If a single transplant is used, the joint can be loaded the next day, but with some flexion restrictions. Otherwise, stress on the joint can be completely avoided for up to 3 weeks and then gradually increased for 3-4 weeks. After 10 weeks the patient can walk again.

- Mosaic chondroplasty of the knee: microfracture and cartilage transplantation
- Historical aspects of mosaic knee arthroplasty
- Mosaic plastic – questions about biomechanics and histology
- What happens to the donor site?
- Tibial bone graft for open sinus insertion
- Topographic anatomy
- Status Localis
- ICD-10 code: S82.7
- Local condition
Mosaic chondroplasty of the knee: microfracture and cartilage transplantation
The articular cartilage of any joint, including the knee, has extremely low potential for self-repair. Deep cartilage defects are very likely to lead to osteoarthritis. The incidence of these injuries is approximately 5 % of all knee injuries.
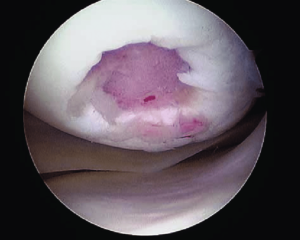
Local injury to the knee joint, arthroscopic view.
The treatment of local cartilage injuries remains a complex and controversial problem in orthopedics. Years of effort by doctors and researchers have focused on finding the best solution to repair the 'worn out' hyaline cartilage at the point of greatest stress.
In the early 1960s, a technique was proposed in which subchondral holes were drilled to stimulate stem cell growth, which appeared to ensure cartilage regeneration. This technique became widespread in the 1990s and was referred to as 'microfracturing'. It was used in a rather limited group of patients - young people with small and 'recent' cartilage damage.
In 1983, M. Brittberg and L. Peterson began using autologously cultured chondrocytes to treat cartilage damage. The essence of this method is to obtain and culture the patient's chondrocytes and then transplant them onto a periosteal flap. The results of this technique are quite satisfactory, but the method itself is technically quite complex. The implantation of autologous chondrocyte matrix using arthroscopic techniques is now widespread.
In the 1990s, various osteochondral transplantation techniques were also proposed and actively used. This term refers to the transplantation of bone and cartilage fragments from one area of the joint to another area of damaged cartilage.
Historical aspects of mosaic knee arthroplasty
Large osteochondral grafts derived from the patellar surface, medial and lateral condyles, and intercondylar sulcus were initially developed. These techniques were too invasive to obtain sufficiently congruent grafts and often resulted in compromised joint biomechanics.
Therefore, the use of multiple cylindrical osteochondral grafts has been suggested. A successful operation using this technique was reported in 1993 by Matsusue et al. demonstrated. The operation successfully closed a 15 mm defect in the femoral condyle caused by a tear in the anterior cruciate ligament. The technique is known as mosaic sculpture.
Mosaic plastic – questions about biomechanics and histology
- Grafts with a diameter of 11 mm and lengths of 15 and 20 mm have better vertical stability;
- A perfect match between the length of the graft and the depth of the 'implantation socket' provides 2-3 times better stability;
- Grafts with press-fit fixation are more stable (this effect is due to the transplanted osteochondral fragment itself being slightly wider than the implant hole).
What happens if the curvature of the graft does not match that of the reconstructed area?
Studies in sheep have shown that a curvature deviation of up to 1 mm is acceptable and the cartilage survives; with a deviation of 2 mm or more, aseptic necrosis occurs and the graft gradually dissolves.
Does the viability of a cartilage graft depend on fixation strength?
Chondrocytes are not damaged with a fixation force of up to 10 MPa, but cartilage damage occurs with a fixation force of more than 15 MPa. It is therefore recommended to insert the graft with several gentle pressures rather than a single strong pressure.
What happens to the donor site?
Follow-up examinations during arthroscopy have shown that the donor site remains empty; only after a sufficiently long period of time does slight settlement and the formation of fibrous tissue occur in the depths.
Attempts have been made to fill the defect with an osteoperiosteal plug from the tibia, but even this does not guarantee bone filling.
If we briefly summarize the above considerations, the following conclusions can be drawn:
- Osteochondral grafts from the lateral and medial surfaces of the condyles as well as from the intercondylar sulcus can successfully correct cartilage defects;
- the diameter of the plug must be slightly larger than the planting hole;
- the length of the graft should correspond to the depth of the planting hole;
- the press fit method is preferred;
- the osteochondral implant remains viable for a long time and ensures normal function of the joint.
Tibial bone graft for open sinus insertion
There are now many different types of bone building. Different materials from different origins can be used to achieve a high clinical success rate. However, in some cases it is necessary to choose the technique by which the procedure will be carried out.
There are specific indications for each method, although it is possible to take different approaches in the same clinical case.
There are currently a large number of different bone replacement materials on the market that are used in augmentations. Most of them have been successfully clinically tested and are used for bone deficiency.
At the same time, there has always been a 'gold standard' in the past. The most popular option is the iliac crest autograft.
Autografts offer the highest clinical success rate, have undergone the longest clinical trials, and have the most experience in use.
The main difference in using autografts compared to xenografts is the invasiveness required.
The higher invasiveness of autograft harvesting is a negative factor compared to the use of various bone substitute materials.
This article uses a clinical case to demonstrate the ease of using autografts with a relatively low degree of invasiveness. The benefits of using the proximal portion of the tibia as a donor site for cancellous bone grafts have been the subject of numerous studies. Postoperative discomfort is significantly lower with the tibia than with the iliac crest (IBS).
Topographic anatomy
Most of the BC is subcutaneous and the proximal part and condyles are palpable below the knee.
The BC tuber is located on the anterior edge of the bone between the condyles and can be felt as an oval protrusion. Palpation of the BC tuber is extremely important to avoid damage to the articular surfaces of the knee.
In the immediate vicinity of the medial surface of the BC, small branches of the medial surface of the inferior patellar artery pass under the patellar ligament.
We would like to explain this technique using a clinical case example.
A patient presented to the clinic complaining of missing teeth in areas 14 and 15. Following the examination, the patient was prescribed a treatment plan that included an open sinus lift and simultaneous implantation in the area of teeth 14 and 15. Autologous bone is removed from the BC using the F. Alfaro technique.
Status Localis
Status Localis
ICD-10 code: S82.7
Condition of moderate severity. The skin was pale. No alveolar breathing, no rales, rhythmic heart tones, 80 per minute, blood pressure 110/70 mm Hg, abdomen soft in all parts and not painful.
Local condition
There is a marked deformity of the left tibia at the c/3-n/3 border, the foot is rotated outward from this level.
On palpation, the entire left tibia is painful; on percussion, the pain increases as it irradiates the area of deformity. There is a significant absolute shortening of the left tibia of 5 cm.
The comparative examination of both feet shows: the circumference of the left ankle is +1.5 cm larger.
Movement in the ankle joint is limited due to severe pain; Passive movement in the knee joint is preserved, active movements are not carried out due to the pain.
When the bandage is removed, a wound with irregular edges in the middle third of the shin bone measuring 10x15 cm is revealed. At the bottom of the wound there are muscles, fragments of fascia, and a 12 cm long distal fragment of the tibia protruding forward. The wound bleeds moderately.
A second, 10 cm by 3 cm wound in the area of the inner ankle, up to 5 mm deep, the wound bed is periosteal. Pulsation in the peripheral arteries is questionable.
There are also several abrasions on the tibia measuring 3 x 4 cm.
Read more:- How long it takes for the ligaments to heal.
- tibial fasciitis.
- lateral bone.
- syndesmosis.
- Immobilization of the knee in osteoarthritis.
- How much does knee surgery cost?.
- Ellipsoid in knee osteoarthritis.
- The intercondylar syndesmosis is the.
