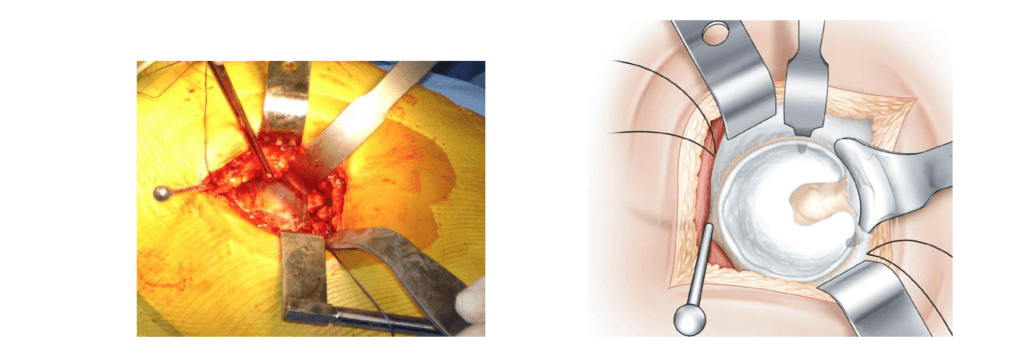
Using wire tensioners reduces tension and avoids interposition. Once the prosthesis is in place, the tendon of the sternocleidomastoid muscle is repositioned. It lies obliquely on the rear upper part of the acetabular component of the prosthesis.

- Femoral artery bypass surgery: indications and contraindications, course of surgery and rehabilitation
- Contraindications and possible complications
- Stages of treatment of open wounds
- Primary self-healing.
- inflammation
- Granulation tissue repair
- Basic wound care
- Preparing for shin augmentation surgery with implants
- Carrying out plastic surgery
- Postoperative period and complications
- Exposure of the acetabulum. (L'exposition du cotyle)
- Preparation of the hip socket. (La preparation du cotyle.)
- forecast
- After the operation. rehabilitation
- Possible consequences or complications
- Phlebectomy
- How is a phlebectomy performed?
- Leg vein removalThe prices are low and the quality is high!
- Exercise therapy after phlebectomy – only from our specialists!
- Disadvantages of surgical removal of foot nodules
- After removing the stitches
- Signs of inflammation and other complications
Femoral artery bypass surgery: indications and contraindications, course of surgery and rehabilitation
During the preparation, premedication and prophylactic administration of antibiotics to inhibit the natural saprophytic flora are carried out.
Traditionally, two approaches to the aorta are used - laparotomy or Robb's incision retroperitoneal. The latter method is most commonly used because it avoids injury to the intestines and reduces the risk of femoral nerve damage.
Once the artery is accessible, a shunt made of inert material is sewn into the area free of atherosclerotic plaque. The diameter of the shunt is adjusted to the lumen of the artery. The other end of the shunt is sewn into longitudinal incisions in the femoral artery. If the shunt connects the aorta and one of the femoral arteries, it is an aorto-iliac bypass; If the shunt connects the aorta to two femoral arteries at the same time, the operation is called aorto-iliac bypass.
Contraindications and possible complications
Femoral artery bypass surgery is a technically complex and risky surgical procedure that requires general anesthesia. For this reason, there are a number of contraindications to the procedure, the main of which are.
- Severe cardiac conduction and rhythm disorders in the patient;
- Stroke or myocardial infarction in the recent past
- severe liver and/or kidney dysfunction;
- coronary heart disease;
- coagulation disorders and other blood diseases;
- presence of a malignant disease;
- decompensated chronic obstructive pulmonary disease;
- Anatomically-related lack of access to the aorta (e.g. severe peritoneal fibrosis, colostomy, horseshoe kidney).
Surgical intervention is not possible if the floor of the iliac artery is severely occluded and the insertion of a shunt does not help normalize blood flow. If femoral artery replacement is not possible for certain reasons, an endovascular (intravenous) procedure such as: B. stenting is carried out.
Like any operation of this complexity, femoral artery bypass surgery carries the risk of complications. One of the most common and completely reversible complications is the accumulation of lymph fluid in the area of the procedure and severe tissue swelling.
In some cases it may be necessary to remove the fluid. The swelling usually subsides 7-10 days after the procedure.

More serious complications include:
- development of a heart attack or stroke;
- Hemorrhage
- Formation of false aneurysms;
- sclerosis of the prosthesis with the development of sepsis;
- Occlusion of the vascular prosthesis.
Stages of treatment of open wounds

Healing of an open wound takes place in 3 phases:
Primary self-healing.
Bleeding occurs immediately after the injury. The vessels contract quickly, allowing blood clots to form and stop bleeding. The vessels then expand and the permeability of their walls increases, causing swelling to form in the injured area.
This endogenous reaction helps the soft tissues clean themselves without the need to use disinfectants.
inflammation
The second phase is accompanied by an increase in tissue swelling. The skin turns red. A large number of white blood cells accumulate in the injured area.
Granulation tissue repair
Granulation tissue repair may occur in association with inflammation. This is a completely normal phenomenon. Granulation covers the entire wound surface, including the edges and surrounding tissue.
The granulation tissue then develops into connective tissue fibers. This process culminates in the formation of a scar.
A wound can heal with primary and secondary tension. If the injured area is small, the edges are close together, and there is little inflammation, tension is primary. In all other cases, healing is characterized by secondary tension.
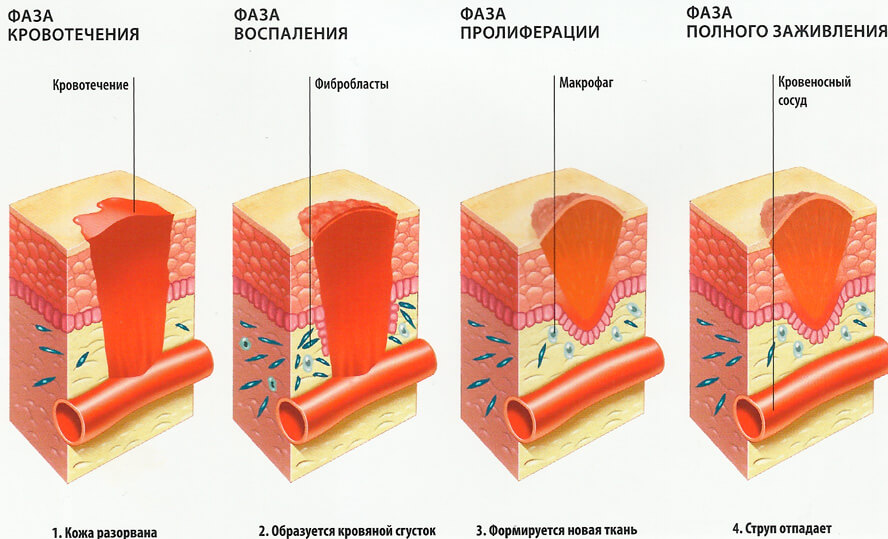
The specific treatment of an open wound depends directly on how intense the inflammatory reaction is and how much tissue has been injured. It is important to stimulate and control all phases of healing.
Basic wound care
First aid treatment of the wound is a must. If it is a small incision made at home, all debris should be removed. This can be done with the sharpened end of a sterile bandage or with tweezers (these should be treated with an alcohol liquid).
Once the wound is free of debris, it should be washed with an antiseptic solution. 3% hydrogen peroxide, iodynol, chlorhexidine, etc. can be used. Hydrogen peroxide helps push out the smallest contaminants as bubbles form on the wound after its use. At the same time it destroys the pathogenic flora. If no remedy is available, a 2% solution of soda, a solution of concentrated salt, vodka or chamomile can be used. It should be clear that there will always be germs in the wound unless the incision was made with a sterile instrument.
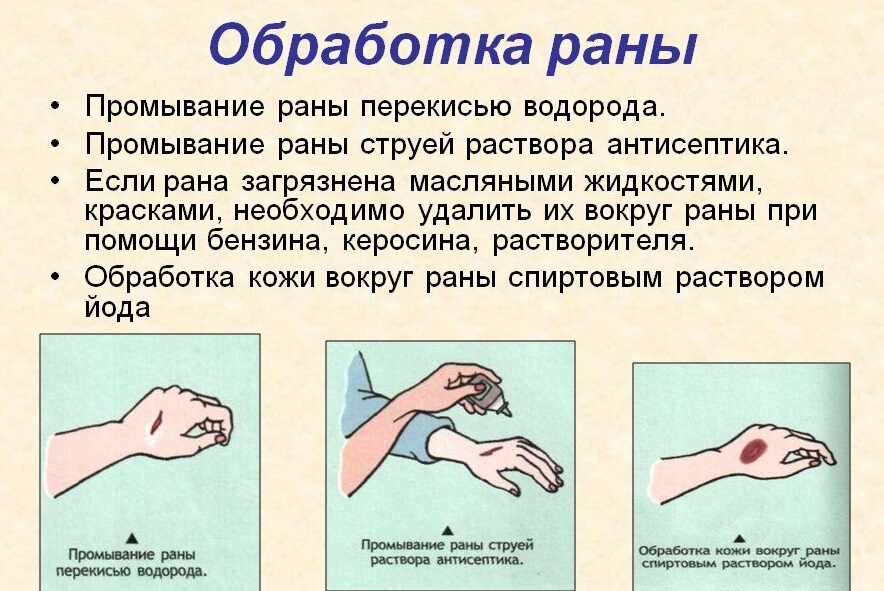
Household wounds are susceptible to infection. Sometimes germs even begin to multiply in surgical wounds. This is why it is important to cover the injured area after an injury. To do this, it is bandaged or covered with a plaster. Only small scratches and superficial cuts should be left open.
Preparing for shin augmentation surgery with implants
The first step to the operation is a conversation with the doctor and an initial consultation. During this conversation, the doctor must assess the patient's psychological state, how he feels and how he would like the operation to proceed.
If a true curvature of the legs is suspected, an X-ray or CT scan is taken: the doctor must be convinced that it is a false curvature in order to perform a crossplasty. If this is confirmed, a 3D simulation is carried out on the computer: the patient can then see what his enlarged lower leg will look like after the operation [8].
A series of examinations must be carried out before the operation. These include a general blood test, a biochemical test, an infection test, a blood sugar test, a urine test and an ECG. Doppler ultrasound of blood vessels is performed to clarify the nature of blood flow in the lower limbs. The patient also speaks with the anesthetist and is consulted by a specialist if necessary (9).
The implants are also selected in preparation for the crossplasty. Their main material is silicone, which makes the implants flexible and natural looking. The key to the success of the operation is the correct choice of size and shape.
The implants can be symmetrical or asymmetrical. A symmetrical implant is as thick as possible in the middle and is shaped like a lens. An asymmetrical implant has more volume in the upper third and looks like a blob. The choice of implant for a particular patient depends on shape, volume and height, and prior computer modeling helps to make this choice as predictable as possible [10].
Carrying out plastic surgery
The actual tibial implant surgery takes between 40 minutes and an hour. Before the operation, the surgeon determines the position of the implant and the incision. The patient is then taken to the operating room, where the legs are treated with an antiseptic.
Croplasty does not require general anesthesia: it is performed under spinal anesthesia, and if the patient wishes, sedation can also be used, that is, the patient is asleep. The surgeon makes a 3-4 cm long incision in the back of the knee so that the suture is as inconspicuous as possible. Under the connective tissue covering the muscle (fascia), a so-called implant pocket is created - a space that corresponds to the size of the implant into which it is inserted. The surgeon then sutures the wound [11] and the patient receives a compression garment.
Cruplasty can also be performed simultaneously with liposuction of the knees or hips for an even greater effect [12].
Postoperative period and complications
After the operation, the patient remains in the hospital for about a week, after which the stitches are removed. He will have to wear a pressure bandage for a month, which will remain in place for the duration of the operation. After the operation, the patient remains in the hospital for about a week, after which the stitches are removed, They should be of good quality and fit perfectly.
Conservative therapy As part of conservative therapy, anti-inflammatory drugs and phlebotropic substances are prescribed to improve blood circulation and speed up recovery.
Physical activity plays an important role in limb vein pathology Physical activity and early stimulation of the patient play an important role in preventing thrombosis and restoring microcirculation. Walking and special exercises are helpful, but prolonged sitting or standing in a position that increases venous congestion should be avoided.
Complications after a crossectomy are relatively rare, but still possible. The most likely cause is the traumatic nature of the procedure and errors in the surgical technique. Complications include:
- bleeding in the area of the procedure;
- bleeding;
- burning of the surgical wound;
- Disturbance of lymphatic drainage and cyst formation (lymphocele);
- Decreased and altered skin sensitivity (if nerve endings are damaged).
Most of these lesions resolve spontaneously, but some (abscesses, hemorrhages) may require additional treatment. Fortunately, serious sequelae in the form of deep clots and progressive thrombophlebitis are extremely rare.
If urgent phlebectomy is required, the modified Trojanov-Trendelenburg operation is the only treatment option without alternative, the disadvantage of which is the need for hospitalization and constant monitoring of the patient.
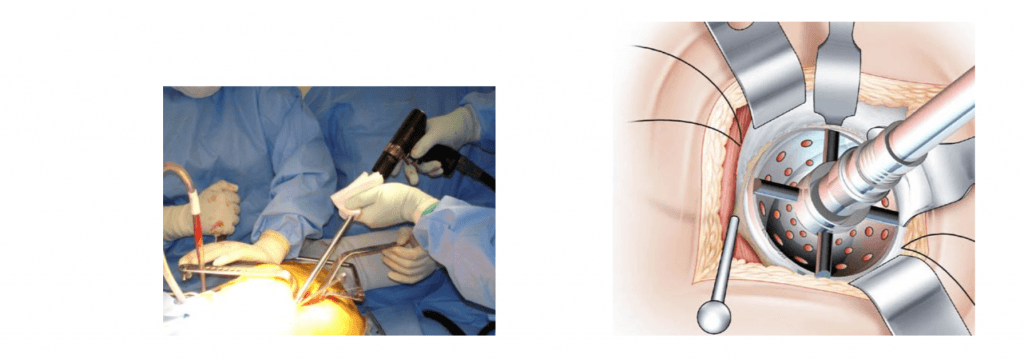
Exposure of the acetabulum. (L'exposition du cotyle)
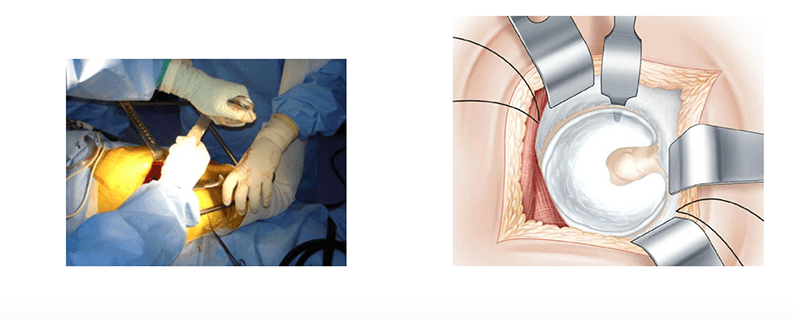
The three retractors are arranged in a circle to allow access to the socket. The position of the leg changes each time, making positioning of each retractor easier. The curved retractor is placed blindly by feel. Its end is inserted deep into the acetabulum to capture the edge of the anterior horn after piercing the capsule at the bone level.
The leg remains in a retracted position.
The tendon of the sternocleidomastoid muscle and the severed edge of the capsule are raised upward. This is the most delicate part of the operation. The position in which the leg is pulled back allows the tendon to release tension. Once the edge of the joint capsule is retracted, the hip socket is exposed. The space between the joint capsule and the hip socket is cleared. Fixation is done with a Stenmann nail, which is placed 1-2 cm above the hip socket.
The leg is placed on a footrest and turned inwards. Hochmann hooks are placed under the dorsal horn after perforation of the joint capsule. The Stenmann nail, placed vertically at the posterior edge of the acetabulum, provides the necessary protection for the sciatic nerve.
Preparation of the hip socket. (La preparation du cotyle.)
After the hip socket has been split, it is milled as usual. Insertion occurs between the anterior and inferior retractors.
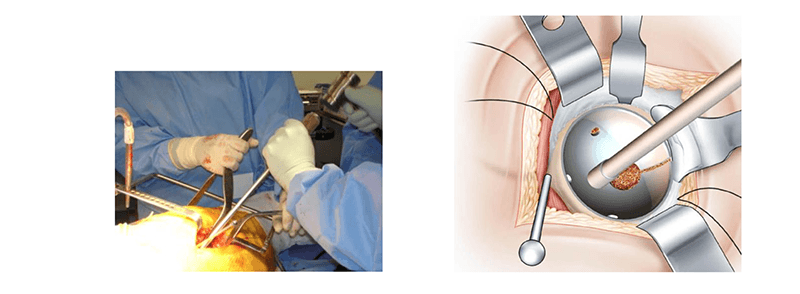
The acetabular component is fixed in the same way. The introduction of wire hooks avoids interposition.
forecast
Phlebectomy has good cosmetic results, is effective in treating varicose veins, and carries a low risk of serious complications. If the phlebectomy is performed by a qualified doctor under appropriate conditions, the long-term success rate is 90 %. As the bruising subsides after the operation, the varicose veins will noticeably disappear. Because only small incisions are made, there are no visible scars and most patients are happy with the results.
A traditional classic phlebectomy is rarely necessary for patients as it usually requires an overnight stay in the hospital and 2 to 8 weeks at home.
After removal of veins in the lower limbs in our center, the patient can exercise, but driving is not recommended for at least 24 hours as distal motor function may be impaired due to prolonged anesthesia, especially after anesthesia in the hamstring area. The patient is recommended to walk for about 10-15 minutes before leaving the clinic.
Diosmin (Detralex) should then be taken and it is not advisable to stand in one place for 2 weeks. This helps minimize the risk of blood clots forming in the deep veins of the legs. The compression bandage prevents secondary bleeding and reduces the likelihood of pain, bruising and other complications. The bandages will be removed 3-7 days after surgery, but the compression stocking should be worn for another 2-4 weeks to minimize bruising and swelling. The length of time it is worn depends on the size of the veins removed and the degree of reflux treatment. The stocking can be taken off when showering.
Further sclerotherapy should be postponed for a few weeks and only carried out after the postoperative swelling has subsided. Many spider veins can regress spontaneously and also disappear spontaneously after varicose vein removal through outpatient phlebectomy. Early sun exposure should be avoided due to possible hyperpigmentation at the puncture or incision site.
After the operation. rehabilitation
After vein removal, the patient remains under the supervision of a doctor who assesses the patient's recovery and rehabilitation period. Doctors focus on the patient's general condition and any chronic illnesses that could affect recovery.
After the venectomy, the patient remains in the inpatient ward. Antibiotic therapy is indicated to avoid complications. Doctors also prescribe painkiller injections and phlebological treatment.
Complete rehabilitation is possible only if the patient follows a few simple rules. Shortly after surgery, you should be able to bend your lower limbs and attempt to turn in bed. The legs should be elevated to improve blood circulation.
After 24 hours, you should get out of bed and start moving around the room. Your legs should always wear compression clothing.
Post-operative massages and physiotherapy exercises, which are usually recommended by your doctor, are important. These measures prevent the formation of blood clots.
Venenectomy patients should not bathe in hot water or undergo other warming procedures, including bathing.
Rehabilitation consists of applying compression material 24 hours a day for a month. The limbs are then bandaged for just one day.
The sutures after the venectomy are removed after nine days. Of course, patients are not allowed to undertake any physical exertion during this time.
One week after the procedure, the patient is discharged from the inpatient department, but longer outpatient follow-up care is indicated. Six months later, an ultrasound scan of the blood vessels is performed to detect possible recurrence or to confirm that there is no recurrence.
Possible consequences or complications

Venectomy, like any other surgical procedure, can lead to various complications. Most of these occur in the first few days after surgery. For example, surgery can be complicated by heavy bleeding. Sometimes subcutaneous nerves are damaged during surgery, resulting in decreased sensitivity in certain areas. If a hematoma has formed as a result of surgery, it can develop into an abscess.
Other possible complications include numbness in the lower leg or ankle, pain and subcutaneous effusions (bruising).
Deep vein thrombosis is an extremely rare complication.
The treating doctor decides on the feasibility and safety of a venectomy on a case-by-case basis.
Phlebectomy
 It is important to know that surgical removal of varicose veins is only indicated if conservative measures can no longer be expected to be successful. This means that without removing the varicose veins you cannot stop the progression of the disease.
It is important to know that surgical removal of varicose veins is only indicated if conservative measures can no longer be expected to be successful. This means that without removing the varicose veins you cannot stop the progression of the disease. This means that without removing the varicose veins, the development of venous insufficiency cannot be stopped, the risk of life-threatening blood clots can be eliminated, or trophic ulcers can be avoided. At this stage of the disease, conservative treatment (wearing compression stockings, taking phlebotic medications) can only slow down the progression of the disease, but not stop it. The more advanced the lesions are, the more difficult they are to treat. Therefore, surgical removal of varicose veins should not be postponed.
This means that without removing the varicose veins, the development of venous insufficiency cannot be stopped, the risk of life-threatening blood clots can be eliminated, or trophic ulcers can be avoided. At this stage of the disease, conservative treatment (wearing compression stockings, taking phlebotic medications) can only slow down the progression of the disease, but not stop it. The more advanced the lesions are, the more difficult they are to treat. Therefore, surgical removal of varicose veins should not be postponed.

The already proven techniques for varicose vein removal are constantly being improved and new techniques are being developed in parallel. However, despite the development of modern minimally invasive techniques for the treatment of varicose veins (sclerotherapy, endovascular laser photocoagulation, radiofrequency current ablation), phlebectomy - the surgical removal of varicose veins - remains a commonly used procedure to eliminate the disease.

Phlebectomy is one of the first procedures to treat varicose veins, which involves surgically removing the area of the vein affected by the varicose veins to restore normal blood flow. It is important to know that in this medical procedure only the subcutaneous veins are removed, through which only 10 % of blood flows, so this varicose vein surgery is completely safe for the deep veins and the circulatory system as a whole. Phlebectomy is often referred to as 'cosmetic surgery' because it not only improves blood circulation but also has a positive effect on the appearance of the legs.
How is a phlebectomy performed?
The operation is carried out using special probes. First, the blood vessel affected by the varicose veins is tied and cut at the point where it opens into the deep vein, then the leg veins are removed: a so-called guide probe is inserted through the incisions into the vessel and the area is pulled out. All procedures are carried out through small incisions, which are later covered with cosmetic sutures so that the postoperative marks are inconspicuous. In some cases, no sutures are used at all and the cut edges are taped together with special plaster strips. When carrying out the Miniflebectomy The procedure is carried out through punctures in the skin, which heal spontaneously and practically without leaving a trace. Phlebectomy is usually performed in the hospital in one day without the need for a long hospital stay. This is an undeniable advantage.
Removal of leg veinsPrices are low and quality is high!
If you suspect you have varicose veins, you should see your doctor immediately. In the early stages, conservative treatment methods can still be used:
However, surgical removal of the leg veins is often necessary. The prices in our clinic are very affordable. You can probably afford it. In addition, the operation itself is relatively easy for the patient.
Exercise therapy after phlebectomy – Only from our specialists!
Our clinic does not abandon patients immediately after the operation. We offer therapeutic exercises after a phlebectomy to quickly restore function and allow you to return to your daily activities.
We have the best physical therapists to work with you. You will find a range of exercises tailored specifically to you. They will also always be there to help you with advice on how to deal with any situation and the best way to get your feet back to health.
If you listen to them, you will quickly return to your normal rhythm of life. You will continue to enjoy every minute - because now you have completely healthy feet! Our specialists will do everything to achieve this goal! Contact us and see for yourself!
Disadvantages of surgical removal of foot nodules
Before you decide to have surgery, you should keep in mind that you will be unable to work for 1-2 months after the operation. During the rehabilitation phase he will only be able to move around on crutches.
You should also be prepared for any pain sensations after the procedure. These can be treated with painkillers. Therefore, the decision whether to surgically remove nodules in the legs should be made carefully. Other treatment options should be discussed with your doctor.
After removing the stitches
If self-absorbable suture material was not used during the operation, it must always be removed by the doctor. Even after the operation, the patient should follow some recommendations for successful healing:
- The wound must not be watered for the first 24 hours.
- Protect the fresh scar (for 2 weeks) from all kinds of mechanical influences.
- Do not expose the scar to ultraviolet radiation for 2 months after treatment. In the long term (up to six months), it is advisable to protect the skin in this area with special creams with a high sun protection factor.
- Silicone-containing and other preparations that can improve the appearance of the scar and make it less visible should be used.
The final scar on the skin does not form until six months after the procedure. All cosmetic procedures to correct the scar on the body can only be carried out after this period.
Signs of inflammation and other complications

The suture does not always heal safely after the operation. This process can be disrupted by a number of factors. Patients should always seek immediate medical attention if:
- The scar is red, swollen, or feels hot.
- The pain in the wound area increases and twitches.
- Purulent or fecal discharge comes from the wound.
- Blood oozes from the wound.
- A foul smell comes from the wound.
- The general body temperature rises.
The above symptoms should definitely not be ignored as they may indicate severe inflammation and other complications. Post-operative infections can develop very quickly, so you should not hesitate to see a doctor.
Read more:- The lateral side is.
- Injury to the ankle.
- Hip Amputation Surgery Code.
- The child has a shorter leg than the other.
- Technique of tibia amputation.
- The reamputation is.
- How to amputate a leg.
- Where do the body parts go after the operation?.
