It's one thing if your child rarely walks on tiptoes - during exercises or when he's just running around. But if this gait is the norm and it carries out most of its activities this way, that's a wake-up call.

- Diagnosis of scoliosis
- The main signs that indicate possible problems with your child's legs are
- The Chaplin Walk
- Symptoms of clubfoot in children
- Causes of clubfoot in children
- Symptoms of Clubfoot
- Treatment of clubfoot
- The most popular
- Latest updates
- My subscriptions:
- What are Taylor's deformities?
- signs
- How they are created
- treatment methods
- Shoes
- massage
- Medication
- What are clubfoot, valgus and varus deformities and how are they treated?
- Then what is a Varus?
- Treatment tactics for children
- What parents can do to help
Contact
Exercises for scoliosis at home
Postural abnormalities are most common in elementary and middle school-aged children. But they also occur in adults. This musculoskeletal disorder can occur in children from birth or as a result of improper sitting and walking. The most correct and cost-effective method of treating this condition is a series of exercises and treatments: LFC (physical therapy), massage, paraffin therapy, swimming and stretching.
Diagnosis of scoliosis
Diagnosing scoliosis alone is not easy. In order to make a correct diagnosis and initiate treatment, a series of procedures must be performed. For the trauma surgeon, Specialization in forms of scoliosis, It is not enough to simply examine the patient, even with the help of computer technology.
Diagnosis of scoliosis requires:
- an orthopedic examination;
- an evaluation by a neurologist to rule out neurological diseases;
- a study of metabolism;
- a record of congenital deformities.
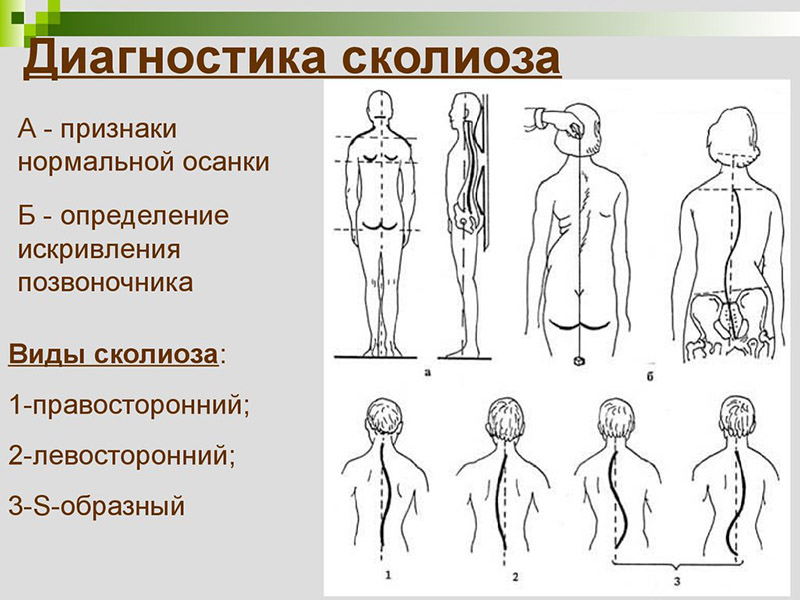
The main method for diagnosing this deformity is. X-RAY. It is one of the most accurate methods in the world. It enables changes in the spine to be monitored. It is one of the cheapest but most harmful methods of examining the spine.
The second method after the X-rays is. the photography. It helps in assessing postural changes. It's not the most accurate, but it's safe.
Optical tomography (computed tomography) Suitable for teenagers only. Scoliometer (scoliometer) Similar properties to computed tomography. MRI (magnetic resonance imaging) and CT scans do not give a complete, high-quality picture of the disease, so an X-ray is most appropriate.
The main signs that indicate possible problems with your child's legs are
- Tires too quickly, the child cannot walk for a long time.
- It may not jump, or the jumps are strange and unusual.
- It can be done with your legs hanging back or with your feet wide apart.
- Instead of a normal step, the child runs, is carried in different directions, legs wander, feet scrape on the ground, knees bump against each other.
- All shoes are worn out.
- The child complains of foot pain at night.
These are common symptoms that may indicate a musculoskeletal problem. Of course, the child may intentionally keep their feet crooked and refuse to jump because it hurts themselves.
The parent's job is to watch the child. If this happens frequently, especially when it feels unobserved, it is worth seeking professional advice. The most important thing is not to panic or scold your child: this can only make the situation worse.
It is worth paying attention to the symptoms of certain gaits, which, if noticed, can prevent the problem or correct it in a shorter time.
The Chaplin Walk
The Chaplin gait is characterized by a strong spread of the legs and walking on almost straight legs. This gait causes twisting of the hip joints due to muscle tension. While Chaplin films evoke positive emotions and nostalgia, parents who see their child leaving in this way ask themselves the question: 'Is everything OK? While this can be seen with the naked eye in older children, the conditions are not always obvious in younger children.
- If your baby isn't walking yet, you should pay attention to how he stands in the crib (important with loft beds). If his feet are always pointing to the side, chances are good that his feet are facing outwards.
- When your baby is just starting to walk, pay attention to how his knees are turned - they shouldn't be pointing outwards.
TIP: When your baby is learning to walk – Do not put a diaper or toys around the waist. Don't let anything get in the way of your baby taking his first steps.
For most healthy babies, this problem will resolve itself: over time, the pelvis will separate completely. However, if the child has already separated and the problem persists, exercise may help. If the problem is ignored, the child is at risk of developing clubfoot.
Symptoms of clubfoot in children
As a rule, the pathology appears at birth: the soles of the feet are directed inwards and upwards, and movement in the ankle joint is restricted. When the child is already walking, he or she leans only on the outer edge of the foot. The child steps on the foot on which he is resting. The gait is wobbly and uneven.
Without treatment, the bony misalignment worsens and subluxations occur in the small ankle joints. The outer edge of the foot skin thickens. The muscles of the lower leg that are not involved in walking gradually weaken and atrophy. This is followed by dysfunction of the knee and pelvic joints. The later treatment begins, the more serious and difficult it is to correct.
The main symptoms of clubfoot in children include:
- – The flexion of the sole of the foot is pronounced in the ankle joint;
- – the sole is turned inwards with the outer edge hanging downwards;
- – the forefoot is turned inwards;
- – the muscles of the lower limbs are underdeveloped and atrophy in older children;
- – A wobbly gait is noticeable;
- – In unilateral cases, one leg is several centimeters shorter than the other.
The children tire quickly when walking and standing, rub their skin and complain of pulling pain in their legs.
Causes of clubfoot in children
There are several defects that can cause a child to develop clubfoot. The most common include:
- – Exposure of the mother's body to unfavorable factors during the first trimester, when the lower limbs lie down;
- – mother’s unhealthy habits – smoking, alcohol and drug abuse;
- – Pressure (mechanical) from the umbilical cord or amniotic sac on the foot;
- – Low amniotic fluid level when the uterus presses on the feet of the fetus;
- – Congenital pathologies of the spinal cord or peripheral nerves;
- – Uncontrolled intake of high-dose medication;
- – Certain infections;
- – Cancers of the uterus.
The fetus is most at risk during the first trimester. Damage caused during this time is very difficult to repair later. The situation is particularly serious when genetic problems are combined with external factors of aggression.
Symptoms of Clubfoot
Congenital clubfoot can be diagnosed by ultrasound as early as the 16th week of pregnancy. But even after the birth of the child, the following symptoms can be suspected:
- The toes are curved inwards.
- The toe is pointing down and the heel is higher than the toe.
- The hock is twisted outwards.
- The tibia and joint are stiff.
The following symptoms are easy to spot in older children:
- Kicking your shoes hard.
- Abnormal gait (the foot appears to have stepped inward).
- Calluses, corns, calluses under the big toe.
- Complaints of discomfort in the foot.
Treatment of clubfoot
The cause of clubfoot can only be determined in one out of five cases. In most cases, it is a congenital disorder caused by heredity or maternal mistakes during pregnancy.
Clubfoot can also occur in a healthy child in the first 2 years of life. The causes of the deformity can be different: trauma, polio, rickets, muscle hypertension, increased load on the musculoskeletal system, poorly fitting footwear and others.
Treatment for clubfoot depends on the exact diagnosis and the type of deformity. It is extremely important to determine the severity of the disease and try to determine the cause. Come to the KIT Multispecialty Clinic for a consultation for an examination and treatment of clubfoot. Our specialists will find the best treatment option for you.
A foot deformity can be corrected in many different ways. Depending on the severity and individual physiological characteristics of the patient, the following methods may be effective:
- tight bandaging,
- plaster casts,
- therapeutic massage,
- PHYSIOTHERAPY,
- Physiotherapy,
- paraffin compresses,
- selection of orthopedic footwear,
- surgical treatment,
- Ponseti method (3-stage treatment for children up to 2 years).
The specialists of our clinic will develop an individual treatment plan that can combine several of the above methods. This increases effectiveness and speeds up your child's recovery.
The most popular
'Neither I nor Sting nor McCartney know the secret of a hit.' – Igor Sarukhanov on how a hit is made. Unformatted. Excerpt from the broadcast from March 17, 2023.
'I want to know who a rat is! Polina Gagarina raged on the set of the program 'Voice 11'. Excerpt from the broadcast from March 17, 2023.
'I treat my age with great respect'. – Irina Ponarovskaya talks about compliments and the age limit. Tonight's show. Abstract .
Every child in Georgia should play the piano'. Brandon Stone talks about how his love of music is in his blood. Anecdotes. Excerpt from March 10, 2023.
'You have become unhappy!' A divorced man reveals how his daughter sees him. Psyche. Excerpt from March 12, 2023.
Latest updates
Are ultraviolet light bulbs dangerous; milk oolong green tea; arthritis in the lower back; Lose excess – start a project. Live healthy!
- about the company
- First funding
- Special Projects
- OTT version of Channel One
- online cinema
- HbbTV Interactive television
- Channel One applications
- Casting for Channel One
- Tell your story about a World War II veteran
- All Movies
- Switch to digital broadcasting
- Your ideas for Channel One
- Working at Channel One
- TV ratings
- User Agreement
- Contact
- Feel free to contact us
My subscriptions:
© 1996-2023, Channel One. All rights reserved.
Reproduction of the material in whole or in part is prohibited.
Permission to use material from the site requires a link to the resource.
The code to embed videos in blogs and other resources on our site may be used without permission.
Online transmission without authorization is strictly prohibited.
Broadcast contribution.
What are Taylor's deformities?
The habit of sitting cross-legged for long periods of time puts constant strain on the outer edges of the feet. The nutrition of these areas is compromised and micro-injuries to the bones and cartilage occur. The last metatarsal bone deforms (its axis deviates towards the outside of the foot), which leads to a flexion of the little toe towards the ring toe and the typical clubfoot arch.
The foot begins to widen, which can make it difficult not only to exercise, but even to walk slowly.
Other causes of Taylor deformity include:
- Peculiarities in the structure of the foot, which either arose at birth or were inherited and are prone to certain anomalies;
- Changes in the structure of the fifth toe, the foot itself (flatfoot, clubfoot);
- Prolonged wearing of unsuitable, tight, uncomfortable shoes with high heels or platforms;
- Trauma, fractures, irregular adhesions of the bones of the little toe;
- tumor masses;
- Certain neurological diseases.
The unphysiological structure of the little toe can be congenital or acquired. Often the condition is combined with a deformity of the big toe, causing the foot to become even wider. This is caused by a weakening of the interdigital ligaments in the foot.
If left untreated, this leads to an unsteady foot hold, the little toe loses mobility and the constant pain makes life difficult, which can lead to purulent inflammation and nerve damage.
signs
The symptoms of the disease include.
- Pain (which increases with exercise but can also occur at rest), feeling unwell;
- Enlargement of the transverse arch of the foot;
- Swelling;
- Redness of the skin in the painful area, between the toes;
- wounds and lesions on the bony prominences;
- Calluses on the surface of the foot.
Free consultation with the head of the Center for Orthopedics and Traumatology, trauma orthopedist of the highest category, medical student Samoilov VV in joint surgery.
How to restore lightness of gait? Relief from joint pain at ON CLINIC
How they are created
Under the influence of one or more of the above causes, changes occur in the bones of the foot. The bones of the foot begin to change shape and assume an unphysiological position. Ligaments and muscles gradually adapt to the changing shape of the foot. This is how a club foot develops.
The symptoms of clubfoot in adults differ slightly from those in children. The most characteristic symptom of clubfoot is the inability to place the entire sole on the ground. The foot is turned to the right or left and part of the heel is raised. Most of the time the foot is turned inwards and the person supports themselves on the outside of the foot.
An adult with a clubfoot has a characteristic 'pooh-pooh' shape. Due to the misalignment of the foot, the lumbar spine is flattened and the thoracic spine is arched. As a result, the back is rounded and the buttocks are raised. A typical clubfoot gait develops.
There are 4 stages of clubfoot development:
- Mild. The pathological changes are minimal and are corrected by wearing orthopedic shoes, massage and gymnastics,
- Medium. The changes are more pronounced, a pain syndrome develops and the alignment of the ankle changes. The treatment is more complex and lengthy,
- Severe. The curvature of the foot and ankle is very pronounced. Correction is only possible through surgery,
- Extremely heavy. Heaviness. Severe deformation of the limbs. The associated curvature of the spine, changes in the position of the internal organs. This stage cannot be treated.
During the examination, the following signs of pathology can be identified:
- forefoot elevation,
- Unequal alignment of the outer and inner edges of the foot,
- Restriction of movement in the ankle joint,
- high arch of the foot,
- Inward curvature of the toes.
Read more:Interesting!!!
If a person develops a severe or very severe degree of clubfoot, he becomes disabled.
treatment methods
How to stop clubfoot - an adult cannot cope with this condition alone. Clubfoot treatment must be prescribed by a podiatrist. A combination of various conservative methods is used and, if these are ineffective, surgical methods.
Shoes
When doctors explain how to get rid of clubfoot in adults, they point out the importance of wearing orthopedic shoes. The foot is in a physiological position and does not drift any further. High heels are strictly prohibited for clubfoot in adults. The maximum heel height should not exceed two centimeters.
The right therapeutic footwear for clubfoot has supinators on the inside of the sole, a stiff buttocks and a thick toe. This ensures maximum fixation of the foot. People with clubfoot must always wear orthopedic shoes.
massage
Massage is not a one-size-fits-all solution. However, it is a mandatory step in the treatment of clubfoot. It strengthens the muscles and ligaments, relieves pain and eliminates cramps. The massage is performed daily before going to bed. Various oils or pain-relieving gels can be used for the massage.
Medication
Taking medication is recommended if the cause of clubfoot is a pathology of the nervous system. Prozerin is used to restore neuromuscular transmission. It is administered in the form of intramuscular injections. Drug appointed under strict indications, as it has significant side effects.
Important!!!
Proserin should only be prescribed by a doctor and treated under medical supervision. This medication is easy to overdose on, which can lead to serious heart rhythm problems.
Symptomatic medical treatment of clubfoot consists in taking painkillers, drugs to improve blood circulation, vitamin and mineral complexes and cartilage protectants.
What are clubfoot, valgus and varus deformities and how are they treated?
Clubfoot is a congenital orthopedic pathology in which the foot is turned inwards. This defect must be treated from birth, and not just with orthopedic shoes. The treatment of this pathology involves plastering, supports and often surgery.
Source: Orthofoot Footwear, with permission from the author and with copyright.
It is not uncommon to hear from parents of young children: 'My child has a clubfoot' and the orthopedist makes the diagnosis: varus of the feet.
Are clubfoot and varus position one and the same disease?
True clubfoot is a congenital orthopedic pathology in which the foot is turned inward. This defect must be treated from birth, and under no circumstances with orthopedic shoes. Treatment of this pathology involves casting, bracing and often surgery.
Normal foot (left) and congenital clubfoot (right)
There are many causes of congenital clubfoot in children.
The most common factors contributing to the development of foot pathology include vitamin deficiency during pregnancy, hereditary predisposition, abnormal development of the foot due to the unfavorable position of the baby in the womb, etc.
Clubfoot is a deformity of the child's foot. It is a malformation of the ankle joint characterized by equinus (restricted upward movement of the foot), varus (walking on the outside of the foot) and supination (abnormal inward rotation of the foot), as well as hypoplasia or atrophy of the lower extremity.
Then what is a Varus?
Varus is a foot position in which the forefoot (toe) is turned inward and the foot rests on the outer edge of the foot when walking.
Normal foot (left), valgus deformity (middle), varus deformity (right)
Varus in a child is easy to recognize: you can see it when walking and when the child uses their toes. The outer edge of the foot is lowered and the inner edge is raised.
The orthopedist treats the varus or foot deformity and prescribes a specific rehabilitation measure that must be carried out. In any case, correcting a foot deformity requires patience as the process can take several years.
The doctor will make a series of recommendations: daily exercises, massages (a general course every three months and a selective course in which specific parts of the child's feet are massaged: foot, shin, etc.).
Massage and special exercises for the feet
It is also often recommended to go to the swimming pool (1-2 times a week) and to wear special orthopedic varus shoes, which are equipped with a special instep that extends the foot outwards and a high pad that fixes the ankle. This allows the child to place the foot vertically, as the varus shoe causes discomfort when the foot is turned inward.
In addition, these shoes often require special insoles (including orthopedic ones).
The most important thing is that you follow all the orthopedist's recommendations, then your child will be healthy!
Treatment tactics for children
Treatment of arthrosis and osteoarthritis in children is comprehensive: it includes medication and physiotherapy. With the help of analgesics in a dose specifically selected for the age, the pain spasm can be stopped. Sometimes anti-inflammatory ointments and lotions can also be used, but only if prescribed by a doctor.
In some cases, intra-articular injections of synovial fluid replacement, such as: B. the safe synthetic drug Noltrex, may be helpful in treating the disease. This method is usually used when the disease has already progressed to the second or third stage and has become severe.
In the initial phase, physiotherapeutic measures such as massages, electrophoresis and UHF as well as special exercise therapy help to get the symptoms under control. During the remission phase, it is not inappropriate for the young patient to take a course of treatment. In general, treatment depends on the child's health, physical abilities and lifestyle.
A child with osteoarthritis should be examined by a podiatrist at least once a year.
What parents can do to help
Osteoarthritis and its forms are diseases that a child has to live with for many years. It is therefore the responsibility of parents to provide their son or daughter with knowledge about nutrition and daily activities and to instill healthy habits.
- In order to prevent excess weight, which is dangerous for the joints, the diet should be improved by enriching it with fruit and vegetables as well as dairy products and avoiding flour and chocolate.
- Your doctor may prescribe vitamins containing calcium.
- The specialist will prescribe special exercises for the joints, which should be done regularly to avoid relapses.
- It is the parents' responsibility to provide their son or daughter with a suitable workplace (chair with a straight back) and a bed with a firm base or an orthopedic mattress (depending on the form of the illness).
- Footwear is also important: it should be made of high-quality materials.
The most important thing for caring parents is to find a competent doctor who will not only prescribe treatment, but also discover the cause of arthrosis at such a young age. This is the only way to keep the disease under control and stop its progression. For example, if the cause of the problem is an endocrine malfunction, the hormones must first be brought into balance, and if the knees suffer from excess weight, you will have to prescribe a strict diet for your child.
Either way, if your child complains of knee, elbow, or other joint pain, you should not self-medicate. The sooner you make an appointment with a good orthopedist, the greater the chance that your child will be able to lead a fulfilling and active life!
- Why does a child develop clubfoot?.
- What is clubfoot?.
- Congenital clubfoot.
- clubfoot.
- Footwear for children's clubfoot.
- 1 year old child with clubfoot.
- Clubfoot in 7-year-old children.
- Clubfoot Treatment.
