Dysfunction of the pelvic organs are not uncommon symptoms of MS. The following disorders are common:

- paraparesis and paresthesia
- causes
- Causes and risk factors
- forms of hemiparesis
- classification
- Why muscle weakness occurs
- Causes of muscle weakness in the limbs
- Symptoms of tropical spastic paresis
- Treatment
- Complications of Multiple Sclerosis
- Diagnosis of multiple sclerosis
- Causes of paresis.
- paresis of the feet.
- Types of paralysis and their symptoms
- Diagnosis and treatment of paralysis in the elderly
- Clinical Signs of Intramedullary Brachial Plexus Injury
- Treatment of flaccid paralysis in children and adolescents
paraparesis and paresthesia
First of all, as always, we should define the terms. Paraparesis is the complete and unconditional immobility of an organ or system for which motor activity is the primary natural function. It is the patient's inability to trigger this activity 'from within' - neither through conscious nor unconscious effort of will, while from the outside e.g. For example, a paralyzed leg can be twisted at the hip or bent at the knee with one's own hands or the hands of another person. This is the difference between paralysis and a muscle spasm or joint contracture, where such movement is essentially impossible; the term 'paralysis' precisely underscores the inability of the paralyzed organ to obey a command from the central nervous system.
Paresis means 'weakness, loss of strength' in Greek; the term refers to an incomplete paralysis (also translated as 'slack', by the way) in which available muscle strength or the original range of possible movements is partially retained; the degree of this preservation can vary greatly.
The term 'plegie' ('stroke') is often used as a synonym for the term 'paralysis', which is semantically close to the terms 'apoplexy' and 'stroke', which is the etymological basis of the obsolete Russian phraseology 'had a stroke', 'after a stroke paralysis broke in', 'stroke of apoplexy' etc. seems to have formed. However, in modern medical terminology, the word 'plegia' is usually used with qualifying prefixes: hemiplegia (paralysis on one side), mono-, para- or tetraplegia (paralysis of one, both or all four limbs).
causes
In general, the cause of paralysis and paresis can be formulated as a disruption in the interaction between the CNS (brain and spinal cord) and the peripheral executive system (skeletal, intestinal, bulbous, sphincteric and other muscular systems).
- Failure of the central nervous system itself (eg, in dystrophic-degenerative diseases, various atrophic, oncological, inflammatory processes, ischemic and hemorrhagic strokes, mechanical damage to motor areas of the cerebral cortex and/or motor neurons of the spinal cord)
- End-stage organ failure (eg, muscle wasting, severe fracture of musculoskeletal structures, or intoxication with certain toxins, particularly herbal toxins known to cause complete muscle paralysis and painful death by asphyxiation and/or cardiac arrest can);
- Damage to the communication system - essentially a disruption in the communication between the central nervous system and the muscular system: in this case there are no activating nerve impulses to a fully functional 'performer' (traumatic, atrophic and other damage or changes in nerve conduction channels).
So-called 'sleep apnea' or hypnopompic ('after waking up') paralysis is sometimes considered a relatively distinct form. This state, which is caused by disrupted or unfulfilled sleep patterns, can last up to several minutes and is usually accompanied by panicked life terror (a sudden awakening in an awareness of absolute stillness, vulnerability, and helplessness) and vivid, frightening hallucinations ('aliens', ' 'invaders', 'rapists', 'murderers', etc.), sometimes with a complete tactile illusion of acts being performed on the paralyzed person. Most notably, he is the source of a small but steady stream of authentic allegations of 'alien abductions', 'demon contact' and absurd (but sometimes very real and serious) allegations of assault and rape. The mechanism for the development of this state is related to the fact that during REM sleep motor activity must be automatically switched off; this is a normal, physiologically based, protective paralysis (otherwise somnambulism or sleepwalking results). 'Sleepwalking', ie dreaming in different variants and forms). However, under unfavorable conditions (chronic stressful situations associated with sleep deprivation, certain psychiatric diseases, narcolepsy, that is, pathological drowsiness, etc.), the reverse activation of motor functions is delayed, and awakening occurs earlier, in the 'rapid' phase.
Causes and risk factors
Hemiparesis can be of primary or secondary origin, either as a distinct disease or as a sequela or symptom of another disease. It can also be diagnosed during the recovery period after hemiplegia. The easiest way to determine the cause is to look at the location of the problem, i.e. whether the left or right side is affected.
The most likely causes of hemiparesis are:
- Stroke – blockage or rupture of cerebral vessels with subsequent bleeding;
- Tumors, benign or malignant – as they grow, they compress surrounding tissue and damage healthy cells;
- Traumatic brain injuries - bruises, concussions are accompanied by necrosis of pieces of tissue;
- Encephalitis - a large group of infectious diseases associated with inflammation of the brain and neurological disorders;
- epileptic states - especially dangerous when the next seizure ends in a contraction of the skeletal muscles, which inevitably leads to paralysis;
- migraine - severe headaches of unclear etiology, which can cause hemiparesis only in particularly severe cases;
- Multiple sclerosis - contributes to the destruction of nerve sheaths, leading to nerve damage;
- Atrophy of brain tissue – this process leads to the death of neurons, which inevitably leads to sensory impairments in certain areas of the body;
- Diabetes mellitus - its severe course causes spasmodic cerebral vascular spasms;
- Cerebral palsy – in this case, hemiparesis is considered to be congenital, in utero or acquired during childbirth.
forms of hemiparesis
Depending on the origin, two forms of hemiparesis are distinguished:
The disease is divided according to its place of origin into:
- Central hemiparesis - caused by disturbances in the pyramidal tract from the CGM to the anterior horns of the spinal cord;
- Peripheral hemiparesis – caused by damage to the cranial nerve nuclei, the cells that make up the anterior horns of the spinal cord.
Hemiparesis usually affects the side opposite the damage because the nerves cross where the medulla oblongata meets the spinal cord. However, there are also cases of paresis on the injured side.
The disease is classified according to the localization of the lesion:
- Right hemiparesis - the most common variant diagnosed in adults and associated with speech disorders; disorders range in severity from mild to severe;
- Left hemiparesis – occurs mainly in childhood as it is one of the symptoms of cerebral palsy; psychiatric disorders occur in this form.
Another classification is spastic hemiparesis, in which only the limbs on one side of the body are affected.

The severity of hemiparesis is divided into:
Hemiparesis is diagnosed using scores depending on the degree of impairment:
- 5 - motor function is fully preserved and muscle strength is normal;
- 4 - range of motion is fully preserved, muscle strength is slightly impaired;
- 3 – motor activity is significantly impaired, but muscles have difficulty overcoming friction, that is, the limb is able to move away from the surface;
- 2 - the movement is minimally preserved and the limb is able to move across the plane without moving away from the surface;
- 1 point - muscle activity is barely perceptible, movement of limbs is almost absent;
- 0 points - no motor activity, complete paralysis.
classification
Muscle weakness is caused by a wide range of pathologies. It can be general (widespread) or localized. The former consists of a state of increased fatigability with constant muscle strength. In the second case, the nerve impulse lines from the CNS to certain muscles are interrupted. In this case, it is important to know the extent of the lesion in order to make a local diagnosis:
- Central motor neuron: Motor area of the cortex, corticospinal and corticobulbar pathways.
- Peripheral Motor Neuron: Anterior horns of the spinal cord, roots, nerves.
- nerve and muscle synapses.
- muscles.
When central or peripheral motor neurons are affected, paresis with reduced muscle strength is observed. The severity can be mild, moderate, pervasive, or paralytic (complete inability to move). Traditionally, paresis is classified according to the location of the lesion and clinical features. In neurology, the following classification is generally accepted:
- Central (spastic). By removing the inhibitory effect of the cerebral cortex on the spinal cord, muscle tone and reflexes increase, and pathological signs and synkinesis appear.
- Peripheral (flaccid). Damage to the peripheral motor neuron leads to disruption of the reflex arc, accompanied by hypotonia and hyporeflexia, muscle wasting, fasciculations are detected on examination.
- Mixed. A combination of spastic paresis below the lesion due to the disruption of the corticospinal pathways and peripheral paresis due to a pathological process in the anterior part of the spinal cord.
Psychogenic pareses that occur without organic causes are differentiated separately, with the conduction pathways of the brain and spinal cord being completely intact. Their development is associated with an impairment of the higher nerve functions. The involvement of individual limbs is important for the diagnosis, which is why several types of paresis are distinguished in the neurological clinic:
Why muscle weakness occurs
Causes of muscle weakness in the limbs
In addressing the question of the origin of skeletal muscle weakness, it is useful to distinguish between the concept of paresis associated with damage to nerve pathways and symptoms caused by defects in synaptic transmission, ie, a muscular lesion. These often include blockage or increased clearance of acetylcholine, primary or secondary muscle pathology, and reflex syndromes. Some of the most well known causes of weakness are.
- Myasthenia gravis.
- Myasthenic syndromes:Lambert-Eaton associated with slow closure of ion channels, familial infantile myasthenia gravis.
- Hereditary paroxysmal myoplegia: Hyper-, hypo- and normokalemia, Andersen-Tawil syndrome.
- Infections:Botulism, tick-borne encephalitis.
- Endocrine Pathology: Hyper- and hypothyroidism, Conn's syndrome, Addison's disease.
- Myopathies: Inflammatory (acute myositis, polymyositis, dermatomyositis), metabolic (including cumulative diseases), mitochondrial.
- muscular dystrophies: Progressive (Duchenne, Becker, Emery-Dreyfus), non-progressive (myotubular myopathy).
- Musculoskeletal disorders:Osteoarthritis, tendinitis, trauma.
- Vascular pathologies: Obliterative arteritis, lower extremity varicose veins, Takayasu disease.
- Poisoning: Phosphorus-organic compounds, carbon monoxide, cyanides, aromatic hydrocarbons (toluene, benzene), plants (hemlock), nicotine, cocaine.
- Taking medication: D-penicillamine, antibiotics, cancer drugs, statins, cortisone, colchicine, chloroquine.
Whole body muscle weakness is provoked by various systemic diseases, poisoning. It occurs in acute and chronic infections, autoimmune diseases and malignancies. Poor physical activity in the elderly, immobilization, and prolonged bed rest are common causes of widespread limb weakness.
Symptoms of tropical spastic paresis
There is progressively increasing spastic paresis of both limbs with plantar flexion reflexes and symmetric loss of vibration sensation in the feet. The Achilles tendon reflexes are often absent. Urinary incontinence and frequent urination are characteristic. The disease progresses over several years.
Suspicion should be raised when there is a characteristic neurological deficit, particularly in a patient at risk. Serological and PCR tests of blood and cerebrospinal fluid and magnetic resonance imaging of the spinal cord are done. If the ratio of HTLV-1 antibodies in CSF to its serum level is greater than 1 or the PCR detects HTLV-1 antigen in CSF, the diagnosis is very likely. CSF protein and Ig levels are usually elevated, and lymphocytic pleocytosis is seen in half of the cases. Spinal cord foci may be visible as bright areas on weighted MRI.
[10], [11], [12], [13], [14], [15], [16]
Treatment
As a rule, clear muscle complaints are always regarded as the main symptom of paresis. If left untreated, a serious condition such as paresis can progress to complete paralysis. In most cases, patients experience severe pain at the site where the muscles are partially paralyzed. However, if the disease is accompanied by other acute diseases, then it develops quite quickly, and treatment is prescribed on this basis.
The main treatment is usually the initial identification and further elimination of the underlying cause of the disease. It is not uncommon for paresis to appear as a result of various pathologies. Strokes are always treated with special rehabilitation therapies. With injuries and other trauma, specialists perform the inevitable sutures on the peripheral nerves. If tumors or other growths are found that are putting significant pressure on the nerves, surgery is recommended to remove them.
Among other things, specific massages are often indicated to maintain muscle tone, since the muscles can atrophy due to constant partial immobility. Treating the different types of paralysis depends on the will and determination of the patient. The patient must have the will to recover in order to activate the body's inner power.
Complications of Multiple Sclerosis
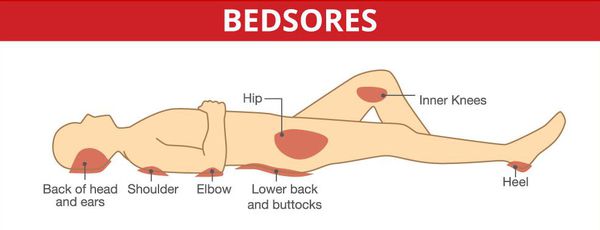
Decubitus ulcers and disorders of the deep pelvic organs are serious complications, especially in spinal forms.
Acute and subacute cases with damage to significant parts of the brainstem can also be unfavorable.
The neurological condition of the patient is directly related to his immune system. Often there is increased fatigue, muscle weakness and dizziness. As the stage progresses, one notices ataxia (coordination and voluntary disorders), a significant reduction in physical and especially motor performance of the limbs with the development of spasticity (movement disorders as a result of increased muscle tone).
Very often, visual acuity decreases rapidly, there is a loss of clarity, the field of vision is reduced, color distortions appear, diplopia, amblyopia and strabismus develop.
Patients are often irritable, have mood swings, in some cases euphoria, and have inappropriate attitudes about their illness.
Cognitive impairments with memory, concentration and spatial orientation problems are not uncommon in MS.
MS also causes abnormalities in the pelvic area, such as B. delayed urination and persistent constipation, and the patient then loses control of emptying the bowel and bladder. The incomplete emptying of the bladder leads to urological diseases up to urosepsis.
The above complications require special attention as they can be fatal to the patient. [15] [16]
Diagnosis of multiple sclerosis
If MS is suspected, an MRI scan of the brain and spinal cord should be performed in addition to a full neurological exam. This examination is the most meaningful additional diagnostic method. It can reveal areas of altered density in the brain's white matter (foci of demyelination and gliosis). [10]

Visually evoked potentials can also be an early diagnostic criterion to determine the degree of preservation of certain pathways.
Isoelectric focusing, with which oligoclonal IgG groups can be isolated, is considered to be meaningful in CSF examination.
The criteria proposed by the International Expert Group are widely used to diagnose MS. [11]
Causes of paresis.
There are 2 types of specific neurophysiological symptoms: organic and functional. In organic paresis, the physical connection between the muscles and the brain is broken, resulting in reduced mobility of the limbs. With functional paresis, the characteristic feature is the destruction of the gray matter substance. Depending on the area affected and the degree of severity, it is classified according to the type of localization: Tetraparesis: leads to muscle weakness. It manifests itself in increased muscle tone, which immobilizes the patient. This type can be caused by chronic diseases, circulatory disorders and trauma after neurosurgical treatments. The weakness of all limbs arises from a deterioration in the blood supply to the nerve fibers. Sometimes the metabolism in the nerve tracts of the gray matter is also disturbed. Paraparesis: affects the arms or legs on both sides of the body at the same time as brain damage. It is caused by tumors: it also arises from osteochondrosis and spondylosis. Hemiparesis: In this form, only half of the body falls out. Strength then decreases: it is replaced by muscle defects in the upper and lower limbs. Hemiparesis is usually aggravated by conditions such as bleeding, tumors, head injuries, and diabetic encephalopathy. Monoparesis: This condition involves muscle weakness in one of the limbs. A similar disorder is caused by Brown-Sekar syndrome. Causes of this type of disorder include inflammation of the intracranial substance, botulinum toxin poisoning, head trauma, spinal cord injury, abscesses, and stroke.



paresis of the feet.
Occurs when attempting to bend the knee. Difficulty flexing and extending the thigh and tibia can be seen with the naked eye. This is due to weakness of certain muscle groups with normal dynamics in the distal parts. Traumatic factors affecting the integrity of the thigh fibers often cause peripheral proximal unilateral paresis. Mononeuropathy of the femoral nerve can cause loss of sensation on the outside of the leg and the front of the tibia. The muscles become very tense and limit their mobility. Extension of the lower limbs is difficult. As this type of paresis progresses, the personal or shin muscle group becomes damaged. Movement of the foot is impossible and walking is impaired by dysfunction of the oculomotor nerve. When stepping on the heel, the patient is unable to lower the foot and raise the outer edge. On the inside, the feel is compromised. In the absence of timely and professional treatment, a 'cutter foot' develops. Severe traumatic consequences can lead to significant problems with the tibial nerve. Symptoms include difficulty flexing the sole, foot, and hand. The affected person cannot stand on their toes and the Achilles reflex disappears. With progressive paresis, trophic ulcers may appear. Feeling in the plantar region and on the outer edge of the sciatic nerve is also affected. Sciatic nerve disease is often the result of trauma. When the extent and depth of the injury is large, bone loss in the hip is inevitable. As a result of destruction, sciatic nerve mononeuropathy progresses. If the nerve endings are completely lost, complete immobilization can occur. However, the outer surface of the thigh remains intact and tender. The ability to perceive tactile stimuli on the posterior surface as well as on the soleus surface is significantly reduced.
As the paresis worsens, the variability and level of dynamic movement decreases, which is easily detected with a simple handshake. It is not uncommon for muscle dysmotility to occur without a clear cause. The acute course of the disorder is signaled by a pronounced pain syndrome. Disorders in which nerve fibers are disrupted are often the result of a traumatic complication. Disorders in the distal area are referred to as 'Dazherin-Klumpke palsy'. Problems of this type can occur as a result of trauma to the child's shoulder joint during childbirth. With this type of strain, the immobilisation also extends to the hands. The injured person is unable to form a normal fist or open and close their hand as the small, soft structures of the hand dissolve. With paresis with a tear of the ulnar fiber, there is acute pain in the muscles involved in extension of the hand and elbow and loss of working capacity. The little finger is affected. Untimely treatment can lead to atrophy and hypotension. In appearance, the hand resembles a clawed paw. The fingers are unflexed in the main limbs and curved in the other limbs, and paralyzed muscles predominate. The symptoms of the disease are accompanied by a significant progression of polyneuropathy (nerve damage).
Types of paralysis and their symptoms
Depending on which part of the body is affected, a distinction is made between the following forms monoparesis (a part of the body), paraparesis (symmetrically arranged body parts, e.g. both arms), hemiparesis (both limbs on one side), tetraparesis or total paresis (all limbs)..
The cardinal symptom of any type of paresis is muscle weakness and difficulty in movement. In addition, patients may complain of pain when attempting to move the affected arm or leg, muscle spasms, and rapid fatigue. With central paresis, there is an increase in reflexes and muscle tone. In the case of peripheral paresis, on the other hand, there is muscle relaxation up to and including atony.
Diagnosis and treatment of paralysis in the elderly
The first stage of diagnosis is a neurological examination with assessment of muscle function. In this way, the specialist determines the presence of paralysis, determines the degree of its development and distinguishes between central and peripheral paralysis. Electroneuromyography to assess the speed of impulse conduction along nerve fibers, computed tomography, or magnetic resonance imaging is recommended after the examination. If an inflammatory reaction is suspected, a general blood test may be required.
Paralysis is treated conservatively; surgery is required only in the presence of a tumor and complex trauma. After a thorough diagnosis, the patient is prescribed various groups of drugs – neuroprotectants, drugs that improve blood supply to the cerebral vessels. Muscle relaxants may be prescribed for central paresis to reduce excessive muscle tension. Taking B vitamins is mandatory. Magnesium can be given to relieve seizures. To alleviate the patient's condition, the following measures are recommended. Physiotherapy, massages, physical therapy.
Preventing senile paralysis consists of getting enough exercise and avoiding physical inactivity. Eating a balanced diet and avoiding bad habits and excess body weight are important.
Clinical Signs of Intramedullary Brachial Plexus Injury
Absence or limitation: in the hand and fingers
Isolated upper limb peripheral nerve palsy, usually of traumatic origin, is most common in the postnatal period. Isolated radial nerve palsy is the most common and results in unilateral limitation of active hand movements. Isolated damage to the ulnar nerve most often occurs as a result of local trauma and is accompanied by a decrease in the strength of the adductors and adductor muscles of the fingers and, in severe cases, the development of claw deformity of the hand. However, in most cases, the neurological deficit in children resolves within 10 days to three months with conservative treatment.
Treatment of flaccid paralysis in children and adolescents
Traumatic injuries of the peripheral nerve:
- Clinical and neurological assessment of the injury. Monthly follow-up by a neurologist and medical-neurological treatment.
- Instrumental methods: ENMG, ultrasound, MRI, CT to clarify the extent of the lesion and its location. ENMG in dynamics once every 3 months.
- Observation by orthopaedists, physiotherapists and physiotherapists once every 3 months.
- Prescription of a functional orthosis to prevent contractures and a number of rehabilitation treatments (massage, physical therapy, physiotherapy).
- Defining the indications for neurosurgical interventions.
- Determination of the indication for an orthopedic operation. When conservative and neurosurgical treatments are ineffective, diagnosis of nerve damage is late (2 or more years after injury), muscle wasting and contractures occur, and limb dysfunction is present, orthopedic surgery is indicated.
- Sanatorium treatment in neurological and orthopedic sanatoriums once a year.
Intrinsic brachial plexus injury
The rate of functional return of the upper limbs in patients with intrinsic brachial plexus injury is relatively high (up to 90 %), but due to neurological deficits, some patients develop impairments in balance and muscle function as early as 2 to 3 years of age, which can be found in lead to osteoarticular deformities and severe movement disorders. The most commonly observed anatomical and functional abnormalities involve the shoulder and elbow joints.
Children with an intra-articular injury of the brachial plexus develop severe anatomical changes of the humeral head and scapula as they grow if measures are not taken to prevent contractures of the upper limbs. The first changes in the brachial plexus are noted at the age of 3-5 months, pronounced changes already at the age of 2 or 3 years.
Read more:- paresis of the lower body.
- paraparesis.
- paresis is.
- Paraparesis - what is it?.
- Lower spastic paraparesis.
- A wobbly gait means.
- Syndrome of the tibial nerve.
- Charcot-Marie foot.
