Here is Patient O's story.
A young man cut himself with a knife, the wound was deep and he was taken to the hospital where the deep flexor tendon of the fifth finger was surgically sewn up.
After difficult rehabilitation, the finger could be flexed but not fully extended and the tendon 'floated'. This was because the flexor tendon channel was too open to allow for a suture.
The patient came to me more than a year after the injury. We discussed all the treatment steps in detail and decided on a long and difficult road to recovery.
A very important condition for the first stage of treatment is full passive movement of the injured finger.

- RU2739275C1 - Method for diagnosing scapholunate ligament injury and instability - Google Patents
- Pictures
- Treatment of hand and wrist injuries
- treatment of injuries
- Irregularly healed fracture of the radial bone
- Fracture of the heel bone
- complications
- Treatment
- Associated Injuries.
- Conservative treatment of typical fractures of the radial bone.
- causes
- symptoms and diagnosis
- Diagnosis of periarticular and semi-articular dislocation
- Treatment of perilunate hand dislocation and crescent bone dislocation
- Ligament tear - what is it?
- Tear of the anterior cruciate ligament in the knee
- Radiological findings:
- X-ray picture:
- Computed tomography (CT).
- Magnetic Motion Picture (MPT).
- Istochniki:
RU2739275C1 - Method for diagnosing scapholunate ligament injury and instability - Google Patents
Publication number RU2739275C1 RU2739275C1 RU2020118462A RU2020118462A RU2739275C1 RU 2739275 C1 RU 2739275 C1 RU 2739275C1 RU 2020118462 A RU2020118 462A RU 2020118462A RU2020118462A A RU 2020118462A RU 2739275 C1 RU 2739275 C1 RU 2739275C1 RU 2739275C1 Authority RU Russia Key words from the prior art scaphoid wrist wrist joint Date from the State of the art 2020-. 05- 26 Application number RU2020118462A Other languages English ( de ) Inventor Olga Gennadyevna Shershneva Ivan Vladimirovich Kirpichev Federal State Budgetary Educational Institution of Higher Education 'Ivanovo State Medical Academy' of the Russian Ministry of Health Date of priority (Date of priority is an assumption and is no legal application. Google has not carried out any legal analysis and does not guarantee the accuracy of the date provided). 2020-05-26 Application date 2020-05-26 Publication date 2020-12-22 2020-05-26 Application submitted by the Federal Budgetary Educational Institution of Higher Education 'Ivanovo State Medical Academy' of the Ministry of Health of the Russian Federation Critical Federal Budgetary Educational Institution of Higher Education ' Ivanovo State Medical Academy' of the Ministry of Health of the Russian Federation 2020-. 05-26 Priority to RU2020118462A Priority Critical patent/RU2739275C1/ru 2020-12-22 Application granted Critical 2020-12-22 Publication RU2739275C1 Publication Critical patent/RU2739275C1/ru
- Espacenet
- Global documentation
- discussion
- 2100003041 Ligaments Anatomy 0.000 Title Claims Summary Description 19
- 238000007906 compression method 0.000 claims abstract description 10
- 206010061194 Hand Deformity Disorders 0.000 Word Description 3
- 2100003857 Anatomy of the wrist 0.000 abstract description 25
- 210000000707 wrist anatomy 0.000 abstract description 17
- 206010022114 Trauma-Related Disorders 0.000 abstract description 10
- 208000002193 pain diseases 0.000 abstract description 10
- 230000036407 pain effects 0.000 abstract description 10
- 2100001513 Anatomy of the elbow 0.000 abstract description 8
- 2300003068 Static effects 0.000 abstract description 5
- 239000003814 medicinal substances 0.000 abstract description 3
- 230000000399 orthopedic effects 0.000 abstract description 3
- 238000007374 Clinical diagnostic method methods 0.000 abstract description 2
- 230000000694 Effects 0.000 Short description 1
- 230000000414 obstructive effects 0.000 Brief description 1
- 2390000126 Substance Substances 0.000 Description 1
- 2100003189 Bone anatomy of the scapula 0.000 Abstract 8
- 238000000034 methods 0.000 description 8
- 2100003991 Anatomy of the lunar bone 0.000 Description 7
- 238000003745 Diagnostic methods 0.000 Description 5
- 238000002595 Magnetic resonance imaging methods 0.000 Description 5
- 238000002591 Computed tomography methods 0.000 Description 4
- 210000000988 Bone and Bone Anatomy 0.000 Description 3
- 206010061223 Ligament Damage Diseases 0.000 Description 3
- 238000001514 Verification method 0.000 Description 3
- 238000010494 dissociation reaction Methods 0.000 Description 3
- 2300005593 Dissociation Effects 0.000 Description 3
- 201000008482 Osteoarthritis Diseases 0.000 Description 3
- 2300001154 Acute Effects 0.000 Description 2
- 238000002347 Injection Methods 0.000 Description 2
- 230009007924 injection substances 0.000 description 2
- 101700052881 AARD proteins 0.000 Description 1
- 206010003246 Arthritis diseases 0.000 Description 1
- 2100002753 Anatomy of the scaphoid 0.000 Description 1
- 210000000845 Anatomy of Cartilage 0.000 Description 1
- 241000766026 Species of Coregonus nasus 0.000 Description 1
- 208000005137 Joint Instability Diseases 0.000 Description 1
- 206010065433 Ligament Rupture Diseases 0.000 Description 1
- 206010030113 Swelling Diseases 0.000 Description 1
- 241000906034 Orthopedic diseases 0.000 Description 1
- 2300003412 Degeneration Effects 0.000 Description 1
- 238000002405 Diagnostic procedure Methods 0.000 Description 1
- 201000010099 Disease Diseases 0.000 Description 1
- 2390000463 Material Substances 0.000 Description 1
- 238000002559 Palpation Methods 0.000 Description 1
- 239000011505 Gypsum substances 0.000 Description 1
- 239000003381 Stabilizer Substances 0.000 Description 1
- 238000001356 Surgery Methods 0.000 Description 1
- 2300002522 Swelling Methods 0.000 Description 1
- 230000000472 Violation Effects 0.000 Description 1
Pictures
- A – HUMAN NEEDS
- A61 – MEDICAL OR VETERINARY SCIENCES; HYGIENE
- A61B – DIAGNOSTICS; SURGERY; IDENTIFICATION
- A61B6/00 - Devices for radiological diagnosis, e.g. B. in combination with radiation therapy devices
- A61B6/50 - Clinical Applications
- A61B6/505 - Clinical applications including bone diagnostics
Treatment of hand and wrist injuries
Approximately 40% of upper limb fractures are fractures of the hand involving 27 bones. Given the numerous functions it can perform, the hand and wrist must be treated with anatomical and surgical techniques to reconstruct damaged structures. In the hospital, osteosynthesis of any complexity is performed using the most modern metal fixation devices.
The most common hand injury in humans is a fracture of the distal portion of the metaepiphysis of the radial bone ('Typical Location Radius Fracture'). In intra-articular fractures of the radial bone, the anatomical restoration of the articular surface is crucial. Currently, arthroscopically guided fracture fusion is the best way to achieve this. With this method, the joint can be viewed from the inside using an arthroscope—a camera held through a small incision (up to 5-7 mm). The hospital uses endoscopic devices and metal fixators from Arthrex, a world leader in this field.
The most common hand injuries are tendon injuries. The hospital's doctors have exceptional experience in treating both fresh and chronic wrist injuries. All types of plastic surgery are performed, including silicone prostheses.
In recent years, the focus has shifted to restoring the soft tissue structures of the hand and wrist. Ligament injuries are characterized by instability (a 'walking sensation') and pain in what is known as the ulnar angle of the wrist. One of the most common causes of these symptoms is damage to the triangular fibrocartilage complex (similar to the meniscus in the knee joint). In the hospital, this complex is sutured with special anchor fixators, including using endoscopic devices.
treatment of injuries
Medical care of hand injuries is often not provided in a timely and appropriate manner, which leads to undesirable consequences - broken bones with displacement, permanent contractures (restricted movement) of finger joints, sensory disturbances, gross scarring of the skin, etc.
The hospital's specialists are proficient in a variety of modern, high-tech surgical techniques, such as B. Corrective osteotomies of the wrist, skin grafts with various flap options and microsurgical techniques for suturing vessels and nerves.
Irregularly healed fracture of the radial bone
Briefly, a subcutaneous extensor digitorum tear is the most common tendon injury, a closed injury to the extensor apparatus of the finger at the level of the distal interphalangeal joint.
Read more belowThumb injuries are often caused by a fall where the hand is resting on an object (e.g. a ski pole). For this reason, an injury to the ulnar collateral ligament of the first metatarsophalangeal joint is referred to as 'skier's thumb'.
The term 'forester's thumb' can also be found in the literature. It's thought to be the same condition, but actually there are some differences. These lie in the mechanism of damage, which is different for skiers and foresters.
Read more belowFracture of the heel bone
A fracture of the navicular bone in the wrist is a very unpleasant injury that requires long and complicated treatment. Delayed referral to the doctor, failure to recognize the fracture during the initial examination, and missing or inadequate treatment are not uncommon. I hope that this article will help all those who have or suspect a similar injury.
Read moreHand fractures are often the result of violent action by the injured party, an unfortunate punch against a hard object can result in a fracture. There's even a special term for the 5th metacarpal - a box fracture.
It can also be caused by dropping your hand or hitting something hard with your hand.
Read more at .complications
The progressive deformity of the crescent bone is accompanied by persistent rotational subluxation of the scaphoid, and disruption of wrist biomechanics leads to severe deformative osteoarthritis. In some cases, there may be compression of the median nerve in the carpal canal; pathological tears of the flexor or extensor tendons of the fingers may be present.

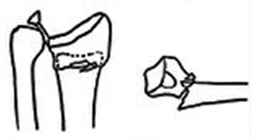
Fig. 1: Wrist radiographs (straight projection on the left and lateral projection on the right) in fragmented Kinbeck's disease: arrows indicate the affected crescent bone.
Clinical diagnosis is difficult in the early stages of the disease, but if the symptoms match (irregular pain at the base of the wrist, localized pain in the area of the crescent bone, increasing pain with extreme flexion and extension of the wrist), the suspicion of this disease can be raised fall.
The X-ray examination is decisive for the diagnosis, but changes in the sickle bone can only be detected 2-3 months after the onset of the disease. On the x-ray, a change in the shape and an increase in the density of the crescent shadow is characteristic. The shadow takes on an irregular triangular shape, the height of the shadow decreases, and the contours of the bone remain distinct but uneven and wavy. At the fragmentation stage, the bone splits into fragments of different shapes, sizes and densities (Fig. 1), each with an irregular outline. In stages III and IV, the crescent bone remains flattened and the adjacent joint space fragments are enlarged. A gradual, incomplete restoration of the pattern of bone structure and shape follows. The crescent-shaped bone remains deformed, and spongy bony outgrowths develop at its edges. Similar hypertrophy occurs on the adjacent articular surfaces (Stage V). The joint space narrows instead of widening. In some cases, intra-articular bodies are discovered in the articular cavity.
Treatment

Fig. 2. Scheme of semilunar-radial arthrodesis with a cylindrical graft with partial destruction of the semilunar bone: 1 – creating a cylindrical defect (outlined circle) at the junction of the affected crescent and radial bone, on the right – the same in a lateral projection (dashed lines indicate the boundaries of the defect); 2 - insertion of a cylindrical graft (shaded); the wrist is immobilized with a spoke, right - lateral projection.

Fig. 3: Schematic representation of the operation to replace the resected crescent bone with a silicone endoprosthesis (according to Swenson): The prosthesis post is inserted into the crescent-shaped bone (arrow).

Associated Injuries.
50 % of these fractures are intra-articular and may involve damage to the distal radius-ulnar joint, 40 % to damage to the triangular cartilage, 30 % to damage to the navicular-lunate ligament, and 15 % to damage to the semilunate-triangular ligament.
Classification of fractures of the radial bone at a typical site.
Fracture type depending on the injury mechanism
Stable (risk of secondary displacement in cast)
Stable, the risk of secondary displacement is low.
1)No displacement 2)Dorsal displacement (Collis fracture) 3)Palatinal displacement (Smith fracture)

Unstable, always secondary displacement
1)Open repositioning. Internal fixation
Type 3 with compression of the articular surface

Can be both stable and unstable depending on the quality of the bone and the number of fragments
Can be conservative if there is no significant displacement.
Type 4 - Tear of ligament structures with wrist dislocation

Closed or open disposal. External fixator. Immobilization of the bony fragments with pins/screws.
Type 5 - Combined High Energy Injury

Combined closed/open 0000 method,
And of course the AO classification that we all love.
Conservative treatment of typical fractures of the radial bone.
Cast immobilization for 4 to 6 weeks depending on fracture morphology, age, presence or absence of osteoporosis. In the case of simple fractures of the distal radius bone, active movement of the wrist can be started after 4 weeks if the cast immobilization ensures sufficient stabilization. When cast immobilization is used as a coercive measure to treat fractured, unstable, intra-articular fractures, e.g. if surgery is to be avoided, immobilization must be prolonged because of the risk of necrosis of the fracture and formation of a false joint.
If the normal position of the fracture is not reached during the initial repositioning, there is a risk of subsequent dislocation of the fracture.
Potential complications of cast immobilization include acute carpal tunnel syndrome and complex regional pain syndrome (when cast immobilization is used when swelling is severe).
causes
A periarticular dislocation is a dislocation in which the crescent bone remains in place while the other bones are displaced backward and proximally (towards the elbow). These dislocations are five times more common than crescent bone dislocations and account for more than 90 % of all wrist dislocations. However, with spontaneous dislocation of the crescent bone, when the other bones are in place, there is a secondary dislocation of the crescent bone, which in its new position rotates like a 'tipped bowl' and no longer has the shape of the adjacent bones. This is the condition described above, which is the most common wrist dislocation.
A dislocation of the sickle bone is one of the typical injuries in a fall when the weight of the body multiplied by the acceleration rests almost entirely on the outstretched hand (the outstretched hand is in the position of an acrobat, gymnast or circus performer when it is e.g (e.g. perform a stand-up with straight arms or a back somersault with hand supports). A similar dislocation can occur during a 'defensive' straight-arm movement, e.g. B. trying to stop a fast approaching object, as well as in traffic accidents and other similar situations.
symptoms and diagnosis
Pain, swelling and restricted movement in the joint are the most common symptoms of a dislocation. There is usually marked posterior dorsiflexion of the wrist and abnormal protrusion of the hand. The fingers are usually in a forced semi-flexed position.
The pain syndrome is especially aggravated when the displaced crescent bone exerts mechanical pressure on the median nerve.
An experienced traumatologist will recognize or suspect a dislocation of the crescent bone upon examination, but because of the risk of associated complications or fractures, a definitive diagnosis can only be made radiographically—two projections are always made, with the lateral one usually being the most conclusive.
Diagnosis of periarticular and semi-articular dislocation
Review of radiographs (anteroposterior, lateral and oblique projections). In order not to miss the diagnosis, the doctor must assess the relationship between the radial bones, sickle bones and skull bones on the lateral x-ray.
In the periarticular dislocation On a lateral wrist x-ray, the cranial bone is misaligned in the vertical axis with the crescent and radius bones. The crescent and radius bones stay in line.
In the Dislocation of the crescent bone. This bone is twisted and misaligned in relation to the other bones; on the x-ray it appears as an 'inverted teapot'.
Treatment of perilunate hand dislocation and crescent bone dislocation
Both perilunar and semilunar dislocations are treated in the emergency department with closed reduction and splinting. The wrist and elbow joint must be fixed in a neutral position (e.g. with a U-splint).
The patient should be referred to an orthopedist immediately; most cases of dislocations should be treated surgically because joint function can be better preserved after surgery.
Ligament tear - what is it?
Here you will learn what a ligament separation is and why it is dangerous for the patient's health and mobility. First, let's discuss the anatomy and physiology of the knee and ankle joints.
The knee joint is formed by the fusion of the condyles of the tibia and femur. These are separated by a dense meniscus cartilage, which absorbs the forces that occur when walking, running and jumping. A dense joint capsule forms around the joint, which contains synovial fluid that is absorbed and secreted by the cartilage that covers the bone heads. This is another cushioning protection mechanism. At the front of the joint is a triangular bone called the kneecap. It is connected to the epiphyses of the tibia and thigh via tendons and its own ligaments.
The stability of the knee itself is provided by four main ligaments:
- The anterior cruciate ligament prevents the femoral condyles from moving forward;
- the posterior cruciate ligament limits backward movement of the tibial condyle;
- 2 collateral ligaments (lateral and medial) restrict mobility in the right and left lateral planes).
Swelling and swelling of the anterior cruciate ligament are the most common problems faced by traumatologists and orthopedic surgeons, since the anterior cruciate ligament bears the greatest physical, mechanical and shock-absorbing loads. Young, active, athletic people who regularly overload their lower limbs are most often affected.
The posterior and lateral cruciate ligaments are less affected. However, severe trauma also causes damage to the collagen fibers that make up the ligamentous tissue.
In normal physiology, the ligament of the ankle or knee joint is made up of tightly woven collagen fibers. It is strong connective tissue. Its disadvantage is its low elasticity and the complete lack of its own blood supply. It can only hold a limited amount of fluid when the surrounding muscles are active.
Tear of the anterior cruciate ligament in the knee
Anterior cruciate ligament strain is a common occupational disease in athletes, wheel loaders, construction workers, painters, plasterers and other trades that are generally associated with increased physical stress on the lower limbs.
In about 60 percent of all cases, the anterior cruciate ligament is injured. This can happen after an initial dislocation or as a result of scar deformity after multiple dislocations or bruises.
A tear in the anterior cruciate ligament is manifested by a feeling of instability in the knee when walking. Any clumsy movement causes a stabbing pain that limits the mobility of the leg for a few days. After that, a relative normality returns. Sooner or later the anterior cruciate ligament will tear completely. This makes walking independently impossible. Surgery is required to restore the integrity of the ligament.
A tear in the anterior cruciate ligament is compensated in most cases. The cushioning load is absorbed by the increased work of the surrounding muscles. Patients are therefore only slightly affected by this pathology. Even with a complete rupture of the posterior cruciate ligament, the patient is initially able to walk or squat. However, the anterior cruciate ligament is affected after 2 to 3 months.
Radiological findings:
Uniform, extensive ossification along the posterior surface of the vertebral bodies, with relatively minor degenerative changes in the intervertebral discs and no ankylosis of the arch joints.
More commonly from mid-cervical (NW-C5) to mid-thoracic (Th4-Th7) levels.
From local thickening to extensive continuous ossification (ligament thickness approx. 2-5 mm).
Morphological features:
ZPS ossification leads to a reduction in the anteroposterior diameter of the spinal canal, resulting in spinal stenosis that compresses the spinal cord.
X-ray picture:
- Widened area of ossification in the posterior part of the vertebral bodies.
- In the lateral projection, the shadow of the ossification is often superimposed by the shadow of the arch joints.
- When interpreting X-ray images, the changes can be so minimal that they are easy to see, so this pathology should always be kept in mind.
Computed tomography (CT).
- The distinctive 'inverted T' or 'bow-tie' appearance of MDA on axial slices.
- The ossification pattern of the VEP is similar to that on the anaerobic CT slices.
- The cortical lamina delimiting the central intraspinal space can fuse with the underlying lid lamina.
- The vertebral body can be separated from it.
- The intraspinal spaces of the ossified MAL and the vertebral body do not communicate with each other.
Magnetic Motion Picture (MPT).
T1-weighted image:
- Continuous ossification in the posterior part of the vertebral body, extending over several planes on sagittal images.
- A characteristic 'inverted T' or 'bow-tie' pattern is seen on axial images.
- The signal is typically low in intensity in all exam modes.
- При значительном объеме жирового компонента in костно-мозговом пространстве оссификата интенсивность сигнала может быть гиперинтесивной.
Istochniki:
Fehlings MG et al: Cervical spondylotic myelopathy: current state of the art and future directions. Spine (Phila Pa 1976). 38(22 Suppl 1):S1-8, 2013.
2 Li H et al: A systematic review of complications in cervical spine surgery for ossification of the posterior longitudinal ligament. Spine J. 11(11):1049-57, 2011.
3 Saetia K et al: Ossification of the posterior longitudinal ligament: a review. Neurosurg Focus. 30(3):E1, 2011
4. Shin JH et al: Dorsal versus ventral surgery for cervical ossification of the posterior longitudinal ligament: considerations on choice of approach and review of surgical outcomes. Neurosurg Focus. 30(3):E8, 2011
5. Matsunaga S et al: Radiographic predictors of the development of myelopathy in patients with ossification of the posterior longitudinal ligament: a multicenter cohort study. Spine (Phila Pa 1976). 33(24):2648-50, 2008
6. Inamasu J et al: Posterior longitudinal ligament ossification: an update on biology, epidemiology and natural history. neurosurgery. 58(6):1027-39; dyskusia 1027-39, 2006 r.
7. Matsunaga S et al: Clinical course of patients with ossification of the posterior longitudinal ligament: a minimum 10-year cohort study. J Neurosurg. 100(3 Suppl):245-8, 2004
8. Shiraishi T et al: Cervical epidural calcification in patients undergoing long-term hemodialysis. Report of two cases. 100(3 Suppl): 284-6, 2004
9 Kamizono J et al: Occupational recovery after open-door laminoplasty in patients with ossification of the posterior longitudinal ligament. spines 28(16):1889-92, 2003
10 Epstein N: Diagnosis and surgical treatment of ossification of the posterior longitudinal ligament in the cervical spine. Spine J. 2(6):436-49, 2002
- The intercondylar syndesmosis is the.
- tibial ligaments.
- Rupture of the ankle.
- Bone structure of the navicular foot.
- Axis of rotation of the knee joint.
- shoulder brace.
- How much does knee surgery cost?.
- Dislocation of a bone in a joint.










