
Knees recover very slowly, and any mistake in the rehabilitation process can have serious consequences. The most important thing is not to put any weight on the injured leg for at least two months. When moving around, it's best to use a cane or walker to avoid putting unnecessary strain on the injured leg.
You should only start training after consulting your doctor. Any exercise that puts weight on the injured leg should be avoided for several months. If all the rules are followed, full recovery can be achieved within 6-9 months. With a sports injury in the knee area, it is important to get a professional diagnosis as soon as possible, so that there are no chronic processes in the knee joint and timely treatment.
Schedule an appointment
Make an appointment and visit our clinic for a professional examination
Symptoms of knee instability

You can recognize the following symptoms of knee instability
- A feeling of looseness in the knee when you move it.
- The feeling that something is 'sticking' and 'blocking' in the knee joint.
- The knee looks swollen and swollen; this is a permanent condition.
- Knee deformity: valgus (X foot) or varus (O foot).
Osteoarthritis and instability of the knee joint
In 2017, Japanese researchers put forward a very interesting hypothesis that the instability of the knee joint could be the cause of osteoarthritis. According to this hypothesis, osteoarthritis is the result of 'wearing' of the knee joint that develops from the accumulation of abnormal stresses during abnormal movements. This leads to the formation of osteophytes and wear and tear of the cartilage in the knee joint.
The researchers asked themselves: Why does the knee lose stability at all? As we age, there is a breakdown of bone and cartilage, including in the condyles of the knee joint—the bony formations that limit excessive extension and flexion of the knee. Hypermobility of the joint develops with degeneration of the condyles, as does degeneration of the meniscus. However, the cartilaginous covering of the meniscus has a cushioning function. When this damping is reduced, the articular cartilage covering the articular surfaces begins to break down.
All of this means that timely treatment of knee instability can be an effective way to prevent osteoarthritis from progressing. Stabilizing the knee decreases the release of pro-inflammatory cytokines that cause chronic inflammation. Overall, reducing knee instability also reduces aggressive cartilage wear.
- The instability of the knee increases the risk of injury significantly. Therefore, at the first sign of this disease, it is important to consult a doctor. First, the extent of the problem and possible causes must be determined. Second, the doctor can help you choose exercises to stabilize the knee joint.
- Doctors emphasize that the stability of the knee joint is provided by the coordinated work of all ligaments and muscles. This means that surgically removing the meniscus does not make the joint more stable, so surgical treatment is an extreme option.
Causes of laryngitis
Acute laryngitis
In most cases, acute laryngitis is due to a viral infection. It therefore rarely occurs in isolation. Inflammation of the larynx is usually accompanied by a cold (catarrh) and inflammation of the throat (pharyngitis). This is where the infection develops, which then spreads to the larynx. Laryngitis can be caused by SARS, the influenza virus, and more serious diseases like measles.
Factors that contribute to acute laryngitis include:
- Cold - both general and local (ie, cold in the throat);
- Smoking;
- alcohol abuse;
- Excessive strain on the vocal cords;
- Excessive contact with spicy foods.
Acute laryngitis can lead to deterioration in general condition, headache and often fever. The cough is dry at the beginning of the disease and then turns into a wet cough with mucous sputum. Sometimes breathing difficulties can occur because the opening of the larynx narrows due to the swelling of the mucous membrane.
Influenza-related laryngitis can cause bleeding in the lining of the larynx. This form of the disease is called hemorrhagic laryngitis.
Chronic laryngitis

Chronic laryngitis can occur as a complication of the acute form. If symptoms persist for more than two weeks, this indicates that laryngitis has become chronic.
However, chronic laryngitis often develops as an independent disease. Chronic laryngitis can be caused by:
- Regular inhalation of irritants - allergens, chemical vapors, smoke, dust (especially if for some reason nasal breathing is impaired and you have to breathe through your mouth);
- Prolonged strain on the vocal cords (this is common in professions such as speakers, teachers, singers, etc.).
- Intestinal contents are pushed into the esophagus, where stomach acid begins to digest the esophageal lining;
- Bacterial and fungal infections. Infections in particular can enter the larynx not only from above, but also from below - from the lungs if there is a focus of inflammation there. Laryngitis can therefore be a complication of chronic bronchitis or pneumonia.
Laryngitis in children
Laryngitis in young children is a dangerous disease. Severe inflammation can quickly lead to swelling of the larynx. Children with a history of allergies may be particularly susceptible. Breathing becomes difficult, wheezing and barking cough.
In severe cases, the swelling blocks airflow to the throat to such an extent that the child does not get enough oxygen and is forced to suffocate. This is called false croup or laryngeal stenosis. Therefore, it is important to diagnose the disease early and treat laryngitis.
See your doctor right away if your child has laryngitis:
Advantages of the treatment blocks.
- High-quality and fast pain-relieving effect. The drug acts directly at the source of the pain.
- Low risk of side effects. The drug only enters the bloodstream after the source of the pain has passed.
- Good therapeutic effect.
- Ability to relieve vasospasm and muscle spasms and inflammation at the focal point.
- Possibility of multiple injections – each time the pain worsens.
- Restoring tissue trophism and reducing swelling.
- neck pain, back pain;
- osteochondrosis;
- neuralgia, neuritis;
- Pain in the spine caused by intervertebral fractures;
- Rheumatism;
- osteoarthritis;
- postoperative pain;
- phantom pains;
- Minnier syndrome;
- neuropathy;
- spasticity;
- pain after amputation;
- post-stroke pain and spasticity;
- Sciatica;
- Migraine;
- Sciatica;
- tunnel syndrome.
Types of therapeutic and diagnostic blocks
topical
The injection is made in the affected area, under or around the lesion, at the site of altered tissue reactions, inflammation, etc. Divided into periarticular (in tissues close to the joint) and periarticular (in nerve ducts).
Segmental
Injections into individual segments, these include paravertebral blocks, which are performed in the projection of spinal segments. Each spinal nerve and spinal segment corresponds to a dermatome (an area of the skin, connective tissue), sclerotome (an area of the skeletal system), myotome (part of the muscular system). Intradermal injection of the drug into the dermatome can affect the corresponding area of the spine and/or internal organ. The most common indication are myotonic reactions of the spinal muscles in osteochondrosis.
vertebral
This therapeutic blockade combines several techniques from the field of neurology. It is used for spinal pain. The anesthetic can be injected intradermally between the spinous processes of the vertebrae to a depth of 2-4 cm in the vertebral body area. In the latter case 3-4 cm lateral to the line of the spinous processes. The needle is inserted at an angle of 35° to a depth of 8-10 cm.
spinal blocks
Severe spinal pain is caused by pressure on the spinal nerves. The blockade has a targeted effect and normalizes the sensation. It is not an easy procedure and is therefore only used as a last resort.
The blockage temporarily cuts off nerve conduction through certain fibers. With the help of local anesthetics, the cellular conduction is blocked by inhibiting the potential-dependent sodium pathways.
Treatments are indicated for bulging discs, osteochondrosis, neuralgia, herniated discs, myositis, spondylarthrosis. Spinal blocks can be cervical, thoracic, thoracolumbar, sacral-lumbar, coccygeal, and paravertebral. The latter are divided into intradermal and subcutaneous (to numb the skin around the spine), intramuscular (to relieve muscle spasms and inflammation), and epidural (to shut down the damaged nerve).
surgical treatment
If the lymphatic tissue is replaced by connective tissue fibers, conservative treatment cannot help. The indication for the patient is tonsillectomy – removal of the tonsils. Tonsillectomy - the resection of the affected areas of the tonsils - is considered a more gentle method of modern surgery.
Preventive measures are aimed at preventing recurrence.
Preventive measures:
– Strengthening of the immune system. Systematic exercise, daily walks in the fresh air, hardening cures, taking immunity drugs as prescribed by a doctor.
- Give up cigarettes.
– Compliance with a rational regime of work and rest.
– Correction of the diet. Do not irritate the throat lining, so avoid hot sauces, pickles, hot condiments, citrus fruits, and pickles.
– Regular check-ups.
Doctors also recommend abstaining from alcohol.
Risk factors that aggravate the development of vascular leg disease:
- Smoking
- diabetes
- Obesity (body mass index over 30)
- High blood pressure (140/90 mmHg or higher).
- High total cholesterol level
- Relatives with vascular diseases.
People who smoke or have diabetes are at higher risk of developing lower limb vascular disease due to decreased blood flow.
complications
Vascular disease of the lower limbs leads to reduced physical activity and reduced ability to work. If the disease is caused by atherosclerotic plaques in the blood vessels, then there is a certain risk of complications:
- Critical ischemia of the lower limbs. This disease causes open ulcers that do not heal, lesions, or infectious lesions in the tissues of the limbs. Critical limb ischemia occurs when trauma or infectious lesions progress and lead to tissue necrosis (gangrene). In this case, the affected limb is amputated.
- stroke or myocardial infarction. Atherosclerotic plaques are not limited to the arteries of the legs. Fat deposits also build up in the arteries of the heart and brain, causing coronary artery disease, among other things.

Vascular disease of the lower limbs, even if it does not lead to the above complications, is accompanied by very unpleasant symptoms: pain when walking and at rest, limping, malaise, chills, etc. If the blood vessels in the legs hurt, then you cannot have a normal one live and are restricted in their physical activity.
Read more:- Damaged ligaments in the elbow joint.
- The parts of the human leg are named.
- parts of the human leg.
- What parts of the leg are called.
- What is the part of the leg below the thigh called?.
- outward rotation of the leg.
- Bone anatomy of the leg.
- How much does crooked leg surgery cost?.

