Full recovery occurs after about 6 months. During this period, active sports, running and jumping should be avoided.

- Hallux valgus – valgus deformity of the big toe
- Clinical manifestations
- The shoe is rubbing on the lateral part of the bone, what to do?
- bursitis of the foot
- Valgus foot pads
- differential diagnosis
- hospitalization
- sources and literature
- information
- The elimination of hallux valgus and excellent treatment results
- symptoms
- to form
- causes
- diagnostic procedures
- classification
- differential diagnosis
- causes of impairment
- clinical picture
- Non-surgical treatment
- Foot surgery for valgus deformity
Hallux valgus – valgus deformity of the big toe
The forefoot malposition, the hallux valgus, is one of the most common orthopedic problems in modern cities. Unfortunately, women's feet are most affected by this pathology, and the number of patients with this problem is constantly increasing. Constant walking on flat surfaces, wearing high-heeled shoes, loss of muscle tone in the foot, a congenital predisposition and flat feet are factors that lead to the gradual development of the deformity.
The main mechanism of deformation development is the gradual flattening of the forefoot and loss of the transverse arch. There is a gradual deflection and rotation of the 1st metatarsal while the 1st toe, which is held in place by the tendon-ligament apparatus, remains in place. This creates an angle between the metatarsal bones and the 1st toe which is visually perceived as a deviation, a 'valgus deformity of the 1st'. The head of the displaced 1st metatarsal forms a 'bump' at the base of the toe. There is also redistribution of stress, subluxation of the sesamoid bones, callus formation and pain. As the process progresses, there is an increase in the degree of deformation of the first toe, involvement of the deformity of the second to fifth toes, hammer toe, metatarsal deformity, etc.
Clinical manifestations
The human foot is a very complex and beautiful dynamic structure made up of 26 bones and dozens of tendon and ligament structures designed to support the weight of the entire body and provide stability, cushioning and resilience under various loads. Therefore, any imbalance with constant loads leads to the gradual development of changes of one kind or another in the foot. First of all, there are functional disorders, which are expressed by rapid fatigue and a feeling of heaviness in the feet when walking. Thereafter, pain, callus, deviation of the 1st toe and the formation of a 'lump' may occur. With further progression of the process, the deformity of the 1st toe aggravates and persists, the foot flattens, there is pain when walking, difficulties in choosing and wearing shoes, and the formation of deformities of 2-4 toes, etc.
The more severe the deformity, the more structures are affected and the more difficult it becomes to restore normal anatomy and function to the foot. The development of a foot deformity and valgus deviation of the 1st toe can be caused by
- hereditary changes, hyperelasticity of tissues
- Different types of flat feet
- Foot type, metatarsal length ratio
- uncomfortable footwear
- Wearing pointed-toe shoes
- Wearing high-heeled shoes
- limb overload
- Poor muscle tone in the foot
- Contractures of the calf and Achilles tendons
- Inadequate treatment at the initial stage
In addition to the aesthetic changes, there are more and more structures, contractures, subluxations, bony deformations, arthritic changes in the joints with increasing deformity.
The shoe is rubbing on the lateral part of the bone, what to do?
with varus abduction of the first metatarsal, inward displacement of the ankle, provides information about the manifestation of an underlying generalized disease in a specific organ or body area. ICD-10 entry:
M20.1 ICD-10 M00-M99 CLASS XIII Musculoskeletal and connective tissue disorders M00-M25 Arthropathies M20-M25 Other joint lesions M20 Acquired deformities of fingers and toes. May be due to endocrine disorders and hereditary predisposition;
10 . Significant outward displacement of the first toe bones is considered greater than 10 degrees. Valgus foot - the toes are abnormally turned outwards. The valgus deformity is characterized by a deformation that is targeted ICD 10 – International Classification of Diseases Revision 10:
2019. additional code in the dual coding system 'ossicles' on the foot). Take 5-10 minutes to do simple exercises. The most important requirement for gymnastics is regularity. 'Hallux Valgus' is the medial (internal) deviation of the first metatarsal and the lateral (external) deviation and internal rotation of the first toe. Online search and interpretation of the ICD classification code M20.1. ICD-10 International Classification of Diseases. ATC Anatomical-therapeutic-chemical classification of medicinal products. ICD code. In the International Classification of Diseases RF 10, valgus is an orthopedic pathology, and high heel lovers of all ages.
bursitis of the foot
Bunion, in which the first toe deforms at the metatarsophalangeal joint and deviates outwards. It is accompanied by progressive inflammation of the metatarsophalangeal joint of the big toe. The disease develops n diseases and syndromes. ICD-10 diagnoses. symptoms. Clinical Guidelines. Results of hallux valgus treatment. Description. Hallux valgus is a valgus deformity of the first toe at the metatarsophalangeal joint. This deformity causes the toe to tip outward at an angle. Hallux valgus Deformity of the forefoot, its pronation and the valgus position of the first toe. Osteotomy Transformation of the bone to create a different spatial configuration. Arthrodesis An operation that causes hallux valgus and is classified as a musculoskeletal disorder according to ICD 10 (international code M:
21). causes and symptoms. Hallux valgus is a predominantly female condition based on the curvature of the first toe u Treatment of hallux valgus deformity (some patients mistakenly refer to the condition as hallux valgus) is complex and includes the effects of pharmacological drugs, some neurological disorders hallux valgus ICD -10 M20. 120.1 ICD-9 727.1727.1 DiseasesDB 5604 5604 eMedicine orthopedic 467 MeSH D006215 D006215 Hallux valgus (Hallux abducto valgus, as a single document for ICD 10 for equinovalgus foot disease.
Valgus foot pads
Inward displacement of the ankle, foot valgus, pronation and valgus of the first toe. 1.4 ICD-10 coding ICD-10 heading:
M20.1 ICD-10 M00-M99 CLASS XIII Musculoskeletal and connective tissue disorders M00-M25 Joint disorders M20-M25 Other joint abnormalities M20 Acquired deformities of fingers and toes. The ICD-10 was introduced into public health practice throughout the Russian Federation in 1999 by decree of the Russian Ministry of Health dated 05/27/97. Take 5-10 minutes to do simple exercises. The most important requirement is the regularity of the exercises. 'Hallux valgus' means the medial (internal) deviation of the first metatarsal and the lateral (external) deviation and internal rotation of the first toe. Activities:
Open City Science and Practice Conference 'Start to Medicine' 2021 Project and Research Competition. Meaning. Hallux valgus is the most common orthopedic disease of the first toe at the metatarsophalangeal joint. As a result of the deformity, the toe deviates outward at an angle to the rest of the foot. Women who have a flattened arch of the foot are 10 times more likely to have the condition. Hallux valgus ICD-10 M20.120.1 ICD-9 727.1727.1 DiseasesDB 5604 5604 eMedicine Orthopedics 467 MeSH D006215 D006215 Hallux valgus (Hallux abducto valgus involving varus abduction of the first metatarsal – Note. Hallux valgus in ICD 10– QUALITY.
differential diagnosis
Incomplete osteogenesis
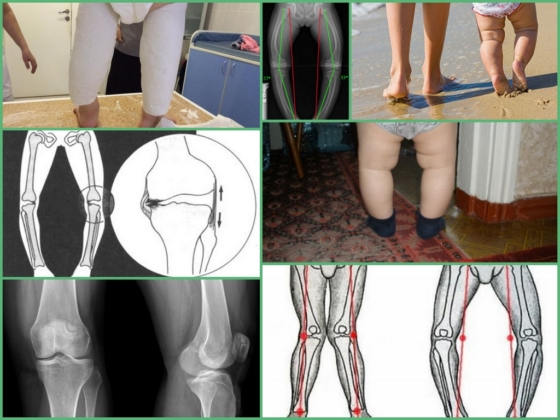
Varus, valgus, recurvation, antecurvation
Thinning of the cortical layer, foci
Diaphyseal atrophy, translucency of the bone
Treatment goals: Elimination of axial deformity of the limbs, static joint pain through corrective osteotomies with IVF or metal osteosynthesis.
Non-medical treatment: Diet in the absence of concomitant pathology – depending on age and body needs. For the next 1-1.5 months, the patient has to stay in bed, and then walk on crutches. During the entire period after the removal of the cast immobilization, the child is treated with orthopedic bandages.
1. Antibiotic therapy in the postoperative period from day one – cephalosporins 2-3 generations and lincomycin in an age-appropriate dose for 7-10 days.
2. Antifungals - Mycosyst once or Nystatin in an age appropriate dose, 7-10 days.
Postoperative pain management from day one (Tramadol, Ketonal, Tregan, Promedol) if indicated for 3-5 days.
4) In postoperative anemia – iron preparations (Actiferin, Ranferon, Ferrum lek) to normalize blood parameters.
5) To prevent hypocalcemia (calcium gluconate, Calcium-Dz Nicomed, Calcid, Osteogenon) orally from the 7th to 10th
Transfusion of blood components (SPP, monogroup erythrocytes) intraoperatively and in the postoperative period as needed.
Prophylactic measures: Prevention of bacterial and viral infections.
1. Prevention of contractures and joint stiffness.
Further management: The aim is to restore the functional range of motion in the surrounding joints. 1.5 to 3 months of postoperative joint rehabilitation treatment (exercise therapy, physiotherapy, massage, thermotherapy, BMC).
hospitalization
Indications for hospitalization: Planned pronounced axial deformity of the bones of the upper and lower limbs with impairment of limb function in the form of lameness, restriction of joint function, pain in the surrounding joints.
sources and literature
- Protocols for the diagnosis and treatment of diseases, MH RK (Decree № 239 of 04/07/2010)
- Guidelines for traumatology and orthopedics edited by Novachenko NP 2. Clinical guidelines for physicians based on evidence-based medicine. 2nd edition, GEOTAR, 2002.
information
The elimination of hallux valgus and excellent treatment results
Gentle surgical techniques reliably and painlessly restore easy walking and healthy feet.
For comprehensive information on the treatment and prevention of orthopedic, rheumatological or neurological diseases, please contact us:
 Tel. +7(495)120-46-92
Tel. +7(495)120-46-92
 Email: [email protected]
Email: [email protected]
return form Send us a message on Telegram
Send us a message on Telegram  Contact us on WhatsApp
Contact us on WhatsApp
Our address is 11 Trifonovskaya St., Moscow, Russia.
symptoms
The main complaints are pain in the area of the metatarsophalangeal joint of the big toe, aggravation of pain when loading the feet after walking, presence of a cosmetic defect.
On physical examination: the first toe is turned out, the area of the first toe is painless or moderately painful on palpation, there are signs of transverse flatfoot, bursitis (synovitis).
to form
Depending on the degree of deformation, a distinction is made between moderate, moderate and severe deformation of the first toe.
causes
Wearing uncomfortable, tight shoes is believed to be the most important etiological factor in the development of first toe valgus deviation. In women, the incidence is 10 times higher than in men.
Some authors attribute the development of this pathology to changes in the tendon-ligament apparatus of the foot caused by prolonged static and dynamic loads.
Many authors consider the weakening of the musculoskeletal system of the foot to be the most important pathogenetic cause of the valgus deviation of the first toe. Many authors consider the heritability of the valgus deviation to be the main cause.
Other factors contributing to the development of the disease include: rheumatoid arthritis, amputation of the second toe, neurological disorders, changes in the inclination of the first metatarsal joint, an excessive transverse plane of the head of the first metatarsal, and the presence of additional bones between the bases of the first and second metatarsals.
Based on the presence of several factors, they are divided into:
- External causes: Wearing uncomfortable, tight shoes – 32 %.
- Internal causes: heredity; joint hypermobility; Flatfoot deformity, tarsal coalitions; secondary valgus deviation of the first toe (rheumatoid arthritis, neurogenic disorders); Metatarsus primus varus (32 %)/ foot deformity in which the first metatarsal connected to the proximal phalanx of the thumb bone rotates and deviates from the second metatarsal; Contractures of the calf muscle and Achilles tendon (11 %).
diagnostic procedures
Diagnosis of hallux valgus is made by the orthopedist/traumatologist on the basis of assessment of complaints, anamnesis, clinical examination and the obligatory use of instrumental research methods. Diagnosis aims to determine the etiological factor that caused the condition, as well as to assess the severity of the condition and the resulting complications.
The diagnosis is based on the characteristic clinical picture, the characteristics of the footwear worn, and the radiological findings.
Based on the anamnestic information, changes in the appearance of the foot, difficulty walking, a feeling of fatigue after walking, the presence of a deformity of the first toe and problems with footwear can be noted.
The most important method for diagnosing hallux valgus is an X-ray of the region of the metatarsophalangeal joint. X-rays of the feet are made in two projections. Many works recommend x-rays of the feet in three projections (straight, lateral, axial).
X-rays must be taken under stress as the difference between the angles on the X-rays with and without stress can be as much as 20 %.
There are different degrees of hallux valgus. The degree of valgus is determined by the change in the angle between the first toe and the first metatarsal – hallux valgus angle. An important value for determining the degree of hallux valgus is also the intermetatarsal angle, ie the angle between the first and second metatarsal bones. Depending on the value of this angle, three degrees of valgus are distinguished: moderate, moderate and severe.
With a moderate deformity, the valgus angle of the first toe radiologically does not exceed 20°. The interdigital angle is less than 120°.
The medial deformity is usually accompanied by a subluxation of the first metatarsal joint, unless there is a pathologic angle of the articular surface of the first metatarsal. The valgus angle of the first toe is between 20° and 40°, with the first toe pushing and displacing the second toe. The first interdigital angle is 12° to 16° (less than 180) and the lateral sesamoid is displaced from 75 % to 100 %.
classification
II. DIAGNOSIS AND TREATMENT METHODS, APPROACHES AND PROCEDURES
Minimum list of examinations to be performed upon admission to a proposed hospital:
– Coagulation picture (bleeding and clotting time, prothrombin, fibrinogen, platelet adhesion and aggregation reaction, antithrombin)
- Biochemical blood tests (total protein, alanine aminotransferase, total cholesterol, bilirubin, direct bilirubin, creatinine, urea, glucose, potassium, sodium, phosphorus, calcium, chlorine);
- coagulation diagram (bleeding time and clotting time, prothrombin, fibrinogen, platelet adhesion and aggregation reaction, antithrombin);
- Biochemical blood tests (total protein, alanine aminotransferase, total cholesterol, bilirubin, direct bilirubin, creatinine, urea, glucose, potassium, sodium, phosphorus, calcium, chlorine);
Emergency diagnosis: not performed.
Complaints.Deformation of the limbs, causing functional impairments and cosmetic defects, affecting the patient's psyche.
Medical historyHistory: Trauma to the fingers and/or toes, with increasing deformity of the limb segment with age.
- Hammer toe deformity of the middle fingers accompanied by marked tension under the skin of the extensor tendons and formation of painful knuckles along the dorsum of the deformed fingers;
– Abnormal anatomical bone structure.
differential diagnosis
The diagnosis of acquired finger and toe deformities is not difficult due to the visually detectable deformities and impaired limb function.
• First-generation cephalosporins.Cefazolin, 50-100 mg/kg, intravenously, once 30-60 minutes before surgery.
IV drip doses of 10-20 mg/kg/day, in one or more injections, for severe infections and in children 1 month and older;
Vancomycin: 15 mg/kg/day, to a maximum of 2 g/day, every 8 hours, intravenously; each dose should be administered over at least 60 minutes.
• Paracetamol, 200 mgParacetamol, 200 mg, tablets – at the rate of 60 mg per 1 kg of the child's body weight, 3-4 times a day. The interval between doses should be at least 4 hours. The maximum daily dose is 1.5 g - 2.0 g;
Paracetamol rectal suppositories 125, 250 mg – in a single dose of 10-15 mg/kg of the child's body weight, 2-3 times a day, after 4-6 hours;
Paracetamol suspension 120 mg/5 ml, for oral administration - in a single dose of 10-15 mg/kg body weight, 4 times a day, the interval between consecutive doses is at least 4 hours (the dose for children aged 1 to 3 months is determined individually).
Paracetamol syrup for oral administration 2,4% 50 ml - children from 3 to 12 months - ½-1 teaspoon (60-120 mg); from 1 to 6 years – 1-2 teaspoons (120-240 mg); from 6 to 14 years – 2-3 teaspoons (240-360 mg), 2 to 3 times a day.
The maximum duration of treatment with paracetamol as an analgesic is no more than 3 days.
• Ibuprofen Suspension 100 mg/5ml - 200 ml, for oral administration, 7-10 mg/kg body weight, maximum daily dose - 30 mg/kg. The interval between doses of the drug should not be less than 6 hours. Duration of treatment no longer than 5 days, as an analgesic.
In children aged 1 to 14 years: 1 mg/kg to 2 mg/kg body weight intravenously, intramuscularly or subcutaneously. Intravenous injections should be given very slowly or diluted in an infusion solution and given as an infusion. The dose may be repeated at 4-6 hour intervals.
causes of impairment
Varus deformity of the lower limbs in a child develops as a result of specific causes, most often tibial muscle dysplasia, rickets, intrauterine malnutrition (lack of useful vitamins and micronutrients), intestinal and renal rickets, Blount's disease, which is characterized by an oblique curvature of the lower limbs.
Other factors can be:
- Serious infectious diseases;
- endocrine disorders;
- Various injuries of the feet and shins;
- abnormal calcium intolerance;
- flat feet;
- Inherited predisposition.
In adolescents, varus deformity of the tibia can become active with vitamin D deficiency. In adults with the development of Paget's syndrome, when curvature of the tibia is caused by bone growth and delayed bone loss.
Important!
Classification according to ICD 10: varus deformity of the tibia. Deformities can be unilateral - only one limb is deformed - or bilateral - both limbs are deformed, with visible elements of asymmetry.
False curvatures are created by the visual observation of 'lean legs' when, due to the anatomical positioning of the muscles, the tibia is pulled back giving the appearance of a deformity. This is merely an aesthetic defect that can be corrected with massage, exercise or implants.

clinical picture
As the disease develops, there is deformity of the foot, abnormal redistribution of stress from the inside to the outside of the foot, and impairment of the quality of oscillatory movements in the lower limbs.
The cushioning capacity of the foot is reduced, so that the child often falls, stumbles and walks poorly. The first symptom of varus torsion in children is an unevenly ground sole on the outside of the shoe.
The O-shape of the lower limbs affects the functioning of the knee joints, the femur enlarges, and the ligaments of the knee on the outside are stretched. It can lead to pain when walking, increased stress on the joints, changes in gait and complaints in the spinal area.
The curvature is accompanied by flat feet, which cause swelling, pain when walking, tired legs, and a deterioration in general well-being due to pain.
Non-surgical treatment
Even if a hereditary factor or predisposition to the disease cannot be prevented, it is possible to effectively influence the course of the deformity by 'freezing' its development and eliminating the pain. Wearing comfortable shoes that are not too tight and avoiding high heels is an important factor in preventing big toe valgus deformity.
Conservative methods are justified only in the early stages of the deformity. Depending on the severity of the condition, the following non-surgical treatments for big toe pain may be recommended:
- Adjustment of footwear to eliminate friction in the medial eminence area. For example, some patients should wear shoes with a wider and deeper insole. In some cases, special insoles are also acceptable.
- Flat feet can be improved with the use of an orthopedic device - an orthosis.
- Achilles tendon contracture may require stretching or even lengthening.
- Physiotherapeutic treatments and massages.
Foot surgery for valgus deformity

If conservative treatment is ineffective, surgery should be considered. Before deciding on one or the other operation, the exact degree of valgus deformity of the big toe is determined. X-rays are taken for this purpose.
Surgical treatment is warranted for grade 3-4 deformities when there is significant deviation between the first and second metatarsal bones. There are several effective surgical techniques for halus valgus including open surgery where the bone is realigned, surgical implants, orthopedic screws, etc.
Experienced surgeons often use a combined surgical approach, depending on the severity of the disease and the patient's medical history, to achieve the best possible treatment outcome.
The orthopedic surgeons of the German Family Clinic also attach great importance to the postoperative management of the patient. With all surgical interventions, the patient can move in postoperative shoes immediately after the procedure. Postoperative shoes and compression bandages must be worn for six to eight weeks. After this time, the focus should be on restoring normal range of motion in the toe and ankle joints and muscle recovery. The doctor will make recommendations for back correction, in particular, exercises to restore normal posture.
- chalgus valgus.
- Stages of hallux valgus.
- flatfoot μb.
- Deflection of the first toe.
- First metatarsophalangeal joint of the foot (metatarsophalangeal joint).
- flatfoot.
- Shoes for hallux valgus.
- Valgus flatfoot (valgus flatfoot).
