The knee specialists at the Joint Clinic choose from several methods for the surgical treatment of Albeck's disease. In order to create an individual treatment plan, the stage of the disease must be determined. Almost all methods are aimed at increasing the vitality and regenerative ability of necrotic bone tissue.
- Deforming osteitis (Paget's disease, deforming osteodystrophy, deforming osteosis)
- ICD-10
- etiology
- diagnosis
- Symptoms of inflammation of the skin around the bones (periostitis)
- Periostitis of the tibia
- inflammation of the shin bone (periostitis)
- diagnosis
- Surgery for aseptic necrosis of the femoral condyle
- Surgical treatment of osteonecrosis of the knee (Albec disease)
- Diagnosis of osteonecrosis of the knee joint
- diagnosis
- Conservative treatment
- Treatment of osteonecrosis
- Conservative treatment
- surgical treatment
- costs of the services
- Treatment of bone cysts
- The symptoms.
- Fracture of the tibial plateau
- Treatment
Deforming osteitis (Paget's disease, deforming osteodystrophy, deforming osteosis)

Deforming osteitis (Deforming osteitis) – is an inflammatory disease in which one or more bones of the skeleton are damaged. It is accompanied by the formation of enlarged, easily deformed bones that are at risk of fracture. It manifests itself through pain and changes in shape in the affected region. If the skull and spine are affected, neurological complications can occur. Diagnosis is made based on history, physical examination, x-rays, CT and MRI scans, and alkaline phosphatase measurement. Treatment consists of immobilization and pharmacotherapy.
ICD-10
Deforming osteitis (Latin osteon - bone) or Paget's disease is an inflammatory disease that affects the bone and is usually localized. In the early stages of the disease, partial destruction of bone tissue occurs, followed by excessive regeneration. The regenerated bone is deformed, brittle and susceptible to fracture. The causes of the development of deforming osteitis are not yet known. It is not possible to completely eliminate the symptoms of the disease. Symptomatic treatment and prevention of complications are carried out.
Deforming osteitis can affect any bone. On average, three bones are affected per patient, but only one bone or several bones can be affected. The disease is quite common and occurs mainly in European men over 50 years of age. It is very rare in people of African and Asian descent and in young people of all races.
etiology
Metaphyseal bone loss usually occurs in childhood, during the period of active bone growth, and is most common in men. The lesions are usually located in the cortical layer of the metaphysis of long, scarred bones. They occur most frequently in the femur (distal metaphysis) and tibia (with equal frequency in the proximal and distal metaphysis). Up to 80 % of all observed foci were found at this site. This also applies to the frequent localization in the fibula. When this pathology is combined with coffee-like skin pigmentation, Jaffe-Campanacci syndrome is diagnosed (a combination of multiple foci in the bones, coffee-like skin pigmentation, mental retardation, hypogonadism, cryptorchidism, ocular anomalies and cardiovascular anomalies). So far only individual cases have been described.
A large number of MFKD have been observed to resolve spontaneously. They often do not show a clear orthopedic picture in children and are mainly an X-ray finding. In a number of cases, the defect is extensive and painful, requiring surgical treatment.
NF is characterized by a higher frequency of pain than MFKD. In neosteogenic fibromas, a pathological fracture is possible in 40 % cases. In addition to pain, there is swelling around the lesion that has a thick consistency.
diagnosis
X-rays, CT scans, and MRIs are important examinations in patients with MFKD. In this case, CT allows a more accurate determination of the extent of the lesion and the risk of a pathological fracture. MRI is more commonly performed for differential diagnosis.
If there is a defect of less than 1/3 of the bone cross-section (not a pathological fracture), conservative treatment and monitoring with the exclusion of physical activity is possible until the lesion is closed. If pain occurs and the lesion is larger than 1/3 of the bone cross-section, surgical intervention in the form of marginal resection and bone grafting (autograft or allograft) is required. If there is a pathological fracture, extrafocal osteosynthesis is carried out.
MFDC is always benign and there is no recurrence after appropriate surgical intervention.
For more information about MFCD and how to address your specific case, please call our call center at +7 (499) 940-97-47.
Symptoms of inflammation of the skin around the bones (periostitis)
The main symptoms of periosteum inflammation are pain during various movements, discomfort and slight swelling in the inflamed areas. The color of the skin does not change and no discoloration, redness or bluish discoloration occurs. If periosteum inflammation is caused by a bruise or fracture, all symptoms and the inflammation will subside after 2-3 weeks. If there is an exacerbation and fibrous overgrowth of the bone, the disease progresses to a chronic stage. This stage is characterized, among other things, by reddening of the skin. If the periosteum inflammation is not treated therapeutically at this stage, a serious complication can develop later, leading to bone damage and purulent periosteum inflammation.
Periostitis of the tibia
This type of disease occurs as a result of heavy and prolonged stress without prior preparation. The main symptom of this type of periosteum is pain in the back of the shinbone, which occurs some time after loading. Shin splintitis is very common in first-year soldiers or in athletes after a break from training or a particularly difficult, unfamiliar exercise. The external symptom of the disease is slight swelling of the affected area. There are no lesions on the skin. There is also a painful, unpleasant feeling when touching the lower leg. In the first 20 days, the periosteum inflammation cannot be seen on the X-ray, after which the diagnosis can be made using an X-ray and a medical examination.
If a patient is suspected of having shin splintitis (periostitis), he or she should immediately stop physical activity to reduce the risk of development and complications of the disease.
inflammation of the shin bone (periostitis)
Periosteumitis most commonly occurs in areas where the bone is poorly protected by soft tissue. The causes of this condition are bruises and fractures. The ulna and shinbone are particularly at risk. In most cases it resolves spontaneously within a few weeks.
diagnosis
In the early stages, aseptic necrosis can only be diagnosed by MRI or scintigraphy. If the process is more extensive, the extent and location of the damage can be determined using x-rays and CT scans.
During the direct examination, the doctor takes a detailed anamnesis, assesses the function of the extremity and the general condition of the patient. A series of standard laboratory tests are also carried out.
Take advantage of the unique opportunity to receive a free consultation for elective surgery. Learn more.

Surgery for aseptic necrosis of the femoral condyle
Conservative therapies such as medication and physiotherapy are only suitable in the early stages of the disease. With progressive development of aseptic necrosis of the femoral condyles, surgical treatment is indicated.
Specialists have several treatment options available:
- Corrective osteotomy of the femur and tibia, during which damaged tissue is removed;
- Endoprosthetics, in which damaged osteochondral tissue is replaced with biosynthetic material;
- Osteochondral autoplasty, in which the damaged area is replaced with a graft from non-contact areas of the joint heads.
Depending on the extent and location of the aseptic necrosis, unicondylar arthroplasty, in which only the medial or lateral condyles of the thigh are replaced, or total arthroplasty, in which all structures are replaced, can be performed.
Surgical treatment of osteonecrosis of the knee (Albec disease)
Surgical treatment of Albec disease is aimed at initiating healing processes in the knee joint to promote bone regeneration. In principle, all joint-preserving interventions described below are recommended up to the third stage Albeck's disease. In the fourth stage, it is difficult to find viable cells in the bone that can be reactivated. In the fourth stage, replacement with an endoprosthesis is required.
- Relief of the knee by correcting the axis of the lower limbs: knee osteotomy
- Treatment of articular cartilage: Pridi drilling (a microsurgical technique used to repair cartilage defects) and grafts
- Decompression of the metacarpal bone
- Spongioplasty (molar bone autotransplantation)
- endoprosthetics
Diagnosis of osteonecrosis of the knee joint
The diagnosis of Albeck disease is made by excluding other possible diseases of the knee joint that are associated with similar symptoms. The patient's description of his condition is the most important criterion for diagnosing the disease. During the examination, the doctor will ask questions about the course of the disease and any injuries. The occurrence of traffic accidents is also important for the diagnosis.

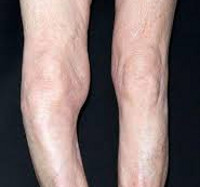
Diagnosis of knee joint disease © Joint Clinic / Prof. Dr. Sven Ostermeier
In any case, an x-ray will be taken. However, visible changes in the joint can only be noticed in an advanced stage of the disease. One of the most important signs of Albeck's disease on the X-ray is sclerosis - a painful thickening of the bone tissue that occurs due to overloading of the knee joint.
In the early stages of the Albeck's disease can be diagnosed by an MRI scan that shows a characteristic painful swelling. A bone density measurement is necessary to rule out osteoporosis of the entire human skeletal system.
If you have any questions about the knee and Albeck's disease, please contact the Joint Clinic in Germany. Dr. Ostermaer, Dr. Markwas, Dr. Rinio and the other specialists in our clinic are top-class doctors and can offer you high-quality treatment for Albeck disease at reasonable prices.
diagnosis
Instrumental examinations are required to confirm and clarify the diagnosis.

medical-massage-at-the-leg-in-a-physiotherapy-center_1139-1214-1.jpg
X-rays – these are taken in anteroposterior and lateral projection. Although x-rays are the most common examination when König's disease is suspected, they are not always conclusive. Even full-thickness hyaline cartilage defects may not be visible on x-ray. However, the femur is usually easy to see. With dissemination osteochondritis, the doctor sees a bright area near the knee joint. In this case, the trabecular structure of the bone is preserved. A necrotic area in the form of a thin band is often seen. In the early stages of the disease, the contour of the femoral condyle is preserved, but as the disease progresses, cavities may appear.
Radiological stages of osteochondritis dissemination:
MRI is the most accurate non-invasive examination. This technique allows the hyaline cartilage to be visualized and the condition of the subchondral bone and soft tissues to be assessed. The most reliable results are achieved with contrast-enhanced MRI.
Arthroscopy is an even more precise but invasive diagnostic method and is therefore rarely used. The doctor makes an incision in the knee and inserts a tube with a video camera to examine the joint from the inside. For diagnostic purposes, arthroscopy is only performed when an MRI scan is not sufficient or shortly before treatment of the disease.
The International Cartilage Repair Society divides the disease into four different stages:
- 1 – Softening of hyaline cartilage;
- 2 – partial detachment of cartilage;
- 3 – Interruption of cartilage formation
- 4 – Formation of free fragments.
Conservative treatment
Conservative treatment cannot cure the disease because damaged cartilage regenerates very poorly. However, therapy can help relieve symptoms and improve quality of life. It can delay the need for surgical treatment and is also used after surgery to improve outcomes.
- Restriction of the patient's activity, relief with an orthosis or immobilization for 1 to 6 months (effective only in young patients with cartilage damage in the non-load-bearing area);
- administration of nonsteroidal anti-inflammatory drugs;
- Injection of hyaluronate, platelet-rich plasma and stem cells into the knee joint;
- Physical therapy;
- shockwave therapy;
- therapeutic exercises.
In recent years, doctors have increasingly chosen surgical treatment of osteochondritis dissection without attempting conservative therapy. This is because in the early stages, when cartilage and bone loss is still minimal, surgery provides the best results. In addition, conservative procedures only affect the symptoms. They cannot cure or even slow the progression of the disease.
Long-term results of conservative therapy can only be expected in children. Sometimes completely relieving the weight of the limb creates the conditions for the cartilage and underlying bone to rebuild. However, if there is no improvement within three months, the patient undergoes surgery.
The success rate of conservative treatment of König's disease in children is between 50 % and 94 % in various studies. The younger the child, the better the prognosis. A cast is usually applied and x-rays are taken regularly to assess the progression of the disease. If the result is positive, immobilization and restriction of physical activity are indicated in the second phase after the cast has been removed. X-rays are taken every one and a half to two months and the load is gradually increased. On average, 2 out of 3 children achieve good treatment results after six months with this approach.
Treatment of osteonecrosis
The specifics of the treatment of osteonecrosis depends primarily on the following nuances:
Experts divide aseptic necrosis into four stages:
Stages 1 and 2, which last up to a year, are characterized by the formation of swollen bone tissue visible on MRI and offer a high probability of recovery.
Stages 3 and 4 are characterized by almost irreversible bone destruction.
Therefore, if the patient is in stage I and, in some cases, stage II, conservative measures can be taken.
Conservative treatment
Conservative treatment of primary osteonecrosis may include the following.
- Pharmacological treatment with non-steroidal anti-inflammatory drugs (e.g. ibuprofen), which are very effective in controlling pain and inflammation. Vitamin complexes and chondroprotectors can also be used to improve the effectiveness of treatment;
- The use of orthoses or crutches in conjunction with limited loading, particularly on the affected limb. This slows the progression of osteonecrosis and creates optimal conditions for tissue repair;
- Individual therapeutic exercise program with a therapist, including participation in swimming pool activities;
- Limiting the number of movements that cause pain (activity modification).
As a rule, conservative treatment, with competent development and adherence to a number of recommendations, leads to positive results.
In cases where the area of joint lesions is sufficiently large and conservative treatment did not produce the desired results, specialists recommend minimally invasive arthroscopic surgical intervention.
surgical treatment
There are a number of highly effective surgical techniques for the treatment of aseptic necrosis.
costs of the services
- Collection of the patient's complaints and medical history
- Examination of the patient
- Diagnosis of the symptoms
- Examination of blood samples, x-rays, MRIs and other examinations
- Creating a diagnosis
- Determination of treatment strategies and procedures.
- Re-examination of the results of the diagnosis made at the first visit to the doctor's office
- Making an accurate diagnosis
- Development of a treatment plan
Intra-articular injection of hyaluronic acid (Duralan is not included)
PRP treatment and plasmolifting (for injuries and/or diseases of the knee joint)
- Consultation of an orthopedic surgeon
- Collection of blood for analysis
- Preparation of plasma with a high number of platelets
- Injecting the plasma into the affected area
Corrective osteotomy of the shinbone in the case of knee osteoarthritis
- hospitalization
- epidural
- surgery
- Surgical screws and plates
- Other surgical material
- hospitalization
- epidural
- Arthroscopy, chondroplasty and coaptation of damaged cartilage (meniscectomy on a case-by-case basis)
- consumables for surgical interventions
One-arm knee replacement
- hospitalization
- epidural
- endoprosthetics
- Surgical materials
- Knee endoprosthesis
- Post-operative examination
- Postoperative MRI and X-ray examination
- Recommendations for rehabilitation
- puncture of the knee joint
- Intra-articular injection of hyaluronic acid
- Removal of stitches
Treatment of bone cysts
Conservative treatment includes puncture (two needles are inserted into the body of the cyst to suck out fluid and administer medications to reduce bone destruction), a plaster cast (in case of a fracture), physical therapy, and physical therapy exercises. If conservative treatment is ineffective, the patient is treated surgically.
If the disease is already advanced and no treatment is carried out, destruction and necrosis of the bone tissue may occur, which may lead to the complete removal of the damaged part.
Aseptic bone necrosis – Necrosis is a condition that leads to the death (necrosis) of bone parts and bones in general, due to the interruption or complete cessation of blood flow in a certain area of the bone. Idiopathic aseptic necrosis develops spontaneously without any specific cause. There are complete and partial necrosis of the bone, with a distinction being made between superficial and deep necrosis depending on the location in the bone. The disease progresses in several stages.
The symptoms.
The first symptoms of aseptic necrosis may not appear immediately. Sometimes it can last months or even years after the injury. pain with movement, which can lead to muscle contractures; Muscular dystrophy; Restriction of movement of the affected body part; Shortening of the limbs.
Bone cysts and necrosis can be diagnosed using the following methods:
- Medical examination (assessment of complaints, palpation of the affected area)
- X-ray of the affected bone in multiple projections
- Computed tomography (CT) or magnetic resonance imaging (MRI)
- Puncture (in the case of bone cysts, the contents are removed for analysis)
- Blood test (in case of other diseases)
Fracture of the tibial plateau
- SECTION MENU
- Allergology-Immunology
- Allergic rhinoconjunctivitis
- Allergy to grass pollen
- Allergic dermatitis
- Allergy to pets
- Allergy to house dust and its components
- Allergy to insects
- Allergy to pollen
- Allergy to tree pollen
- Allergy to grass pollen
- Eczema and other immune-mediated dermatoses
- Allergy to insect bites
- angioedema and Quincke's edema
- Atopic dermatitis
- immune disorders
- Allergy to drugs
- Acute and chronic urticaria
- Early signs of allergy
- Allergic alveolitis
- Why do my ovaries hurt and what can I do about it?
- Dysplasia of the cervix
- How to prepare for a visit to the gynecologist?
- Causes of abdominal pain
- Stroke of the ovary
- Bartholin's inflammation, cyst or abscess
- Ectopic pregnancy
- hematoma
- hydrosalpinx
- Hyperplasia of the endometrium (hypertrophy, polyps)
- Leukoplakia of the cervix
- endometritis of the uterus
- Uterine fibroids
- menstrual disorders
- Ovarian tumors (cysts and cysts)
- Prolapse and prolapse of the uterus and vagina
- Polycystic ovaries
- cervical polyps
- Spontaneous termination of pregnancy
- endometriosis
- Cervical erosion and ectropion
- Current approaches to the diagnosis of cervical abnormalities
- sinus infection
- Chronic rhinitis
- Nasal furunculosis
- pharyngitis
- inflammation of the tonsils
- Polypoid stomatitis
- otitis media
- acute rhinitis
- nosebleeds
- laryngitis
- Distorted nasal septum
- ENT diagnosis
- Repair of a peri-tonsillar abscess
Treatment
The fracture of the condyle is treated as an inpatient. If there is a sprain, a puncture is performed to drain the accumulated blood into the joint. In the next phase, the joint is immobilized with a plaster cast from the buttocks to the toes. The prerequisite for effective treatment is a state of calm.
When treating this type of fracture, an individual approach is taken and, if necessary, the injured joint is put under early pressure. The treatment algorithm depends on the severity of the injury.
A condylar fracture requires immediate treatment by a surgeon. The earlier the patient is treated, the better the result. Complications such as joint instability can occur if the treatment measures are not carried out correctly or the doctor's instructions are not followed.
- Pain in the periosteum of the tibia.
- Bones of the tarsal bone of the hand.
- Fracture of the lateral condyle.
- metatarsal and metacarpal bones.
- Pain in the heel bone of the foot.
- ligaments in the ankle.
- Rupture of the ankle.
- function of the fibula.
