
- Knee Ligament Sprains and Strains Treatment: First Aid, Healing
- How is a diagnosis made?
- classification
- Treatment
- Causes of inflammation of the popliteal tendon
- How Does a Person With Popliteal Tendonitis Feel?
- diagnosis
- Treatment options for tendonitis in the knee
- How do you treat chronic calcific tendinitis?
- Main causes of injuries
- treatment and rehabilitation
- FEEDBACK FROM OUR PATIENTS
- The location of the injury and its initial symptoms
- Methodology for diagnosing dislocations
- Treatment of cruciate ligament injuries
- Types of sports injuries
- Diagnosis of sports knee injuries
- SURGICAL TREATMENT
- RESULTS OF SURGICAL TREATMENT
Knee Ligament Sprains and Strains Treatment: First Aid, Healing
In just 24-36 sessions, depending on the intensity of treatment and the stage of the disease, you will get rid of pain and grinding in the knee joint, increase its mobility and range of motion, and be able to live your life
When treating sprains and ruptures of the ligaments of the knee joint, it is necessary to select an individual set of therapeutic exercises, learn the technique of their implementation and exclude contraindicated exercises.
The most important thing for this symptom is regular attendance at therapy sessions, complete treatment in a specialized center and preventive health care on your own.
All videos with therapeutic exercises
Ligaments connect the bones of the lower leg and thigh, keeping them stable while walking, squatting, and twisting.
The ligaments can be torn or stretched by trauma or extreme stress.
How is a diagnosis made?
When you go to the doctor, he or she will most likely ask how the injury happened and provide a visual diagnosis of the knee joint.
- Persistent pain that cannot be felt;
- unusual cracking and grinding in the joint that causes pain with even small movements;
- Difficulty changing posture, limitation of knee mobility;
- tissue swelling;
- bruising that appears many hours after the injury;
- Abnormal lateral deviation of lower limbs with tear of collateral ligaments;
- Pathological mobility of the tibia bent at the knee in a cruciate ligament tear;
- Instability or stiffness of the joint, with the patient complaining that the knee is 'loose' or 'drops out' with movements.

To determine the location of the injury, the doctor will order an X-ray, ultrasound, or magnetic resonance imaging (MRI).
Additional diagnostics provide information about possible fractures or tissue damage in the knee.
classification
– Indirect mechanism (non-contact – failed landing after a jump, twisting of the leg when braking sharply).
II. DIAGNOSIS AND TREATMENT METHODS, APPROACHES AND PROCEDURES
– Blood chemistry: (determination of glucose, total bilirubin, alanine aminotransferase, aspartate aminotransferase, urea, creatinine, total protein);
Minimum list of examinations to be carried out upon admission to hospital:
– Magnetic resonance imaging of the knee joint (indications: torn, dislocated and damaged knee ligaments)
– Blood chemical tests: (determination of glucose, total bilirubin, alanine aminotransferase, aspartate aminotransferase, urea, creatinine, total protein)
– Collection of complaints and anamnesis, physical examination.
Complaints: Severe pain accompanied by swelling, a feeling of slackness and instability of the knee joint, limitation of range of motion.
anamneseOccurs more often with an indirect mechanism of injury (unsuccessful landing after a jump, twisting of the leg when braking suddenly). Rare – direct impact on the knee joint.
X-rays of the knee joint in 2 projectionsAbnormal convergence of the articular surfaces.
Treatment
Antibiotic therapy.
Antibacterial drugs are used for postoperative wound inflammation and to prevent postoperative inflammation. These include cefazolin or gentamicin if allergy to B-lactams is present, or vancomycin if methicillin-resistant Staphylococcus aureus is detected/at high risk. The Scottish Intercollegiate Guidelines and others strongly recommend antibiotic prophylaxis for this type of surgery (3,4,5). Changes in the antibiotic list for perioperative prophylaxis should be based on microbiological monitoring in the hospital.
Administration of NSAIDs for postoperative pain relief should be started intravenously 30-60 minutes before the expected end of surgery. Intramuscular administration of NSAIDs for postoperative pain relief is not advisable due to variability in serum concentration and pain caused by the injection [7], with the exception of ketorolac (intramuscular administration possible).
NSAIDs are contraindicated in patients with ulcerative lesions and a history of gastrointestinal bleeding. In this situation, the drug of choice would be paracetamol, which has no effect on the gastrointestinal mucosa.
Table 1. Medications used for shoulder joint dislocation (other than anesthetics)
Causes of inflammation of the popliteal tendon
Inflammation of the popliteal tendon is most often caused by overloading the supporting structures of the knee. It is caused by constant bending and straightening of the knee joint. The most common cause of the disease is overexertion during sports. However, tendinitis can also occur in people who do not exercise.
In orthopedics, a distinction is made between internal and external causes of tendinitis. External factors include:
- the constant wearing of uncomfortable footwear;
- Mistakes when exercising (walking too fast).
- Uncomfortable footwear; incorrect footwork (walking too fast).
The intrinsic factors for the development of knee tendonitis include age-related changes in the human body, loss of joint flexibility and mobility. This can also include flat feet and different leg lengths. All of these factors lead to uneven strain on the musculoskeletal system.
An increased Q-angle or femoral anteversion are two common types of misalignments that contribute to knee tendonitis. The Q angle is the angle that the patellar tendon makes with the extension axis of the quadriceps muscle. It is different for men and women. It is usually larger in the weaker sex. The normal value is less than 15 degrees. If it is exceeded, the tendon is put under a lot of strain, which can lead to painful inflammation. The twisting of the thigh affects the position of the kneecap. Any imbalance in the structure of the lower limbs directly affects the joint.
The strength of a tendon depends on the number, size and orientation of the collagen fibers that compose it. When this structure is overstretched, a discrepancy occurs between the load and the tendon's ability to distribute the force. Such a discrepancy can lead to injury.
How Does a Person With Popliteal Tendonitis Feel?
The first inconvenience in the development of the disease is pain syndrome. These occur in the lower part of the kneecap and increase during physical activity. The tissue at the site of the injury swells, warmth is felt and the skin becomes hypersensitive.
diagnosis
In the clinic, diagnosis begins with the doctor taking the patient's medical history. A physical examination will be performed. The doctor asks questions about your health, symptoms, lifestyle and hereditary factors. The doctor will always ask when the pain started, at what times it gets worse and what helps to relieve the symptoms.
The examination includes palpation of the painful area and simple exercises (squatting, walking). The strength and length of the muscles and structures surrounding the knee (quadriceps, tendons, calves, hip flexors, and glutes) are checked. The physical examination is often enough to make a diagnosis. However, additional diagnostic tests are sometimes performed:
- Ultrasound – an ultrasound examination using sound waves.
- X-ray examination – examining the painful area with gamma rays.
- MRI – magnetic resonance imaging, a painless and safe X-ray examination of the body's internal structures.
Blood and urine tests may be ordered to check for signs of inflammation.
Treatment options for tendonitis in the knee
The use of nonsteroidal anti-inflammatory drugs (NSAIDs) is controversial in both the acute and chronic phases. Many studies have shown that these medications interfere with soft tissue healing. Although they reduce pain and relieve swelling in the knee area, they have a negative effect on tendon repair.
Corticosteroids are also used to relieve pain and reduce swelling. Surgical intervention only makes sense if conservative treatments for knee tendonitis have failed.
How do you treat chronic calcific tendinitis?
First of all, negative influencing factors are excluded, an accurate diagnosis is made and the form of the disease and the degree of deviation from the norm are determined. Calcific tendinitis is a serious condition in which calcium salts build up in the tendon fibers. Their location can be identified using X-ray findings. These deposits block the elasticity of the tendon.
Main causes of injuries
- Injuries (sports or direct trauma to the knee joint: fall, jump, blow, etc.).
- Ligament weakness caused by: tendonitis (patellar ligamentitis), chronic diseases (diabetes, rheumatoid arthritis, infectious diseases, etc.), taking steroid hormones
- Numerous microtraumas to the ligament
- Previous knee surgery
- Cracking and jumping in the joint with severe pain in the kneecap area
- Bleeding and swelling in the front thigh area
- Displacement of the kneecap upwards towards the femur
- muscle cramps
- 'Sinking' of the knee when walking
- Increased sensitivity in the knee joint area
- Inability to bend the knee
treatment and rehabilitation
If the patellar ligament is only partially damaged, conservative treatment can be performed by numbing the injury site with a plaster cast. Once the cast is removed, physical therapy, mud baths, and other treatments are recommended to restore mobility. In most cases, the kneecap ligament is torn and surgery is required. During the operation, the torn ligament is sewn with stitches through holes in the bone at the tip of the kneecap. After the operation, the patient is given pain medication and the limb is immobilized with a splint or cast (if immobilized). The patient can also be moved with the help of crutches. After a certain period of time, the splint or cast is removed and the patient receives a course of treatment for improvement: therapeutic exercises, laser therapy, massage, ultrasound, etc.
For expert medical care, you can contact the NCC2 (Central Clinical Hospital of the Russian Academy of Sciences) in Moscow.
FEEDBACK FROM OUR PATIENTS
Thank you for helping me with my TMJ problems. Even my dentist could tell a difference after a few sessions! FEBRUARY 11, 2020.
The doctors at the clinic helped me get my life back together after a car accident. It didn't seem like a big deal, but the injury I sustained, although it didn't require surgery, seriously ruined my life as I had headaches even in my sleep, I think. I'm glad to be clairvoyant again. Thank you, Valentin Sklyarov August 28, 2019.
Wonderful place where doctors take care of patients. Excellent specialists in physiotherapy practice. Soulful trainers in the MTT room. They became a family within two months of treatment. Thank you for your help and recovery from a very difficult injury. Zoya Viktorna July 22, 2019.
Many thanks to Sergei Viktorovich and Vera Petrovna that I can now walk without pain! What a joy it is to live life to the fullest, move and own my body! Health and happiness and good luck to the clinic! Igor Timofeevich July 17, 2019.
Vitaly Vladimirovich and Sergey Viktorovich literally brought me to my feet. I came to the clinic with a limp and a blank stare - my leg had been in pain for a month and a half. It turned out to be a large hernia in the lumbar spine (1 cm). After a visit to Sergiusz Wiktorowicz, I received an anti-inflammatory and pain-relieving drip and physiotherapy in the clinic on the same day. And immediately I wanted to continue living; there was an incentive to heal and move. During the treatment I got to know the doctors better, they are not only great professionals but also very interesting people. Thank you for all your help! Ivan Sergeyevich July 5, 2019.
Reputable clinic with competent doctors. Helped me get rid of the headaches I suffered from for several years. I always recommend this clinic to my friends and I have never had to be ashamed of it. Feedback from yell.ru Mikhail V. July 4, 2019.
Hello. I am 55 years old, I lead a sedentary lifestyle, at the age of 50 sitting was already very difficult and painful, pillows and belts did not help. When I was 52, I started going to different doctors and clinics. The pain temporarily subsided, but came back quite quickly. In the clinic of Dr. I finally got rid of Grigorenko. And unfortunately I didn't find it again until I was 54, with virtually no help for two years. The doctors are exceptional and competent, I recommend them. Sound Health! Sergius June 26, 2019.
The location of the injury and its initial symptoms

If the reaction is timely, a dislocation does not promise any complications and does not require serious intervention. However, leaving a leg injury untreated is not an option. Particularly in children, a dislocation can be associated with an injury to the growth plate in the formative and active growth phase of the skeleton.
Depending on their location, sprains are divided into four types:
The name of the ligaments already indicates that they are connecting elements that connect the muscle to the bone and the joint. A ligament injury usually occurs when the leg is twisted to one side. In this case, the symptoms are usually acute and immediate:
Methodology for diagnosing dislocations
A qualified trauma surgeon can diagnose a sprain based on these symptoms. However, the diagnosis cannot be limited to an objective examination of the leg:
- To rule out the risk of a tear or fracture, an X-ray examination of the leg is essential;
- An ultrasound scan of the damaged joint may be necessary to determine the extent of the dislocation;
- Sometimes an MRI scan is done (if treatment of the leg has been delayed and pain persists, the ligaments should be checked for torn nerve fibers).
The severity of the sprain is divided into 3 levels. At the first stage, pain is an important indicator as there may be no bruising, swelling or other signs. Grade 2 is characterized by limited mobility and visible signs of ligament strain. At grade 3, invasive surgery is possible (if there is a bone or fragment fracture).
Treatment of cruciate ligament injuries
Surgical treatment of cruciate ligament injuries is required only in the event of a complete rupture of the fiber with chronic instability of the articular bone. The operation is performed abdominally or endoscopically five to six weeks after the injury. The injured area is reconstructed. Either your own or synthetic fabric can be used.
Conservative treatment of non-intuitive cruciate ligament injuries involves a puncture to remove accumulated blood from inside the capsule. A supporting bandage is then applied for several weeks. In severe cases, a plaster cast is applied. Active rehabilitation begins after 5-6 weeks.
When treating anterior cruciate ligament injuries, rehabilitation is the main focus. With the help of these techniques, it is possible to restore the integrity of the ligament and regain the ability to play sports and lead an active life.
In our chiropractic clinic, rehabilitation is carried out on an individual basis. Depending on the type and complexity of the injury, the doctor will create an individual treatment plan. This can include kinesiotherapy, physiotherapy, massage, osteopathy, physical therapy, laser therapy, acupuncture and much more.
If you need rehabilitation after a cruciate ligament injury, schedule a free initial appointment with an orthopedist at our chiropractic clinic. During your visit, the doctor will review your medical records and talk to you about the prospects and possibilities of using these techniques for your injury.
Doctor of medicine, chief physician of the clinic
Types of sports injuries
The flexible knee joint plays a key role in human movement. It helps distribute the load across different muscle groups and joints and acts as a shock absorber for the entire musculoskeletal system. Therefore, the knee is at greater risk of injury during increased physical exertion than any other complex joint. The most sensitive parts of the knee are considered to be:
The soft tissues around the knee joint are susceptible to bruises, tears, and other injuries resulting from an active lifestyle. These can be caused by a dynamic impact on the joint (shock or fall) or excessive physical stress.
Sports medicine experts note that training with high dynamic forces should be monitored by experienced doctors who calculate the risk of injury. Ligament and meniscus injuries occur when there are no techniques to gently increase the load during exercise. This problem is particularly acute among athletes in athletics and endurance sports. A particularly hard training cycle or sporting stress as punishment leads to particularly serious knee injuries and long recovery times.
In the event of a knee injury or severe pain in the knee joint area, it is important to provide the injured athlete with first aid quickly. This consists of cold radiation and immobilization of the joint with a knee cap made of special fabric or a simple elastic bandage. All other medical measures must be avoided until a medical examination has been carried out.
Without a complete MRI scan of the knee joint or an X-ray, it is not possible to properly assess the extent and nature of the injury and recommend the correct treatment. All injuries to the knee joint can be divided into several groups:
With inadequate treatment or severe trauma, a dangerous pathology can develop: inflammation of the joint capsule. This is practically a death sentence for the damaged knee joint. The disease becomes chronic and leads to immobility. The unpleasant thing is that the treatment is difficult and time-consuming. That's why treatment should never be neglected if you have a knee injury, even if the injury is minor.
Diagnosis of sports knee injuries
Diagnosis of sports knee injuries is complicated by the uniformity of symptoms of most knee injuries. An accurate diagnosis can only be made with the help of special devices. MRI is a versatile method that can be used to diagnose both bone and soft tissue damage.
An ultrasound machine can be used to detect abnormalities in soft tissue. X-rays can help eliminate or confirm the most serious assumptions about the condition of the cartilage and bone structure. When diagnosing meniscal injuries, atroscopy - a technical examination in which a miniature probe is inserted into the injured area - is performed.

SURGICAL TREATMENT
Most patients with a patellar tendon rupture require surgery to restore normal function to the knee joint. During this procedure, the tendon is reconnected to the kneecap.
The sooner the operation is carried out, the better the result. During a longer operation, the tendon shortens and becomes shorter.
Inpatient treatment. Tendon sutures are sometimes performed on an outpatient basis, but most patients remain in the hospital for at least a day after such a procedure. Whether this is the case in your particular case depends on the medical indications.
The procedure can be performed under regional anesthesia (spinal anesthesia), in which only the lower half of the body is 'frozen', or under general anesthesia.
Surgical technique. To repair the tendon, the end of the tendon is sutured, and these sutures are passed through bone channels created in the lower pole of the kneecap. The sutures are then tied, restoring the normal tension of the tendon and the correct position of the kneecap.
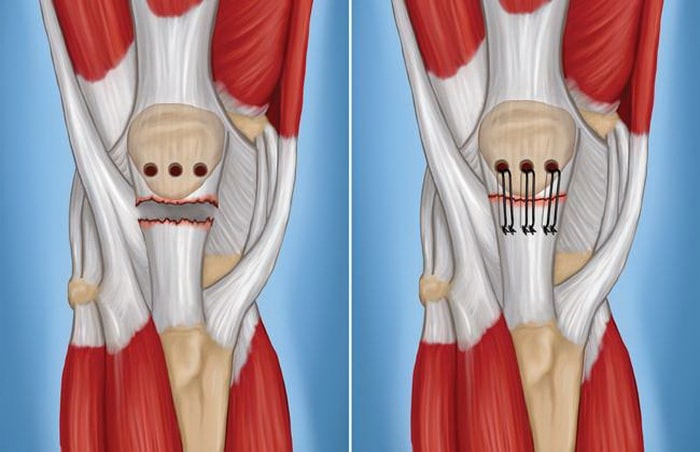
To repair the patellar tendon, small bone channels are created at the lower pole of the kneecap (left), through which threads are pulled to fix the tendon to the kneecap (right).
New minimally invasive techniques. Currently, suture anchors (anchors) are most commonly used to reattach the tendon to the kneecap. These are small metal or polymer implants with threads. Their use eliminates the need to create bone channels in the kneecap. It should be noted that the possibilities of these modern methods are much greater than in the past. The use of anchors will accelerate rehabilitation and improve functional outcome.
Additional methods of stabilization. Some surgeons find it necessary to stabilize the kneecap with wire sutures while the tendon heals to protect the tendon suture. In such cases, additional surgery may be required to remove this wire suture.
RESULTS OF SURGICAL TREATMENT
After a patellar tendon rupture, most patients return to their previous work and physical activity. Many patients notice limited mobility of the knee joint, although most have almost the same range of motion as the other knee joint.
If you are an athlete, your surgeon will probably want to assess the extent to which the knee joint has regained function and the strength of the surrounding muscles before allowing you to return to sport. For this purpose, special functional tests, such as: B. jumping on one leg. The muscle strength of the injured leg should be at least 85-90 % of the muscle strength of the healthy leg. In addition to muscle strength, parameters such as muscular endurance, body balance and the occurrence of swelling in the knee joint after strain are also assessed.
The surgeon will discuss with you in detail the options and conditions for returning to sporting activities.
Read more:- Injury of the tibial condyle.
- The lateral dislocation is.
- patellofemoral fold.
- Injury to the ligaments of the ankle.
- Injury to the ankle.
- How much does knee surgery cost?.
- Injury to the navicular semilunar ligament.
- heel bone injury.
