With a small perforation, the recovery time is up to 10-14 days – if the patient complies with all the prescribed medications and non-pharmacological treatments, during this time the integrity of the tympanic membrane will spontaneously recover.

Earditis or tympanitis (Latin: myringa) is an inflammatory process in the membrane tissue, usually associated with infections caused by pathogenic microorganisms that have entered the inflamed area from the surrounding tissues or from the bloodstream.
The inflammatory response develops according to the usual mechanism. First, the body releases cytokines, ie specific proteins that trigger an immune response to the attacking pathogens. Under the influence of cytokines, the blood vessels of the eardrum expand, and blood plasma of certain form elements is released through their walls into the surrounding tissues, which leads to swelling and congestion of the eardrum.
The development of inflammation is accompanied by tinnitus, discomfort and pain in the ears, sometimes with fever and hearing loss. When the disease progresses to a chronic or hemorrhagic stage, blood- and pus-filled blisters form and rupture, exuding exudate.
- Current treatment
- Cure for Ear Infection.
- treatment of the chronic form
- General information.
- causes
- Methods for diagnosing damage
- Myringoplasty: stages of the operation
- flap placement
- indications
- contraindications
- expert opinion
- Treatment of perforation of an eardrum
- class of reptiles
- Causes and clinical features
- otitis media
- Aerotitis (aerogenic perforation)
- Direct membrane damage
- diagnosis of a rupture
- Causes of Carpal Tunnel Syndrome
- Symptoms of Carpal Tunnel Syndrome
- prevention
- Benefits of treating otitis media at Rebenok Clinic
Current treatment
People with tympanitis in most cases do not seek medical attention until unpleasant purulent discharge from the ears appears and the treatment of the disease is complicated. The diagnosis is confirmed by a medical examination, otoscopy, ultrasound, and laboratory tests. Determining the type of pathogen will help choose the right treatment. Difficulties in diagnosis arise from the fact that the disease has symptoms similar to otitis media. In contrast to otitis media, in tympanitis the Eustachian tube is not damaged, so the otolaryngologist checks its integrity by blowing.
Treatment depends on the stage of the disease. With acute inflammation, painkillers, antiseptic solutions and anti-inflammatory drugs are prescribed. If an abscess is present, it is opened with a needle, as are blisters on the surface of the membrane in the ear. If there is a discharge from the affected ear, a small gauze pad is inserted into the ear canal. The acute form passes within four days with appropriate treatment.
Cure for Ear Infection.
Local treatment is with anti-inflammatory and pain-relieving ear drops, e.g. B. Otenum and others. If the disease appeared against the background of flu, then treatment is carried out with antiviral agents. Antiviral drugs, e.g. B. Anaferon, are used to eliminate the viral infection. Vasoconstrictor drops are put in the nose. Amoxicillin is commonly prescribed as an antibiotic. Erespal is used as an antihistamine. In addition to drug treatment, physiotherapy and ear wraps are also used. The dosage and duration of drug therapy can only be determined by the doctor.
treatment of the chronic form
The chronic stage is more difficult to treat. The affected ear is soaked in boric acid alcohol or resorcinol. Warm carbolic glycerin and powdered boric acid can also be used to blow into the affected ear. The droppings should always be removed. Long-term treatment and following all doctor's orders can restore ear health. Sometimes the disease cannot be treated with medication and part of the damaged eardrum must be surgically removed.
General information.
The eardrum is located at the end of the ear canal and separates it from the tympanic cavity of the middle ear. It consists of three layers: the outer layer, which is an extension of the epidermis of the skin of the ear canal, the middle layer, which consists of radial and circular fibers, and the inner layer, which is the mucous membrane of the tympanic cavity. The eardrum has a protective function by preventing air, water, foreign objects and microorganisms from entering the middle ear. The second function of the eardrum is to conduct sound. The sound waves generated by the eardrum are transmitted from the eardrum to the auditory system in the inner ear via the chain of auditory ossicles. The severity of the damage to the protective function and sound conduction from an injured eardrum depends on the type and extent of the injury to the eardrum.
Injury to the eardrum can lead to complete destruction, partial or complete rupture, damage to the integrity of individual layers or components of the eardrum. Damage to the tympanic membrane, accompanied by a violation of its integrity, is considered infectious and carries the risk of infectious complications: acute otitis media, chronic purulent otitis media, labyrinthitis, mastoiditis, otomycosis, etc.
causes
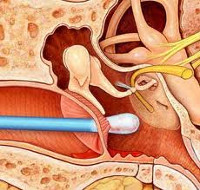
Mechanical damage to the eardrum can result from trauma to the ear, a foreign object, inappropriate attempts to remove earplugs, or the use of inappropriate objects (pins, matches, paper clips, etc.) to clean the external auditory canal. Damage to the tympanic membrane can occur with traumatic brain injury, which is accompanied by a fracture of the temporal bone pyramid and damage to the integrity of the tympanic cavity.
Physical factors that can cause damage to the eardrum include, in particular, sudden pressure differences within the eardrum cavity and the external auditory canal. Acoustic (barometric) damage to the eardrum can occur as a result of falling on the ear, hitting the eardrum, severe sneezing with a closed nose, staying in an explosive zone, diving or caisson work, testing in a hyperbaric chamber, jumping into water from a great height. Acoustic damage to the eardrum is the result of overstretching, can vary in severity and can be accompanied by aero-otitis and aero-sinusitis. Barotrauma of the ear can result in structural damage to individual layers or elements of the eardrum, damage to a vessel running through the eardrum, or complete rupture of the eardrum.
Thermal damage to the eardrum is usually accompanied by a burn of the pinna. They can occur both in the home and in industry (forging, pottery, metalwork). Chemical damage to the eardrum occurs when caustic chemicals (acids and bases) get into the ear canal. This often leads to a complete rupture of the eardrum and penetration of the caustic substance into the eardrum and through it into the inner ear. Other types of eardrum injuries include gunshot wounds and shrapnel wounds.
Methods for diagnosing damage
A trauma surgeon or an ENT doctor should be consulted if there are symptoms that indicate a perforation of the eardrum. After examining the injured area, an otoscopy is performed. If membrane defects are detected, a more accurate diagnosis of the pathology is carried out. This consists of the following measures:
- stylography;
- audiometry;
- vestibulometry;
- electrocochleography;
- acoustic impedance;
- ventricular examination.
A comprehensive diagnosis makes it possible to assess potential damage and initiate therapy. It can be surgical or non-surgical.
Myringoplasty: stages of the operation
Laryngoplasty is a surgical procedure to close a ruptured eardrum. It is performed both as a standalone procedure and as part of a larger tympanoplasty. The aim of the procedure is to protect the middle ear cavity from infection and improve hearing.
The main indication for tympanoplasty is a non-healing hole in the diaphragm caused by a chronic form of purulent otitis media.
Myringoplasty is considered an uncomplicated procedure. It is performed under local or general anesthesia and lasts an average of 40 minutes.
The operation begins with the creation of a flap to close the perforation. Surgical material can be used for this:
- Patient's own tissue from the area of the temporal fascia;
- a flap of elastic skin from the occipital region;
- a small piece of tissue from the inner thigh or upper arm;
- A transplant from the external ear canal, or pinna.
Depending on the location of the damage, the appropriate option is chosen to restore the eardrum as best as possible.
flap placement
The operated area can be accessed in two ways - through the ear canal or through a small incision behind the ear. This area is being prepared for replacement:
All surgical procedures are performed using a microscope and micro-instruments to avoid significant trauma to the tympanic cavity.
If the hole is close to the wall of the ear canal, the flap is placed as close to it as possible. The central defect is closed with new skin all around, but sometimes the central perforation is performed only marginally. Due to the large area of the bone, the transplant can be implanted better and faster. Finally, the graft is fixed.
indications
Puncture of the tympanic membrane is indicated in the following cases

- severe pain syndrome with confirmed otitis media;
- Fluid in the middle ear detected by a special examination: tympanometry;
- no positive response to long-term treatment with antibiotics and other drugs;
- Dysfunction of the Eustachian tube in adults;
- Hearing problems due to fluid accumulation in the tympanic cavity;
- the need for investigations to determine the causative agent of possible infection and allow appropriate drug therapy.
If the effusion from the middle ear cavity is removed in a timely manner, without waiting for complications, then otitis media will not develop into a chronic disease.
Important!!! Myringotomy of the tympanic membrane does not replace antibiotic therapy, does not reduce the frequency of otitis media, and does not reduce the number of recurrences.
contraindications
A myringotomy may be contraindicated if there is evidence of a middle ear tumor or vascular anomaly. A relative contraindication is previous radiation therapy in the head and neck area.
The ENT doctor decides on the method of the operation on the basis of a comprehensive examination of the patient, a confirmed diagnosis and the presence of indications for an intervention.
A microscope is used to obtain the best possible view of the middle ear cavity. A small incision is then made in the eardrum and the fluid is removed from the middle ear. In most cases, a small tube may be required to remain at the incision site and allow for continued drainage.
No sutures are needed to close the incision—it will heal on its own.
expert opinion
As a doctor who regularly deals with this pathology in patients, I would like to note that in case of perforation of the eardrum, it is of paramount importance to seek timely treatment from an otolaryngologist and follow the recommendations of the specialist. Responsible approach to one's own health will speed up the duration of treatment, facilitate the rehabilitation period and minimize the possibility of a gross scar on the membrane and associated irreversible hearing loss.
Ophthalmologist of the highest category, microsurgeon, candidate of medical sciences, professor, head of the department of ophthalmology at the 'SM Clinic' on Jaroslavska Street.

Treatment of perforation of an eardrum
To eliminate the cause of the purulent otitis media that caused the perforation, or to prevent infection in case of mechanical damage to the eardrum, antibiotic therapy is recommended. Antibacterial and anti-inflammatory topical drops can speed up the healing process.
If the hole is small, the membrane will heal on its own within a few weeks. For larger holes, an ENT doctor can help repair the perforation.
If conservative methods are not enough, the patient undergoes surgery to close the eardrum - myringoplasty.
During this operation, the patient is put to sleep (anesthesia) or given a local anaesthetic. The ENT surgeon uses a piece of skin from the auditory canal or cartilage from the area above the ear as plastic material. With the help of an endoscope (a thin tube with optical illumination), the doctor places this flap on the damaged area and reinforces it with special materials that dissolve during the transplant. At the end of the operation, the specialist inserts an antibiotic tampon into the patient's ear canal to prevent the infection from spreading and to promote healing of the damage as quickly as possible.

class of reptiles
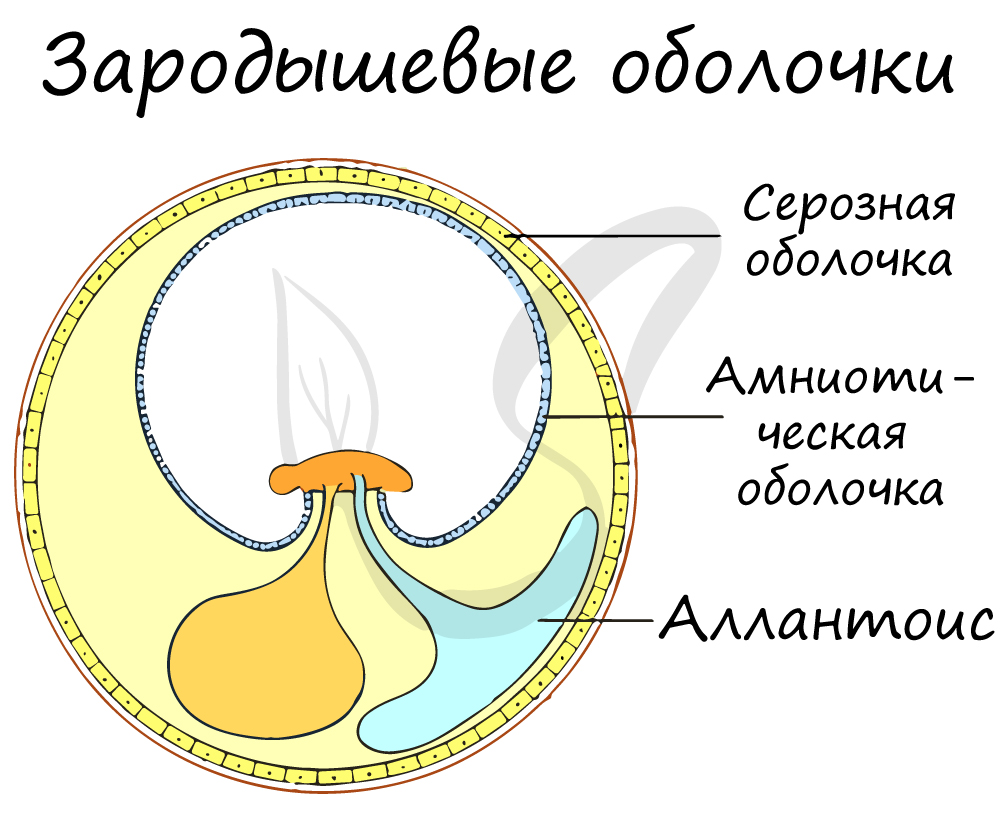
Reptiles are a class of terrestrial vertebrates that no longer depend (like amphibians) on water for reproduction and development. They belong to the amniotes. Reptiles peaked in the Mesozoic.
Today this class counts about 10 000 species.

The reptiles evolved from the ancient armored amphibians, the stegocephala, which could protect their bodies from drying out and were able to colonize areas away from water bodies.

The reptiles struggled to become independent of water, for which their bodies evolved a number of advanced features called aromorphoses:
As already mentioned, reptiles are amniotes. This means that the development of their embryos takes place in a special fetal sac containing amniotic fluid - the amniote. Astonishing!!! You no longer need a reservoir, this reservoir is always with you, right in the woman's body around the embryo.
The fetal membranes include the outer serous membrane (serosa), the inner amniotic membrane, and the allantois. The allantois is the organ of the embryo through which respiration occurs. Thanks to these membranes, the reptiles were able to spread from the water to the interior of the continents and colonize large areas.
In fish and amphibians, fertilization was external and inefficient due to the small chance of gametes meeting. In internal fertilization, as occurs in reptiles, the male's semen containing sperm is injected directly into the female's reproductive tract, greatly increasing the likelihood of male and female germ cells meeting.

Causes and clinical features
Causes leading to an eardrum rupture include otitis media (acute or chronic suppuration), aerotitis, direct trauma (direct injury), chemical or noise trauma (acoustic trauma), and skull base fracture.
otitis media
Perforation of the tympanic membrane occurs in the second phase of acute otitis media. In patients with severe ear pain and fever, pus collects in the eardrum cavity, causing the eardrum to rupture. Immediately after the rupture, patients notice an improvement in mood, a decrease in ear pain, and a drop in temperature. A characteristic feature of acute perforating otitis media is the pus that flows from the ear, despite the relief.
Prolonged chronic mesotympanitis and epitympanitis also lead to eardrum rupture, which is difficult to treat conservatively and is associated with permanent hearing loss and frequent dizziness.
Aerotitis (aerogenic perforation)
Aerotitis is caused by a sudden drop in air pressure, which usually occurs during takeoff or landing. The sudden drop in pressure on the eardrum will deform or rupture the eardrum only if there is concurrent obstruction of the Eustachian tube.
Eardrum rupture in aero-otitis is accompanied by constipation, pain, tinnitus, dizziness and hearing loss. After the rupture, a bloody discharge comes out of the affected ear.
Direct membrane damage

Direct mechanical damage to the eardrum often occurs at home. It can rupture when objects used to clean earwax (matches, cotton wool, hair clips) go deep into the ear canal or when foreign objects are pushed into the ear canal when trying to remove them yourself. They are always accompanied by acute pain and bloody discharge from the external auditory canal.
diagnosis of a rupture
A ruptured eardrum is easily diagnosed with an otoscopy, a diagnostic, noninvasive examination of the ear canal. If the eardrum is ruptured, otoscopy examines the ear canal, the eardrum itself, and, in some cases, the structures of the middle ear. It is performed using ear specula and a front reflector, or a modern otoscope that combines an ear specula, a light source, and a magnifying glass.
In order for the eardrum to be accessible for the examination, the auditory canal must first be cleaned of earwax, dirt, blood, secretions or foreign bodies. For otoscopy:
- Increased vascularization in minor trauma;
- bleeding in the membrane in case of acoustic trauma;
- visible cavities in case of severe trauma;
- A fracture with irregular edges, as well as the inner wall of the tympanic cavity;
- Hematoma in the tympanic cavity.
In addition to otoscopy, the following additional examinations are carried out if an eardrum perforation is suspected or detected: stabilization, vestibular nerve, audiometry, caloric examination, acoustic impedance measurement, electrocochlearography and ventricular examination. These diagnostic methods are used to determine the extent of damage to the structures in the tympanic cavity and to assess the degree of hearing loss.
Causes of Carpal Tunnel Syndrome
The median nerve in the hand passes through a tunnel formed by the transverse ligament and carpal bones of the hand. Compression of the nerve in this tunnel can be caused by:
- Traumatic hand injuries. Contusions, dislocations, and fractures can cause swelling of the ligaments and muscles, and even dislocation of the bones in the wrist. All of this can compress the nerve in the canal, leading to impaired function. With proper treatment, all of these processes are reversible, but if not treated in a timely and correct manner, muscle and ligament contractures and bone deformities can be irreversible.
- Osteoarthritis, arthritis and other pathological joint processes of different etiology and origin. Swelling and inflammatory reactions, including tissue necrosis, caused by these pathologies can also cause nerve compression. If the inflammation persists and degenerative and dystrophic processes progress, the articular surfaces of the wrist lose their properties and wear out, which leads to deformation and compression of the nerve in the canal by bony structures.
- Tendonitis or tendovaginitis. Inflammation can be septic (caused by microorganisms) or aseptic (caused by stress, hypothermia, etc.). Septic inflammation can B. caused by purulent wounds on the hand, including armored lesions, improper finger blood sampling technique, etc. Non-infectious inflammation can be caused by chronic traumatic stress, such as B. frequent monotonous hand movements, static loads on the hand, temperature trauma.
- Diseases that cause water retention in the bodyDiseases that cause water retention in the body can cause swelling in the limbs, leading to soft tissue swelling and compression of the median nerve. A disturbed water-electrolyte balance can be caused by: pregnancy, taking hormonal contraceptives, menopause, kidney disease, etc.
- Rare but not uncommon. Tumors of the nervous tissue and median nerve In particular, tumors of the nerve tissue of the metacarpal bone and the median nerve. These are mostly benign tumors (schwannoma, neurofibroma, perineuroma), but malignant ones originating from nerve sheaths can also occur. The tumor grows and presses on the nerve, damaging it.
- diabetes mellitus. During the course of the disease, the enzyme protein kinase C begins to break down sorbitol and fructose stored in the nerve tissue. There can be aseptic inflammation of the nerves and their surroundings, as well as impairment of the trophicity of the neurons and their progenitors. Swelling develops, which in turn compresses nerves, including the median nerve.
- acromegaly. As a result of prolonged and intense growth, a person with acromegaly develops disproportionate hypertrophy of bones and soft tissues. The median nerve can be compressed in the carpal tunnel due to increased bone volume and narrowing of its lumen.
- Congenital anomalies. The transverse carpal ligament may be thick from birth and tendon fat production is also deficient. A predisposing factor for carpal tunnel syndrome may be an anatomical feature of the wrist, known as the 'angular wrist'.
Symptoms of Carpal Tunnel Syndrome
A numbness in the fingers. The syndrome in question usually occurs gradually and usually only on one side. The pathological process usually starts from the dominant limb, that is, from the right hand in right-handed people and from the left hand in left-handed people. The development of carpal tunnel syndrome is insidious. However, a two-way process can also occur, e.g. B. in endocrine diseases or during pregnancy.
paresthesias. They express themselves as tingling and loss of feeling in the fingers. They appear in the morning after waking up and subside within a few hours. However, over time these symptoms become more persistent and intense and can become permanent. Normal limb functions such as strength, dexterity, etc. may be impaired and the affected limb may need to be rested by changing hands during the activity. Manipulations that require static limb tension can cause discomfort.
Pains. At the manifestation of the disease there may be a burning or tingling sensation, which is relieved by pulling down and shaking the limb. The blood flow to the arm increases again and the pain subsides. Most often, the pain occurs during sleep, when the arm is in a static position or during monotonous work with the limb. The pain is not specific to any particular joint but is widespread. As the disease progresses, the pain can affect not just the fingers, but the entire hand and arm up to the elbow joint, which often complicates the diagnosis. The patient is unable to perform his duties as the pain can appear throughout the day.
loss of dexterity and strength. If left untreated, the limb loses strength and dexterity in movement over time. The patient has difficulty holding objects, especially small objects that seem to fall out on their own. Fine motor skills (grasping small objects, opposable thumb, etc.) are impaired.
prevention
To prevent otitis media, a number of recommendations should be followed:
- If the child has a cold, use nasal drops with a vasoconstrictive effect (as recommended by the doctor).
- Vaccination against certain pathogens such as pneumococci and influenza can prevent some infections.
- Timely and proper elimination of accumulated mucus in the nasal passages.
Acute otitis media in children is one of the most common diseases. Frequent or neglected middle ear infections pose a risk to hearing and speech. It should be treated in time by a doctor.
Benefits of treating otitis media at Rebenok Clinic
The clinic is staffed by doctors who have extensive practical experience. Specialists use modern diagnostic equipment and prescribe effective treatment of otitis media in children, taking into account the age and condition of the patient. If necessary, you can call the doctor at home or use the 'Online Consultation' service.
- Boikova NE, Rybalkin SV. Acute otitis media in children: standards of care. [Electronic resource].
- Ustinovich AA, Ustinovich KN Peculiarities of clinical manifestations of acute otitis media in children in the first months of life. [Electronic resource].
We react immediately to additions and changes to the price list. In order to avoid misunderstandings, we recommend specifying the full list of services and their cost when registering at the clinic or by calling 8-495-104-35-35.
The price list on the website does not constitute an offer. Medical services are provided on the basis of a signed contract.
- hole in the eardrum.
- Membrana interossea tibiae in Latin.
- Gum disease on feet.
- Earplugs to buy.
- pain in the elbow joint.
- Child walking with clubfoot aged 2 years.
- sphenoid sinusitis.
- structure of the toes.
