The effectiveness was examined in all patients included in the study. The onset of effect was observed on day 23 in the majority of patients, the earliest onset on day 20 and the latest onset on day 34 were observed in 25 % subjects.

- Study on the effectiveness, tolerability and safety of hyaluronic acid in patients with knee osteoarthritis
- Material and methods.
- Treatment of aseptic necrosis of the knee 1.jpg
- Treatment of aseptic necrosis of the knee 2.jpg
- Radiological diagnostics
- Conservative treatment
- Diagnosis of fractures of the femoral condyle and tibia
- Treatment of femur and tibial condyle fractures
- Diagnosis of tibia fractures
- Treatment of tibia fractures
- This might be of interest
- User questions about tibia fracture
- Treatment of meniscus injuries and tears
- Recovery after meniscus surgery
- Treatment of intra-articular fractures
- surgical treatment
- Medical therapy
- prevention
- diagnosis
- Treatment
- Restriction of physical activity and therapeutic exercises
Study on the effectiveness, tolerability and safety of hyaluronic acid in patients with knee osteoarthritis
C. Anikin, MD, PhD
Л. D., PhD
E. M. Zaitseva, MD
Н. G. Kashevarova
T. A. Korotkova, MD
E. TA Korotkova, MD, Candidate of Medical Sciences
VA Nasonova NIIR, Moscow
Osteoarthritis (OA) is a joint disease characterized by cellular stress and degradation of the extracellular matrix resulting from macro- and micro-damage, activating abnormal adaptive repair processes, including pro-inflammatory immune system responses, bone remodeling, and osteophyte formation [1]. OA is one of the most common musculoskeletal disorders. Overall, the prevalence of knee OA in people aged 55 years and over is 10 %, with 25 % of OA cases presenting with frequent exacerbations and severe clinical symptoms [2]. The main symptoms of OA are pain, mainly mechanical, with startle, short-term stiffness lasting up to 30 minutes, and joint dysfunction. The clinical picture may be accompanied by crepitus during active movement, mild effusions and bony hypertrophy. A comprehensive approach is taken to treat OA, using both drug and non-drug treatments: physiotherapy, exercise therapy and other rehabilitation methods. In the case of persistent OA, which is associated with severe pain symptoms, severe functional limitations and a significant reduction in quality of life, surgical treatment is carried out. OA is a chronic disease that requires long-term therapy. The majority of patients with primary OA are elderly and usually have multiple comorbidities. The most recent 2014 Osteoarthritis Research Society International (OARSI) guidelines for non-surgical treatment of knee OA focus on the issue of comorbidity [3]. The organization's expert panel evaluated each method not only for its effectiveness, but also for the risk of adverse events. Based on the decisions of the expert panel, conclusions were drawn about the validity of a particular therapeutic approach. Nonsteroidal anti-inflammatory drugs (NSAIDs) and intra-articular glucocorticoids are used to treat pain in OA. These therapies can significantly reduce pain and improve function. However, their use may be limited by coexisting gastrointestinal, cardiovascular, renal, hepatic, endocrine and other diseases. When treating with NSAIDs and glucocorticoids for intra-articular injections, possible impairment of the function of internal organs should be taken into account, and the duration of such therapy should be short, using the lowest effective doses of drugs [3, 4]. Another group of medications commonly used in the treatment of OA are slow-onset symptom medications (SARPs). Their role and significance in the treatment of OA remains controversial to this day. This is due to the great heterogeneity of the data obtained in different clinical studies. In general, it can be stated that PMREs are characterized by a moderate symptomatic effect and good tolerability. Almost all studies reported a very low incidence of adverse drug reactions, which were generally not clinically significant. Due to these characteristics, PMREs can be widely used in patients with high levels of comorbidity and in different age groups.
Material and methods.
A one-year prospective cohort study included 30 patients with a diagnosis of primary knee OA, of whom 93 were % female and 7 were % male. OA was diagnosed according to the 1986 American College of Rheumatology (ACR) classification criteria. [4].
Inclusion criteria: Men and women aged 45-70 years, diagnosis of primary tibiofemoral OA confirmed according to the American College of Rheumatology criteria, pain when walking with an intensity of at least 40 mm on a visual analogue scale (VAS), second or third radiographic Kellgren-Lawrence stage, requirement of at least 30 days of NSAID therapy in the previous three months, and signed informed consent.
Exclusion criteria: Patients with known secondary gonarthrosis, patients treated with other symptomatic agents and slow-acting drugs in the last six months, intra-articular administration of other drugs in the last six weeks before inclusion in the study, cases of chondrocalcinosis, aseptic necrosis of the femur - and tibial condyles, knee operations and patients with hypersensitivity to GnA and severe comorbidities, including systemic rheumatic diseases.
The use of NSAIDs that patients were taking at the time of study enrollment was permitted. Other intra-articular injections, including glucocorticoids and other GnA preparations, as well as physiotherapy treatments were not permitted.
Treatment of aseptic necrosis of the knee 1.jpg

Treatment of aseptic necrosis of the knee 1.jpg
Aseptic necrosis of the knee is treated conservatively or surgically.
Conservative treatment is considered successful if the lesion does not occupy more than 40 % of the width of the condyle. MRI is considered the most effective non-invasive method for assessing the extent of osteonecrosis. Carrying out the procedure using STIR makes it possible to assess the actual extent of swelling, the extent of necrosis and the prognosis of the course of the disease.
- Dismissal of the limb;
- nonsteroidal anti-inflammatory drugs;
- shockwave therapy;
- Knee closure to relieve pain;
- platelet-rich plasma therapy;
- Injection of mesenchymal stem cells from fatty tissue into the knee.
The specialists in the clinic of Dr. Glatskov prefer conservative treatment methods. In many cases, bone necrosis stops and the tissue regenerates, allowing the affected person to relieve pain and return to their previous physical activity.
Treatment of aseptic necrosis of the knee 2.jpg

Treatment of aseptic necrosis of the knee joint 2.jpg
Aseptic necrosis of the thigh tissue in the knee joint requires surgical treatment in the following cases.
- There is a tear in the meniscus;
- in the advanced stage of the disease, when more than 40 % of the width of the condyle have died;
- Conservative therapy is ineffective and the disease progresses.
Most operations in Dr. Glazkov are performed using arthroscopic methods. These are minimally invasive procedures that are carried out through punctures in the knee area, without large incisions and without opening the joint cavity. After these procedures, the affected person recovers more quickly, is less prone to complications and spends less time in the hospital.
Operation of aseptic necrosis of the femoral condyle:
Debridement with microsurgical procedure. The doctor crushes the damaged tissue and creates small lesions in the bone area. These stimulate regenerative processes, stop tissue death and promote healing.
Decompression. A surgery that creates one or more channels in the bone to reduce internal pressure. After this procedure, new blood vessels are formed, which improve the blood supply to the bone tissue.
Osteochondroplasty. Used to replace defects in bone and cartilage tissue. These are taken from other areas of the body. Artificial materials are also used less frequently.
Osteotomy. Removal of a dead piece of bone.
Single condylar endoprosthesis. It is used in the most severe cases. Doctors replace part of the knee joint with an artificial prosthesis.
If you have osteonecrosis of the knee, contact our medical center. We use innovative cell therapies, perform minimally invasive operations and, in most cases, can cure the disease without an endoprosthesis.
Radiological diagnostics
X-rays. X-rays provide images of dense anatomical structures, including bones. Bone changes that occur in the later stages of osteonecrosis can be detected with this examination. In the early stages of the disease, there are usually no changes visible on x-rays.

This x-ray shows signs of osteonecrosis of the inner femoral condyle.

As the disease progresses, the joint stroma narrows due to damage to the articular cartilage.
Magnetic resonance imaging (MRI). Early bone lesions that may not be visible on x-rays are often discovered using MRI. This examination can be used to assess how severely the bone is affected. MRI can also detect lesions that do not yet show symptoms (e.g. osteonecrosis of the opposite knee joint).
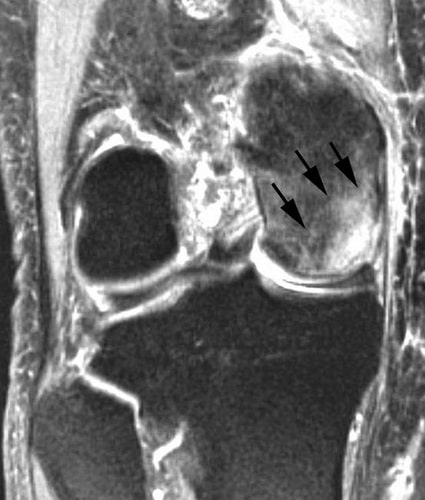
MRI can also detect lesions that do not yet have symptoms (e.g., osteonecrosis of the inner femoral condyle). MRI is often used for the early diagnosis of this disease.
bone scintigraphy. In some cases, patients are prescribed skeletal scintigraphy. During this test, a small amount of a radioactive drug is injected into a vein. Osteonecrosis can be characterized by an increased accumulation of radioactive material in the bone, which is due to increased metabolic activity in this area.
The treatment strategy for aseptic necrosis of the knee joint depends on several factors:
There are four stages of osteonecrosis of the knee joint.
Stages 1 and 2 – the swelling of the bone is clearly visible on magnetic resonance imaging (MRI) after 6 to 12 weeks. At this stage there is still hope for healing.
Conservative treatment
In the early stages of the disease, conservative treatment is indicated. If only a small part of the bone is affected, this treatment is sufficient.
- Pharmacological treatment. Taking nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen helps control pain and inflammation in the knee joint. Supplementing your treatment with cartilage protectants and vitamins will enhance the healing effect.
- Reducing the burden. In some cases, limiting weight bearing on the affected limb can slow the progression of joint damage caused by osteonecrosis and allow healing. Your doctor may recommend that you use crutches for a period of time to take pressure off the affected knee joint. In some cases, you can wear a weight-relieving brace to shift the load from the affected part of the knee joint to the healthy part.
- therapeutic exercises. Your doctor or physical therapist will create a specific exercise program to help you strengthen your hip muscles and maintain mobility in the affected knee joint. In some cases, swimming exercises may be recommended to avoid overloading the knee joint.
- Change in activity. The doctor may recommend avoiding certain physical activities that cause or worsen pain symptoms.
With correct and timely treatment in the early stages of the disease, very good clinical results can be achieved.
When conservative treatment is ineffective, patients are usually recommended minimally invasive arthroscopic surgery.
Diagnosis of fractures of the femoral condyle and tibia
Examination reveals varus or valgus deformity of the knee joint. It is enlarged and its contours are smoothed. Palpation reveals tenderness at the site of injury, sometimes crepitus, and the presence of an effusion (hemarthrosis) in the knee joint, characterized by oscillation and ballooning of the kneecap. Positive axial load sign. Passive movements in the knee joint are painful and may be accompanied by a grinding sensation.
Laboratory and instrumental investigations
X-ray images in two projections clarify the diagnosis.
[4], [5], [6]
Treatment of femur and tibial condyle fractures
Conservative treatment of fractures of the femur and tibial condyles
For fractures without dislocation, the knee joint is punctured, the hematoma is removed and 20 ml of a 2%igen procaine solution is injected. A circular plaster cast is applied to the limb stretched at the knee at an angle of 5° from the upper third of the thigh to the fingertips. With fractures of a single femoral or tibial condyle, the fixation of the limb is carried out with additional hypercorrection - inclination of the tibia on the fractured inner condyle outwards and vice versa, that is, to the healthy side.
Fractures of a single femoral condyle or fractures of the tibia with displacement are treated conservatively. Hemarthroses are treated. A 2 %ige procaine solution (20 ml) is injected into the joint cavity and the lower extremity is rotated as far as possible to the side opposite the fractured condyle. The fingers are used to try to press the fracture against the material bed. The manipulation is carried out with the limb stretched. The position achieved is secured in a functionally favorable position with a circular plaster cast from the groin fold to the fingertips.
The duration of immobilization for fractures of a femoral condyle is 4-6 weeks. The splint is then replaced with a movable splint and rehabilitation treatment is initiated, whereby the leg must not be put under any strain. After 8-10 weeks, immobilization is removed and, after radiological control, the careful use of crutches is allowed, gradually increasing the load. Walking freely is only possible after 4-5 months at the earliest. The ability to work is restored after 18-20 weeks.
The treatment tactics for fractures of the tibial condyle are the same. The duration of permanent immobilization is 4-6 weeks, removable immobilization is 8 weeks. The ability to work is given after 14-20 weeks.
In case of fractures of both condyles with displacement of the fragments, alignment is achieved by pulling the axis of the limb and compressing the condyles laterally with the hands or special devices (vise). The limb is fixed with a circular bandage. If repositioning is ineffective, skeletal traction is performed behind the heel bone with a load of 7-9 kg. After 1-2 days, a radiological examination is carried out. During this time, the fractures fuse in length, but sometimes there is a shift in width. The fracture is repaired by lateral compression of the fracture and a plaster cast is applied from the upper third of the thigh to the foot without breaking the traction. The limb is placed in a splint and traction on the skeleton continues. It should be noted that traction, repositioning and cast immobilization is carried out with extension of the limbs at an angle of 175 °. Body weight is gradually reduced to 4-5 kg. Traction and permanent immobilization are removed after 8 weeks, then rehabilitation treatment begins. A mobility splint is indicated after 8-10 weeks for femoral condyle fractures and after 6 weeks for tibial condyle fractures. In patients with fractures of both femoral or tibial condyles, return to function occurs after 18-20 weeks.
Diagnosis of tibia fractures
Diagnosis of tibia fractures is primarily based on x-rays. In our center for traumatology and orthopedics, computed tomography with three-dimensional image reconstruction is often used in addition to X-ray images. Modern methods of diagnosing bone fractures allow us to determine the correct treatment tactics.
 X-ray image of a tibia fracture X-ray image of a tibia fracture |  3D reconstruction of the fracture 3D reconstruction of the fracture |
Treatment of tibia fractures

Current treatment of tibia fracturesFractures of the shinbone are usually treated surgically. This is due to the anatomical features of the shinbone, shin usually superficial (not covered by muscle on the medial surface), often resulting in secondary perforation of the skin by bone fragments. Helps to immobilize the fragments Tibia fractures Skeletal traction of the heel bone is used in hospitals. This method is used for preoperative preparation and improvement of the skin on the injured shinbone.
Our trauma surgeons and orthopedists use the latest methods for the conservative and surgical treatment of tibia fractures. With the latest methods of osteosynthesis and intramedullary osteosynthesis accelerates the recovery and rehabilitation time of patients with tibia fractures.. As a rule, the patient can put weight on the injured leg the day after the operation. The early use of osteosynthesis in intra-articular fractures enables in most cases the most exact reconstruction of the articular surfaces, so that the risk of early osteoarthritis of the injured joint can be excluded.
This might be of interest
User questions about tibia fracture
The doctor's answer:
You know that this information is not enough. You can come to our center for a consultation.
Doctor's answer:
The delay in surgery is most likely due to the presence of soft tissue swelling in the area of the fracture. You should continue to contact your doctor.
Doctor's answer:
We recommend that you contact your doctor. Do not self-medicate over the Internet.
Treatment of meniscus injuries and tears
The choice of treatment depends on the severity of the injury as well as the patient's level of sport and stress.
As a rule, conservative treatment of a meniscus injury is sufficient for minor injuries. Severe injuries often require surgical treatment.
Conservative treatment consists of temporarily reducing the load on the knee joint. Pain relief is achieved by injecting painkillers into the joint. If the joint is blocked, this will be treated under local anesthesia. If there is exudate or blood in the joint cavity, the joint must be punctured, the fluid removed and a bandage applied for 21 days. Once the bandage is removed, physical therapy and exercise therapy are recommended.
If the meniscus is inflamed, therapy includes the administration of anti-inflammatory and antibacterial drugs.
If the meniscus in the knee is torn, radical treatment is required in most cases.
There are several known methods of meniscus surgery:
- The meniscus is stitched and repaired;
- part of the meniscus is removed;
- total meniscectomy;
- Transplantation.

The main surgical method is arthroscopy, in which only 2 small incisions are made. Arthroscopy minimizes tissue damage and shortens rehabilitation time.
Recovery after meniscus surgery

The rehabilitation period depends on the type of procedure. It can take between 20 and 40 days. During the 4 to 7 days (sometimes up to a month) postoperative rehabilitation, it is necessary to use crutches. We then begin to restore the normal function of the joint and strengthen the muscles and ligaments.
Do not treat on your own!
Only your doctor can make a diagnosis and prescribe appropriate treatment. If you have any questions, you can call us or send us an email.
Treatment of intra-articular fractures
Purpose of treatment of intra-articular fractures The goal of treating an intra-articular fracture is to restore the anatomical structure and fully restore the stability of the joint. This treatment can be conservative or surgical.
surgical treatment
If there is no sprain, a plaster cast can be applied to immobilize the affected area, relieve pain and speed healing of the fracture.
For intra-articular fractures Intra-articular fractures with displacement are treated using the following techniques.
- Skeletal traction. Allows the injured joint to be immobilized and the fractures to remain in the same position. Once the primary callus has formed, it is replaced with a plaster or plastic cast.
- Surgical intervention (osteosynthesis). The operation consists of putting the fractures back together and fixing them with plates, screws and spokes.
In cases of severe trauma or when the above treatments are unsuccessful, endoprosthesis is performed, in which the damaged joint is replaced with an artificial one. This is most commonly done for intra-articular fractures of the tibia.
Medical therapy
It is based on the prescription and extensive use of the following medications:
- Analgesics: narcotics, non-steroidal anti-inflammatory drugs;
- Anticoagulants, platelet aggregation inhibitors to prevent blood clots
- antimicrobials (for open fractures) to prevent infectious complications;
- Chondroprotectants – medications needed to speed up the repair of bone and hyaline cartilage and prevent complications. They are characterized by high effectiveness with the simultaneous absence of contraindications and side effects.
The glucosamine-based chondroprotective drug Artracam has a pronounced restorative effect. It rebuilds damaged cartilage and joint tissue by inhibiting and preventing inflammation, and it is gently absorbed without causing significant side effects. Its supplementation helps accelerate the regeneration of deformed joints.
prevention
Prophylactic measures are aimed at preventing intra-articular bone fractures and include timely treatment of diseases that provoke them, normalization of body weight, prevention of household, street, industrial and sports injuries.
It is important to strengthen bones and joints. This requires a nutrient-rich diet and intake of dairy products, grains, fish and vegetable oils. In addition, physical activity should be maintained and coffee and salt consumption should be reduced.
To strengthen joints and prevent diseases, preventive treatment with chondroprotectors is recommended. A course of Arthrakam 1-2 times a year keeps joint, cartilage and bone tissue in a healthy condition and prevents thinning, brittleness and brittleness.
Intra-articular fractures require lengthy and complex treatment, including surgery. Any injury, even minor signs of joint damage, should be treated immediately.
diagnosis

Your doctor will order the following tests to confirm the diagnosis:

There are different types of tuberosity injuries. These include flattening or thinning of the tuberosity, curvature, one or more fractures and contusions, and significant growth of the epiphyseal process of the tibia.
In complicated cases, the doctor's recommendations require the ordering of additional examinations:
- general blood test;
- Rheumatoid factor test;
- C-reactive protein levels;
- PCR tests.
These examinations can be used to differentiate Schlatter disease from bone tuberculosis, osteitis, quadriceps epiphyseal fractures, and bone tumors.
Treatment

Schlatter's disease of the knee joint is chronic (1-2 years) and resolves spontaneously, and bone hypertrophy does not affect the further function of the knee.
However, if bone fragments are discovered, an effective and uncomplicated operation should be performed that will allow the patient to continue leading a physically active life. However, in most cases, treatment is conservative.
Restriction of physical activity and therapeutic exercises

Conservative treatment of Schlatter's disease primarily consists of significantly limiting the load on the affected knee, including completely refraining from physical activity and participation in physical education classes.
The painful joint is wrapped with an elastic bandage, a special vocal bandage or a soft elastic bandage. This support for the knee is not accidental. It prevents the quadriceps tendon from tearing from the epiphyseal tubercle of the tibia.
Teens shouldn't be happy, though, because exercise, no matter how small, is still necessary. A painful knee should undergo daily specific LFC exercises that include quadriceps and hamstring stretching.
Read more:For your information. Particular attention should be paid to swimming in the pool 2-3 times, alternating between slow and fast paces, with rest breaks. For more detailed instructions on a therapeutic swimming class plan for Schlatter's disease, contact your physical therapist or sports therapist.
- Inflammation of the tibial cortex.
- Injury of shin ligaments.
- External tibial condyle.
- Мыщелка берцовой.
- Injury to the navicular semilunar ligament.
- heel bone injury.
- Injury to the ankle.
- tibial ligaments.
