Vitamin and mineral supplements: strengthening the immune system, revitalizing the body

- Symptoms and treatment of knee muscle pain
- pain above the knee
- Diagnostic risks
- Anatomy of the iliopsoas muscle
- What causes muscle damage?
- Causes of inflammation of the iliopsoas muscle
- Treatment of thigh muscle pain.
- Exercise therapy for muscle pain in the hip
- Clinical relevance
- Consequences of weakness and tension
- Self-exercises for the muscles. Massages. Friction therapy
- Stretch
- Prevention of abdominal muscle pain
- causes
- Symptoms of tendonitis
- Symptoms:
- diagnosis
- Symptoms of Achilles tendon inflammation and rupture.
- Treatment of the Achilles tendon
- medication
- Leg cramps and magnesium
- Leg cramps and calcium
Symptoms and treatment of knee muscle pain
Leg muscle pain can occur above or below the knee. Doctors at Yusupov Hospital use modern examination methods to determine the cause. Comprehensive treatment is aimed at eliminating the factors that caused muscle pain, influencing the mechanisms of disease development and eliminating the pain syndrome. For this purpose, Yusupov Hospital uses the latest drugs with high effectiveness and minimal side effects. Professors and doctors of the highest category use their own methods of rehabilitation therapy. Rehabilitation therapists prescribe effective physiotherapeutic procedures, use modern manual therapy techniques and carry out acupuncture treatments. The high level of expertise of specialists, the patient-centered approach to the treatment of diseases that cause muscle pain above or below the knee and the use of modern techniques allow the doctors of the rehabilitation clinic to enhance the effect of drug therapy and prevent exacerbation of the pathological process impede.

pain above the knee
In this case, topical ointments and oral non-steroidal anti-inflammatory drugs are very helpful.
Muscle pain below the knee is a symptom of many diseases:
- mechanical damage to muscle fibers and tendons;
- varicose veins of the lower limbs;
- Obliterating atherosclerosis and arteritis;
- Myositis and nerve inflammation.
The most common cause of muscle pain in the legs below the knee is heavy physical exertion. Mild tendon injuries do not cause serious clinical symptoms other than occasional pain when walking. Mechanical muscle damage that occurs over time from constant movement is exacerbated by inflammation, resulting in swelling below the knee.
The second most common cause of knee muscle pain is a spinal disorder in which the nerve endings are compressed:
They increase when the posterior region of the lower leg is palpated and when the body is suddenly bent. The cause of leg muscle pain below the knee is synovitis (inflammation of the muscle coverings under the tendons). It occurs due to osteoarthritis of the knee joint or damage to the meniscus. If the joint space of the knee joint is severely narrowed, the cartilaginous structures are damaged and an inflammatory fluid forms. This accumulates in the tendon sheaths and causes swelling in the back of the knee.
Pain in the muscles below the knee can be caused by
- nerve damage (polyneuropathy),
- Bone inflammation (osteomyelitis);
- taking medicines (statins);
- decreased levels of calcium, potassium and magnesium in the blood;
- Disorder of bone formation in children and adolescents (Osgood-Schlatter disease).
The muscle pain below the knee is not localized. It extends 10-15 cm, indicating that the anatomical structures of the lower limbs are large in area. The pain syndrome increases with exercise and decreases when exercise is stopped. Muscle pain below the knee bothers smokers. Severe pain is caused by deep vein thrombosis in the lower leg. They are localized below the knee and increase in the anteroposterior direction with dorsiflexion of the foot and compression of the lower limbs.
Diagnostic risks
- The sufferer begins to feel unwell, with reduced activity and performance and a general feeling of emptiness.
- The fever can increase, but usually remains at a low level.
- The body begins to hurt, the muscles ache, general weakness increases, the patient becomes hot and sweats more.
In the vast majority of cases, vertebral disease develops on the right side of the body because this area is subject to greater stress. The situation is different for left-handers, as they compensate for this mechanism by shifting the main load to the left side, which causes it to suffer more.
Diagnosing inflammation of the iliopsoas muscle is difficult due to its proximity to the spine. Due to the brachial plexus running nearby, it is difficult to determine the exact location of the pain. The disease is often confused with osteochondrosis or plexitis. Incorrect prescription of anti-inflammatory and analgesic medications can relieve the discomfort, but the lack of appropriate treatment causes the disease to become chronic and periodically recurring. Therefore, choosing a doctor is an important step on the road to recovery.
Anatomy of the iliopsoas muscle
The anatomy of this area includes the fusion of the psoas minor, psoas major, and iliopsoas muscle. In the distal sections, the muscles separate into bundles and form a new muscle, which is part of the internal structure of the pelvic muscles. The proximity of the spine provides diffuse nutrition to the cartilaginous elements of the intervertebral space.
Physiologically speaking, the iliopsoas muscle surrounds the hip joint and is anchored by a tendon fiber in the front area of the trochanter of the thigh. This is the reason for the involvement of this structure in the movements of the lower limbs. The inflammation leads to pain when moving the leg, such as B. when kicking, squatting or moving your leg back and forth.
What causes muscle damage?
Muscle damage can be caused by trauma (shocks, bruises, accidents), inflammation in nearby structures, poor circulation, and nutrient deficiencies. The inflammation may be a response to a sprain or to the action of osteophytes that have formed on the vertebrae and the intervertebral discs that separate them.
Another possibility of injury is compression caused by swelling of the surrounding tissue. Avoid excessive training and calculate your strength carefully. Caution should be exercised when performing exercises such as splits and stretches, especially for people who are learning these techniques for the first time. If the muscle fibers of the iliopsoas muscle are torn, you can expect a long recovery time.
Causes of inflammation of the iliopsoas muscle
A common cause of inflammation is infection. The most likely pathogens are Staphylococcus aureus, E. coli, streptococci and other pathogens. The infection spreads best among people with poor health and weak immunity.
The following factors contribute to the development of the pathological condition:
Treatment of thigh muscle pain.
Before starting treatment, doctors at Yusupov Hospital determine the cause of muscle pain in the hip using modern diagnostic methods:
- MRI of the lumbar spine;
- X-ray of the hip joint;
- Ultrasound examination of the blood vessels in the lower limbs.
Treatment methods for hip and leg muscle pain depend on the cause of the pain. As soon as the cause of the pain syndrome is identified, doctors at Yusupov Hospital eliminate it, stop the progression of the disease and carry out rehabilitation therapy to strengthen the spine, muscles and ligaments.
How can muscle pain in the thigh be relieved? Hip muscle pain can be relieved by stretching the muscles of the painful limb in the area where the pain occurs and the opposite area on the other leg. If the pain occurs in the back of the right leg, stretch the back on the right side and the front on the left side. If you have osteoarthritis in your knees, perform stretches on the entire surface of your hips. If you have pain on the outside of your hip, do the following exercise: lie on your back, without removing your arm from the same surface, turn the painful lower limb to the opposite side and let it hang there, being relax your muscles. Perform the exercise for 5-6 minutes.
Rub the skin of the thigh with a warming or pain-relieving ointment. Place the painful limb horizontally by elevating the leg to 30° (you can place a pillow or pad under the lower leg). If varicose veins are the cause of hip pain, phlebologists recommend wearing compression stockings or tights in bed in the morning. If there is inflammation of the hip muscles, taking non-steroidal anti-inflammatory drugs (ibuprofen, diclofenac, nimesulide) relieves the pain.
Rehabilitation therapists use tape for muscle tension and hip pain. To attach the band to the hip joint, the patient must lie on his back. Both legs are stretched and bent at the knee joints (frog position). Rotate the leg outward to stretch the groin (adductor group of the thigh). Place the anchor of the stabilization band on the thigh and spread the band on the inside so that it ends just above the knee. Place the tape around your thigh with almost no tension.
Exercise therapy for muscle pain in the hip
A senior physiotherapist at Yusupov Hospital individually selects a set of exercises for each patient with muscle pain in the hip and leg to relieve muscle spasm and increase muscle tension. There is a physiological reflex that causes the muscle to relax when stretched for a long period of time. It is triggered after about 2 minutes of continuous stretching of the muscle. The relaxation lasts for about 6 hours. This series of exercises is based on the effect of this reflex. They do not act on the cause of the disease, but are symptomatic - they relieve muscle pain in the hip.
Stand on the healthy leg and bend the painful lower extremity at the knee. With the appropriate hand, grasp the ankle joint and pull it backwards, stretching the front of the thigh of the painful leg. Hold the tension for 2-3 minutes and then slowly release the leg. This exercise helps with pain in the front thigh muscles.
To stretch the hamstrings, do the following exercise:
- Stand on the good leg and stretch the painful leg on a chair;
- Bend the other leg to the maximum, tensing the back of the thigh;
- Hold the tension for 2-3 minutes and then slowly remove the leg from the chair.
Stretching the lower leg muscles helps with pain in the back of the thigh. Go to a wall or other vertical surface. Place the foot of the sore leg against the wall - heel on the floor, sole on the wall. Pull the knee of the lower limb and the entire upper body as close to the wall as possible and tense the calf muscles. Hold the tension for 2 to 3 minutes and then slowly remove the leg. This exercise helps with leg pain below the knee.
The cause of the muscle pain should be clarified by your doctor. If the pain does not subside or increases within a week despite treatment and exercise, call Yusupov Hospital. After a comprehensive examination, doctors will determine the cause of muscle pain in the hip and leg, carry out drug treatment of the disease and prescribe physiotherapy treatments. An individual exercise complex developed by rehabilitation specialists, acupuncture and innovative manual therapy techniques will allow the patient to get rid of hip muscle pain, regardless of the cause.
Clinical relevance
- Tear of the tendon of the tibialis posterior muscle
- Crack of the tibia
- Dysfunction of the tendon of the tibialis posterior muscle is considered the likely cause of most cases of acquired flatfoot in adults. [3]
- In cases of cockle walk due to deep peroneal nerve paralysis, surgery is performed to relocate the posterior tibialis muscle tendon to the dorsum of the foot to compensate for the loss of dorsiflexion due to paralysis of the anterior tibialis muscle. [4]

Location of the trigger points
Consequences of weakness and tension
Consequences of weakness of the tibialis posterior muscle
Weakening of the tibialis posterior muscle impairs inversion force and results in a decrease in force of at least 50 % [42]. The tibialis posterior muscle is an important stabilizer of the forefoot, and its weakness affects a person's ability to stand on their toes, even with intact plantar flexors, because the foot is unstable. Weakness also leads to an imbalance with the hindfoot muscles, and the foot tends to roll outwards and backwards, i.e. prone to pronation [25,55,89]. Patients with tibialis posterior tendon dysfunction (TADD) demonstrate increased pronation in the hindfoot and forefoot, reflecting the extensive role of this muscle in supporting the majority of the foot [89]. DSFBM is a major cause of acquired flatfoot and alters the normal movement of the tarsal bones during weight-bearing and walking [31,69]. Factors associated with an increased risk of DSFBM include obesity, age, hypertension, diabetes, and lack of tendon vascularization [31]. Pre-existing flat feet also appear to be a risk factor for rupture of the posterior tibial muscle. [16]. Arai et al. reported increased sliding resistance of the tibialis posterior muscle around the medial ankle in people with flat feet [4]. Increased frictional forces on the tibialis posterior tendon may contribute to an increased risk of tendon rupture in people with flat feet.
Rupture of the posterior tibialis muscle tendon
A spontaneous rupture of the tendon of the tibialis posterior muscle causes pain and significant functional impairment. It often occurs after a prolonged episode of chronic tendonitis. The association with pre-existing foot deformities, obesity, age and hypertension suggests that measures to control flat feet, such as: B. Pronation restrictions, can help reduce stress on the tibialis posterior muscle tendon and prevent rupture. Outcome studies are needed to determine the effectiveness of such measures.
Self-exercises for the muscles. Massages. Friction therapy
There are many ways to treat cambialis muscle pain. For moderate injuries, it is often sufficient to lift the toes with the knees bent and avoid excessive strain. In this case, recovery will take several months.
The biggest mistake is resuming normal activity too soon - before the muscle has fully regained its function.
Friction therapy combined with massage accelerates the recovery process and shortens recovery time to 4-6 weeks for minor injuries and 8-12 weeks for severe injuries.
During friction therapy, the patient must lie face down on the massage table. Approach the table from the side and bend the client's leg at the knee to 90 degrees. Place the client's ankle on your shoulder and keep the knee bent at 90 degrees. Place your hands around the leg so that your fingertips point straight toward the middle of the calf, holding the shin with your thumb. Move your fingertips toward the middle of the calf muscle to make contact with the cambialis muscle. While applying pressure to the anterior back muscle, move horizontally from medial to lateral for 1-2 minutes. Then move your hands to another part of the camelback muscle and treat the entire area one at a time. After 5-6 minutes, let the client rest and repeat the process. After these rubs, massage the calf muscle for 5 minutes.
Stretch
Start with a warm-up - walk for a few minutes or bend and straighten your legs while sitting. Then sit on the floor and bend one leg at a 90 degree angle. Your knee should be facing the ceiling and your foot should be planted firmly on the floor. Make sure your foot is flat against your shin (not turned in or out). First, lift the toe towards the shin by tensing the muscles, then grab the foot with your hands and pull it towards the knee (see illustration). Pull the sock out for two seconds and then lower your foot to the floor. Do not pull the sock out for more than two seconds. Repeat this exercise 8-10 times with each foot.
Stand straight and rise onto your toes with your knees bent. Feet should be parallel and shoulder-width apart. Raise yourself on your toes 3 times for 10 reps, with a short rest between sets. If you find these three repetitions easy, you can make the exercise more difficult by rotating your feet in and out 45 degrees.
You can also make the exercise more difficult by placing your toes on the edge of the step, with your heel not parallel to your foot. Try starting with your legs straight and gradually bending your knees.
The final step is to use weights. You must learn to perform this exercise with a weight while standing on one leg and holding onto an object to give you support. This exercise not only works the cambium muscles, but also the calf muscles, especially when the knees are bent. The stronger these muscles become, the easier it becomes for the client to perform all phases of the exercise with the knees bent.
Prevention of abdominal muscle pain
Preventive measures against abdominal pain have not yet been developed because the causes of abdominal pain are very diverse. In addition, due to its non-specific nature, the syndrome cannot be prevented, but there is
Prevention of abdominal muscle pain, which concerns the so-called training pain. If one speaks of abdominal muscle pain as a specific, independent symptom, ie as damage to the muscle tissue, it is usually related to overload, overexertion, carrying weights and incorrect weight distribution. Preventive measures should therefore look like this:
- Adapt your physical abilities appropriately to the task at hand.
- Remember to warm up the muscles of the entire body, including the abdominal muscles.
- Choose an exercise program that is tailored to your individual needs, taking into account any chronic illnesses you may have.
- Make sure you take breaks between heavy loads.
- Distribute the weight evenly and maintain a straight posture when carrying weights.
- Regularly train your muscle corset, including the back and abdominal muscles.
- At the first sign of pain, take breaks and give overworked muscles a break.
In addition, prevention of abdominal pain syndrome can consist of a routine examination that every adult should undergo annually. A comprehensive check-up at least once a year statistically reduces the risk of abdominal muscle pain by 55-60 %.
Abdominal muscle pain is not a pathological symptom, as it is a muscle structure that regenerates quite quickly, but any discomfort in the abdominal cavity can be a sign of a serious illness. As the saying goes, there are a thousand diseases, but health is one, so it's best to take care of it and save it in advance.
An additional tab for information about items, delivery or other important content. It will help you answer your buyers' questions and dispel their doubts about the purchase. Use them at your own discretion.
causes
Achilles tendonitis is more commonly diagnosed in athletes and is a result of overuse, poor technique or an incorrect training plan. It can be diagnosed in 40 to 60 year olds after a single high load on the Achilles tendon (e.g. during a running test). The high likelihood of tendonitis is due to the increasing stiffness of the Achilles tendon with age and a certain limitation in the range of motion in the ankle joint.
In clinical traumatology and orthopedics, three forms of tendinitis are distinguished. Peritendinitis is an inflammation of the tissue surrounding the Achilles tendon. Peritendinitis is an inflammation of the tendon itself, leading to degeneration of the tendon. Enthesopathy is an inflammatory process at the attachment of the Achilles tendon to the heel bone, which can be associated with a heel spur and calcification of the tendon tissue. All three forms of the disease can occur in isolation or simultaneously, or progress from one to the other.
Symptoms of tendonitis
The disease develops gradually, initially the patient feels pain in the ankle (Achilles tendon) only in the first few minutes of stress or training. After warming up, the pain decreases and disappears completely with rest. There will be some discomfort when palpating the affected area, but usually no pain. If the disease remains untreated, it will eventually become chronic. The pain increases within a few weeks or months. In contrast to the initial stage, the pain increases rather than decreases after warming up. Even prolonged rest does not provide relief, and some patients still experience pain even after a full night's sleep.
Many patients report pain when walking downhill, climbing stairs or on an inclined plane. Examination reveals tightness of the calf muscle, thickening of the Achilles tendon, local congestion, and a local increase in skin temperature in the affected area. The range of motion of the ankle joint is somewhat limited. In tendinitis, the pain is usually limited to the entire tendon; in tendonitis, it is 2-6 cm above the heel; in enthesopathy, it is at or just above the tendon attachment point.
Symptoms:
– Pain on the inner surface of the ankle and foot
– Pain at the beginning and end of running
– Pain when palpating the inside of the ankle
– in advanced cases the pain can be almost constant
– Discomfort caused by pronation of the foot (movement in which the foot turns outwards)
– Pain when the ZBM contracts against resistance, in severe cases when the sole is flexed or the foot is inverted
– Sensation of impact in the calf muscles
– Restriction of dorsiflexion of the foot.
As already mentioned, the ZBM performs plantar flexion and inversion of the foot. These movements are accompanied by a shortening of the muscle or its concentric contraction. However, the muscle can also work eccentrically, which is a much more difficult task. Eccentric contraction is characterized by a slow lengthening of the muscle.
When running, the ZBM slows eversion (from the moment the heel hits the ground to the beginning of the mid-stance phase).
There are several factors that can lead to the development of tendinopathy - one of which is a general reduction in the height of the arch of the foot. Against the background of a high volume of running, this can lead to degenerative changes in the tendon.
Excessive pronation, high heel eversion angle, and transverse stereotypy can all be causes of increased stress on the tibialis posterior tendon. 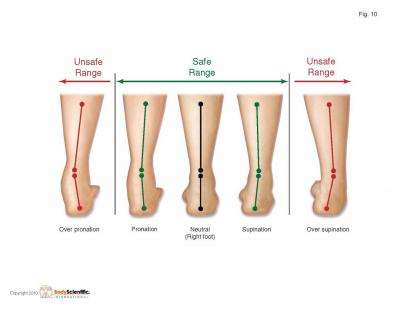

diagnosis
– Tactile examination: the area behind the inner ankle may be swollen and painful, the tendon itself is thicker when comparing its size with that of the opposite side
– Running analysis: The pronation time is increased and can persist even when pushing off with the toes
– USG, MAGNETIC RESONANCE TOMOGRAPHY
Treatment
Peace and relaxation
Continuing to run makes the situation worse. However, rest alone is not enough; the cause of the tendinosis must be treated.
To give the tendon a 'rest' (if you are 'on your feet' all day), you can apply taping to reduce pronation and thus reduce the stress on the tendon (video or photo).
Shoes that support the arch of the foot also reduce stress on the tendon.
Another way to reduce the strain is to use shoe insoles. A well-fitted orthosis can make life much easier, especially at the beginning of rehabilitation.
exercises
Strengthening the tibialis posterior muscle is key to treating and preventing this condition. Functionally, this muscle moves the foot from dorsiflexion and eversion to plantarflexion and inversion. With this movement we will work by gradually increasing the load. The following exercises can be used in the first phase:
Symptoms of Achilles tendon inflammation and rupture.
- Tactile and stepping pain in the heel area, which increases with exertion and decreases at rest;
- swelling of the ankle joint;
- Redness and warming of the skin in the back of the ankle;
- Crunching and pain when trying to turn the foot;
- Impairment of mobility in the soleus level;
- noticeable stiffness of the tendon, loss of the ability to stretch normally;
- Difficulty climbing stairs, jumping and toe-climbing.
- Swelling of the ankle joint with a 'sunken' ankle at the site of the tear;
- Stitching pain, especially when trying to stand on your heel or toes;
- Severe difficulty walking.
- tendon injuries (open and closed);
- Inflammatory, metabolic, viral and other diseases that do not directly affect the Achilles heel (gout, rheumatoid arthritis) or occur in its immediate vicinity (heel spurs, tendinitis, achillobursitis);
- congenital problems with the Achilles tendon (insufficient length from birth and paralysis of the foot) or collagen synthesis, constitutional features;
- others (age-related, biochemical, habitual).
Injuries and. Achilles tendinitis can be caused by infectious diseases as a result of taking fluoroquinolone antibiotics. Even within the first 48 hours after surgery, any severe strain on the Achilles tendon can lead to a rupture.
The tendon can also be damaged by being overweight or wearing uncomfortable shoes (too tight or with high heels). This deforms the collagen fibers and reduces their strength. A sedentary lifestyle increases stress Achilles tendon. This is due to the poor development and shortening of the calf muscles, which help the Achilles tendon distribute the load.
Treatment of the Achilles tendon
conservative Treatment of the Achilles tendon Conservative treatment of the Achilles tendon consists of relieving pain, reducing swelling and protecting the affected tissue. The etiology of the problem influences the treatment strategy. For example, if an x-ray shows calcification of the Achilles tendon.If the patient suffers from tendonitis, shock wave therapy and, if necessary, surgical treatment are recommended.
If Achilles tendon If the Achilles tendon hurts due to an injury, a local anesthetic (for example, Novocaine) and a plaster cast should be applied. In case of complete tear and detachment, suture surgery is always required.
medication
Under In the treatment of the Achilles tendon Two groups of drugs are mainly used in the treatment of Achilles tendon: NSAIDs (non-steroidal anti-inflammatory drugs) and chondroprotectors. NSAIDs (same as NSAIDs) help relieve symptoms of inflammation and reduce pain and swelling. They are usually prescribed in the form of gels, ointments and compresses, but in cases of severe Severe Achilles tendonitis However, tablets can also be used as a supportive measure. Treatment with oral NSAIDs usually lasts 10-12 days. External anti-inflammatories can be used for several weeks or even months (for tendon injuries). If Achilles tendon pain Even after using NSAIDs, glucocorticosteroids are prescribed for severe tendonitis.
The value of chondroprotective agents in the Treatment of the Achilles tendon are their effects on collagen synthesis and the health of joint structures. This group of drugs also has a preventive effect and is therefore recommended for regular use by people who are at risk of developing Achilles tendon disease (competitive athletes, patients with musculoskeletal system diseases). Since the Achilles tendon has no blood vessels, the regeneration of its tissue usually occurs very slowly. Taking chondroprotectors helps speed up this process and prevent the formation of abnormal, unstable collagen fibers.
Leg cramps and magnesium
Leg cramps can also simply be an expression of metabolic disorders in the muscles, such as chronic magnesium deficiency.
This is probably a very common cause of. Magnesium is a unique mineral that is involved in hundreds of biochemical processes in the human body (according to current research, magnesium is involved in about 300 biochemical processes in the human body). Magnesium is needed everywhere, but is not supplied with food, as only small amounts of foods containing magnesium (bran, nuts, pumpkin seeds, sesame) are consumed. Magnesium is most commonly produced in stressful situations (it is essential for the nervous system), during strenuous physical exertion or in hot weather (it is excreted in sweat), when drinking large amounts of fluids (it is excreted in urine), and during frequent consumption of alcoholic beverages Drinks consumed. When there is a magnesium deficiency, the muscles tend to tense and cramp. For the same reason (magnesium deficiency) the eyelid can 'twitch' - the circular muscle of the eye is sensitive and reacts very sensitively to magnesium deficiency.
Recently I was asked if there were alternatives to magnesium supplementation besides taking Magne B6. There are – other preparations containing magnesium: Magnerot, Magnecum. Magnesium is thought to be well absorbed by the intestine in the presence of pyridoxine (vitamin B6) or as orotic acid salt, but in the diet magnesium is often accompanied by calcium or phosphorus and these prevent magnesium absorption in the intestine. When food is cooked, its content is greatly reduced. And thanks to the rapid development of 'new technologies', food also contains less and less of it. Of course you can get magnesium through a proper diet, but you have to want it.
Leg cramps and calcium
Calcium is also responsible for the ability of muscles to contract. Calcium deficiency (hypocalcemia) may be a metabolic cause of leg cramps.
Calcium is needed for muscle work during the day and for bone formation at night.
Hypocalcemia is usually difficult to diagnose in the early stages. Subtle muscle spasms can occur in the muscles of the legs and back, and sometimes even in the muscles of the face. At the same time, there may be a tingling sensation in the tip of the tongue, lips and fingers. Only in the advanced stages do carpel cramps occur (persistent and very painful strong flexion of the foot and finger flexor muscles) and tetany attacks (with laryngeal cramps and generalized, life-threatening cramps).
Calcium deficiency, on the other hand, can lead to a variety of diseases. The most common are hypoparathyroidism (parathyroid hormone deficiency leads to reduced calcium concentrations in the blood), vitamin D deficiency (decreased calcium absorption in the intestine), chronic kidney disease (decreased calcium reabsorption in the kidneys leads to increased calcium excretion, and vitamin D synthesis in the kidneys decreased), in acute pancreatitis (fatty necrosis binds calcium to fatty acids and increases the secretion of glucagon and calcitonin), as well as when taking certain medications (antacids, rifampicin, phenobarbital, phenytoin, ie, which lower the calcium concentration in the blood). However, in reality, there are many causes of low calcium levels that should be identified through appropriate examinations.
If it Cramps in the legsIt's up to you to decide whether you need to worry or not. However, in my opinion, any change in our body is not random and must be taken into account. However, do not engage in self-medication and self-diagnosis. See your doctor and stay healthy!
Read more:- Tibialis posterior muscle.
- lower leg flexion.
- Sore muscles in the calf.
- shin tendon.
- The long section of the big toe.
- muscles in the legs.
- lower leg muscles.
- Exercises for the triceps tibialis muscle.
