5.5 Access to the Material is sequential by topic. At any point in time, the customer is provided with a topic for study. Once material on a topic is completed, access to that topic will be terminated.

- Leg shortening, how do you distinguish functional from anatomical shortening?
- Fitness training for trainers.
- Our courses are suitable for both beginners and experienced trainers and offer income growth and career development.
- What is the risk of shortening the quadriceps muscle?
- Stretching of the quadriceps femoris muscle
- Shorten
- diagnosis
- differential diagnosis
- Shortening defects of the lower limbs
- Automation of your clinic: fast and inexpensive!
- Automation of your clinic: fast and inexpensive!
- classification
- One leg is shorter. How does the orthopedist treat this? Are shoe inserts required?
- causes and symptoms
- diagnosis
- Where does short leg syndrome come from and when will it be fixed?
- Diagnostic methods for the 'short leg syndrome
- Caused
- diagnosis
Leg shortening, how do you distinguish functional from anatomical shortening?
How can you distinguish a functional from an anatomical leg shortening?
The only sure way is an X-ray examination (topogram of the lower limbs, panoramic tomography of the legs).
Functional shortening is accompanied by:
- twisting of the pelvis,
- valgus femur and asymmetric valgus knee;
- asymmetrical positioning of the foot in valgus/varus position.
- In a standing position – different heights of the greater trochanter and the ischial tuberosity,
- in supine position – tibial tuberosity, heels, inner malleolus in supine and prone position.
It is important to be aware that all of these signs are circumstantial, that numerous compensations 'blur' the picture and that even with a perfect examination, the measurement error can exceed the desired leg length discrepancy.
Therefore, if significant leg shortening is suspected, it is advisable to refer the person for an X-ray examination.
Fitness training for trainers.
For fitness instructors looking for classes that will increase their income, make them even cooler, and never have to worry about finding a job again, we recommend the following distance learning courses:
Basic personal trainer course – For trainers who want to supplement their knowledge with basic information. An incredible amount of useful material that will take you to the next level.
upgrade – Online course for fitness trainers who want to increase their income and knowledge. Custom Themes.
structure of the body – Course by author Dmitry Gorkovsky with practice days on site and remote theory for fitness trainers, massage therapists and doctors.
pregnancy – Training techniques for pregnancy courses and postpartum recovery.
Our courses are suitable for
for both beginners and experienced trainers and offer income increase and career development.


The user who purchases services from the evotren.ru website, hereinafter referred to as 'Client', on the one hand and Evotren LLC, hereinafter referred to as 'Contractor', represented by CEO FG Kapishev, acting under the Charter, on on the other hand, automatically entered into this Agreement (hereinafter – 'Agreement') when purchasing services from the Contractor on the following:
1. TERMS AND DEFINITIONS USED IN THE CONTRACT
1.1. customer – a natural person, a sole proprietorship or a legal entity, regardless of its legal form, who has placed an order with the Contractor under the terms of this Agreement by purchasing the Services of the Contractor.
1.2. contractor – is the legal entity providing services to the Client under the Agreement.
1.3. Services – Services consisting in providing access to the study of the distance learning material indicated in the description of the information courses.
1.4. site – The contractor's information resource, located on the Internet at: edu.evotren.com
1.5. The contractor's personal account – The program interface on the website for studying the informational material and other necessary information, accessible to the customer after authorization by a login and password.
1.6. Order – An automatically generated document detailing the services requested by the customer. The order is placed by filling out the necessary forms on the contractor's website -www.evotren.ru.
1.7. Acceptance of the terms of the contract – The acceptance of the contractual conditions by the customer takes place by paying for the services in cash or by means of cashless or electronic means of payment. Acceptance of the contractual conditions is deemed to have taken place at the time the customer pays for the services in cash or by means of cashless or electronic means of payment.
What is the risk of shortening the quadriceps muscle?
The quadriceps muscle is the front muscle of the thigh, the extensor of the knee. A spastic and shortened quadriceps pulls the pelvic bones forward and downward, resulting in abnormally increased lumbar lordosis and a hyperextended lower back. Hyperlordosis - increased lumbar flexion - causes the abdomen to expand forward and the pelvis to expand back and down.
Many people believe that the number one solution to a bulging stomach is to exercise your abdominal muscles. It's true that strong abs, especially deep abs, are important for back health because they support the spine from the front, relieve stress on the lower back, and create a natural corset for the body. A bloated stomach makes it easier to keep the stomach tight, but they cannot completely solve the problem. If the quadriceps of the thigh are shortened and the lower back is weak, then over time the hyperlordosis will only get worse, that is, the progression of the lowering will continue.
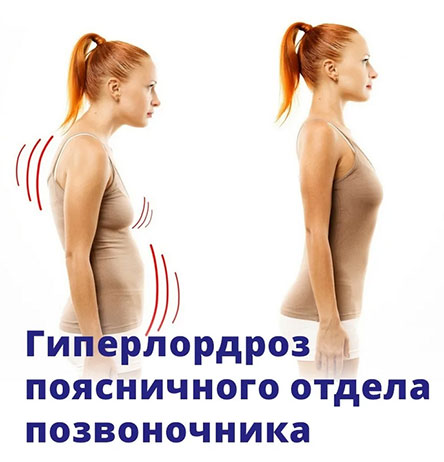
Visually, increased lumbar flexion doesn't look very aesthetic, but that's not the only problem.
Hyperlordosis leads to deformation and displacement of the vertebrae in the lower back and narrows the lumen of the intervertebral foramen, where the peripheral nerve roots are located. Eventually, this leads to degenerative changes in the spine, bulging, and eventually herniated discs. This also affects the joints of the legs, which are additionally stressed when walking due to the reduced cushioning properties of the spine.
The only way to treat hyperlordosis is to pay attention to the condition of the muscles. The priority should be to restore the quadriceps and lumbosacral muscles of the back to proper condition and function.
Stretching of the quadriceps femoris muscle
Exercise 1Stretch the quadriceps while standing on one leg.
A classic exercise that you can do anywhere you want. Even during the lunch break at work. Stand up straight, bend your leg at the knee, and grab your shin with your hand. Keep your knees together. If you find it difficult to keep your balance, use your hand to support yourself on the chair in front of you or on the wall. Pull the heel as close to your buttocks as possible. After 30-50 seconds, repeat the exercise with the other leg.
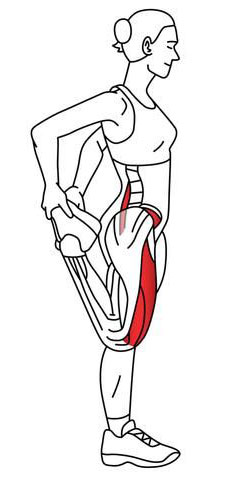
The exercise is great for stretching the front of the thigh, improving mobility and eliminating muscle stiffness. It has a decompressing effect on the knee joint.
Exercise #2Stretching the quadriceps muscle in a lunge.
Stand up straight, bend backwards and place your knee on the floor. If you find it difficult to balance, you can lean on a chair with your free hand. Grab your foot with your left hand and try to pull it towards your buttocks. After 20-30 seconds, repeat the exercise with the other foot.
Shorten
Shortening of a limb means shortening of the length of a limb. There are several reasons for shortening:
- to compensate for different limb lengths
- for binding after removal of tumors
- used to shorten after resection of a limb that has been broken due to trauma or a regrowing disease (osteomyelitis).
- in growth disorders (both limbs are shortened).
Shortening operations should not be considered mutilation. Technically, it's a more complicated process than renewing. It requires compliance with certain rules. First of all, the shortening should not be more than 4-5 cm, as this can lead to muscle and tendon disorders. After the resection, the bone fragments should not be brought together all at once, but gradually, in order to avoid compression of vessels and nerves.
The choice of foreshortening technique is decided on a case-by-case basis.
diagnosis
II. DIAGNOSIS AND TREATMENT METHODS, APPROACHES AND PROCEDURES
Minimum list of tests to be performed upon admission to an elective hospital:
- coagulation picture (bleeding duration and clotting time, prothrombin, fibrinogen, platelet adhesion and aggregation reaction, antithrombin);
- blood chemistry (total protein, alanine aminotransferase, total cholesterol, bilirubin, direct bilirubin, creatinine, urea, glucose, potassium, sodium, phosphorus, calcium, chlorine);
- coagulation values (bleeding and clotting time, prothrombin, fibrinogen, platelet adhesion and aggregation reaction, antithrombin);
- blood chemistry (total protein, alanine aminotransferase, total cholesterol, bilirubin, direct bilirubin, creatinine, urea, glucose, potassium, sodium, phosphorus, calcium, chlorine);
complaintsDeformation and shortening of the upper limbs, which leads to functional impairments and cosmetic defects, burdening the patient's psyche.
Medical history: The disease manifests itself from birth, with increasing deformity and shortening of the limb segment with age.
– Underdevelopment of the bones of the forearm (especially the radial bone); abnormal development of the fingers and hand.
– Other changes in the hand are hypoplasia and clinodactyly of the 2nd finger, syndactyly, flexion and extension contractures of the middle and interphalangeal joints, especially the 2nd and 3rd fingers. The carpal bones on the radial side are also affected, with aplasia or calculus with other bones being observed.
– X-ray of the upper limbs with the adjacent joints (picture of the shortening and deformation of the forearm bones).
– CT scan: Depending on the degree of anomaly of the limb and the nature of the defect, hypoplasia/aplasia of the bony structures of the upper limb and their deformation are detected.
– Consultation of an oncologist (if there are bone masses to rule out a malignant disease);
differential diagnosis
Diagnosis of congenital clubfoot is not difficult due to the visually detectable deformities and obvious limb dysfunction.
• First-generation cephalosporinsSingle dose: Cefazolin, 50-100 mg/kg, intravenously, once 30-60 minutes before the procedure.
Intravenous drip of 10-20 mg/kg/day in one or more injections for severe infections and in children 1 month of age and older;
Vancomycin: 15 mg/kg/day, maximum 2 g/day, in 4 intravenous doses, each dose administered over at least 60 minutes.
• paracetamolParacetamol, 200 mg, tablets – at a dosage of 60 mg per kg of the child's body weight, 3-4 times a day. The interval between doses should be at least 4 hours. The maximum daily dose is 1.5 g - 2.0 g;
Paracetamol rectal suppositories 125, 250 mg – single dose 10 – 15 mg/kg body weight of the child, 2-3 times a day, after 4-6 hours;
Paracetamol suspension 120 mg/5 ml, for oral administration - a single dose of the drug is 10-15 mg/kg of the child's body weight, 4 times a day, with an interval of at least 4 hours between successive doses (the dose for children at the age of 1 to 3 months is determined individually).
Paracetamol syrup for oral administration 2,4% 50 ml - children from 3 to 12 months - ½-1 teaspoon (60-120 mg); from 1 to 6 years – 1-2 teaspoons (120-240 mg); from 6 to 14 years – 2-3 teaspoons (240-360 mg), 2-3 times a day.
The maximum duration of treatment with paracetamol as a pain reliever is 3 days.
• Ibuprofen Suspension 100 mg/5ml - 200 ml, for oral administration, 7-10 mg/kg body weight, maximum daily dose 30 mg/kg. The interval between doses of the drug should not be less than 6 hours. The duration of treatment should not exceed 5 days as an analgesic.
In children aged 1 to 14 years: 1 mg/kg to 2 mg/kg body weight intravenously, intramuscularly or subcutaneously. Intravenous injections should be given very slowly or diluted in an infusion solution and given as an infusion. The dose may be repeated at 4-6 hour intervals.
Shortening defects of the lower limbs
Shortening errors of the lower limbs (ectromelia) – is a congenital anomaly of limb development associated with severe underdevelopment or absence of limbs [1].
User of the log: Orthopedic pediatric traumatologists, general practitioners, pediatric surgeons, medical physiotherapists (physiotherapists, physiotherapists).

Automation of your clinic: fast and inexpensive!
– 800 RUB / 5,500 KZT / 27 BYN – 1 order per month

Automation of your clinic: fast and inexpensive!
classification
Clinical classification of lower limb shortening defects (ectromelia) [1].
Types of lower limb shortening defects (ectromelia):
• Distal ectromelia (distal ectromelia) – is an anomaly affecting the distal part of the limbs.
There are the following types of distal ectromelia:
– Type of the first toe. – Hypoplasia or aplasia of the thumb or the presence of a three-toed thumb
– tibia type – Hypoplasia or aplasia (partial or total) of the tibia. It is associated with shortening and curvature of the tibia, malformation of the fibula, foot, underdevelopment of the quadriceps femoris, and anomalies of the patella. Abnormalities of the lower leg and foot muscles are also observed. Frequently, the deformity is accompanied by an aplasia of the I-II metatarsals and the corresponding toes, sometimes also by a fibular duplication. It is more common on one side, more rarely on both sides.
• Axial ectromelia – Absence or hypoplasia of both the distal and proximal parts of the limbs.
Depending on the extent of the process, a distinction is made:
– long axial type Leg – hypoplasia or partial aplasia of the thigh with partial aplasia of the tibia or complete aplasia of the tibia;
– intermediate type Leg - subtotal femoral aplasia with partial or total tibial aplasia;
– Short axial type Leg – total femoral aplasia with partial or total tibial aplasia.
• Proximal ectromelia – A defect of the proximal part of the leg (thigh bone) without damaging the distal part. It manifests itself in a shortening and curvature of the femur, whereby the kneecap and fibula may be missing.
The following types are distinguished:
– Long proximal type - Hypoplasia of the thigh or partial aplasia of the thigh;
– Intermediate proximal type – Subtotal femoral aplasia;
– Short proximal type – Total hip aplasia.
One leg is shorter. How does the orthopedist treat this? Are shoe inserts required?
As a rule, the orthopedist recommends an insole for the short leg. To balance the hold. How justified is this treatment? There are several options to consider.
(a) If the parents do not intend to have their child treated by a chiropractor and are genuinely trying to straighten their child's legs, a brace can probably be arranged in that case. For what reason? To more or less maintain the posture. However, the orthoses have to be worn for life and replaced from time to time;
(b) If the parents want to try to straighten their child's feet and alleviate the problems described above, then not using orthotics makes sense.
2. One leg is shorter in an adult or older child. If the child is older than 10-12 years and does not have a chance to straighten his legs (he has already tried and it does not work) - in this case it may make sense to use orthotics to maintain posture. If it's an adult who has lived their whole life with different feet and without an orthosis, in my humble opinion it's not worth equipping them with an orthosis. Since a whole chain of adjustments has formed in the body over the years, the body as a whole has long since found its balance. If you put an insole under the foot of such a person, you disrupt all these adaptations and force the organism to seek a new balance. This can be accompanied by a number of unpleasant side effects (discomfort, joint pain, lower back pain, etc.). Especially in middle age and old age.
How many sessions are necessary and what are the chances?
In the case of anatomical shortening, the first sessions are carried out at short intervals (about a week), the subsequent sessions then every 1-2 months or less frequently if the dynamics are good. The total duration of treatment is at least one year.
The number and frequency of treatment sessions is determined individually. It all depends on the severity of the problem, age and the ability of each body to respond to treatment: for some the process is fast and dynamic, for others it is slow and lengthy. As already mentioned, the chances of success also depend on the age of the child, the severity of the lesion and careful adherence to the recommendations and visit schedule.
In the case of functional shortening, this is much easier and faster. In my practice it usually takes 2-3 sessions to treat a short leg.
causes and symptoms
Bilateral leg shortening is caused by a variety of genetic conditions. The unilateral form can be provoked by various pathologies and diseases:
The slight difference in leg length is often not even visible to the patient and is only determined during special examinations. If the difference in length of the limbs is more than 3 centimeters, there is a significant pelvic tilt, which impedes normal walking and causes a limp.
In children, shortening of the lower limbs is usually detected during an examination by an orthopedist. Several external signs (position of the back of the knee, upper pole of the knee, etc.) indicate the presence of an anomaly.
diagnosis
To clarify the severity and nature of the pathology, the doctor measures the length of the patient's lower limbs, as well as each segment, focusing on the bony protrusions (ankles, knees, etc.). X-rays are also recommended.
Lower limb shortening is treated by specialists such as podiatrists and traumatologists. In the case of a slight shortening, conservative correction (wearing special shoes and orthoses) is indicated.
If the pathology is caused by a hip dislocation or subluxation, treatment consists of splinting, exercise and massage. In some cases, the dislocation is corrected with surgery.
A major dislocation requires surgery. The most common method of orthopedic foot correction is the use of an Ilizarov brace.
Legs of unequal length are a serious disorder and, if not treated properly, can cause serious joint and spine problems.
- Open daily from 09:00 to 22:00
- All diagnosis rooms are open daily from 08:00 to 22:00
- Trauma and treatment rooms open 24 hours a day
- Open daily from 09:00 to 22:00
- All diagnostic practices open daily from 08:00 to 22:00
- Trauma and treatment rooms open 24 hours a day
- Open daily from 09:00 to 22:00
- All diagnostic practices open daily from 08:00 to 22:00
- Trauma and treatment rooms open 24 hours a day
- Open from 08:00 to 22:00 daily
- All diagnosis rooms are open daily from 08:00 to 22:00
- Trauma and treatment rooms open daily from 08:00 to 22:00
- Open from 09:00 to 22:00 daily
- All diagnosis rooms are open daily from 08:00 to 22:00
- Trauma and treatment practices are open 24 hours a day
Where does short leg syndrome come from and when will it be fixed?
Short leg syndrome has been actively researched for many years. In 1981, DB Clement et al. in their study of this phenomenon that differences in the length of the lower limbs in 59 % runners can cause back pain.

SI Subotnik studied 4,000 athletes around the same time and found a leg length discrepancy in 40 % of them. According to O. Freiberg and other researchers, the number of people with a leg length discrepancy of 5 mm or more is more than 50 % worldwide.
Sports physician and orthopedist Vladimir Nechaev emphasizes that a leg length difference of up to 5 mm is a clear indication for non-surgical correction. If we are talking about athletes who are constantly subjected to intense loads, then the correction should already be made with a leg length difference of 3 mm.
But what if she is bigger? An asymmetry of about 9 mm leads to lumbago, a difference of 10 mm means an increased risk of intervertebral fractures and a difference of 15 mm can lead to scoliosis. With a leg length difference of 20 mm or more, a person's physical resources and general mobility are severely restricted.
- Anatomically related. Can result from congenital malformations, birth and trauma, arthrosis, operations (e.g. endoprosthetics) or cancer.
- Functional. In this case, the asymmetry is not accompanied by shortening of the bones of the limb and can be caused by weakness or shortening of muscles and ligaments, joint contractures and changes in the biomechanics of the foot.
20 interesting facts about the human body in our gallery:
Diagnostic methods for the 'short leg syndrome
The examination and treatment of suspected short leg syndrome is carried out by podiatrists and orthopedists.

I would like to draw attention to the connection between the different lengths of the legs and the numerous musculoskeletal and neurological pains that patients complain about,' says Vladimir Nechaev. – I often see anatomically caused leg shortening in patients who come with chronic complaints and back pain. Unfortunately, they are often prescribed expensive and unnecessary equipment and laboratory tests. In the case of conspicuous clinical symptoms, proven and accurate manual assessment methods are of great importance.
The so-called 'back pain test' has proven to be a good diagnostic method. Block, block position and block flexion method. In the block position method, special plates (blocks) are gradually placed under the heel of the shorter limb. The extent of the correction is assessed visually and by touch.
In the block and flexion method, the flexion test is repeated with the patient standing with feet shoulder-width apart and successive blocks of 2, 4, 6, 8, and 10mm placed under the heel until a negative flexion test on the side of the shorter leg is achieved. The visible results of this test make it possible to understand the cause of the impairment and then to develop the most effective treatment strategy.
A postural x-ray and other assessment methods may also be used.
Caused
Various congenital and acquired orthopedic diseases and injuries are responsible for shortening or deforming the limbs. The cause of shortening and deformation of limbs in congenital diseases can be due to abnormalities in the formation and development of the embryonic zone during embryogenesis and various genetic defects. This group of diseases includes abnormalities such as congenital shortening of the thigh, lower leg, upper arm, and forearm, congenital labral deformity of the femoral neck, and longitudinal ectromelia of the lower leg. Congenital shortening includes various forms of bone dysplasia (osteogenesis imperfecta, etc.), epiphyseal dysplasia (spondylo-epiphyseal dysplasia, etc.), metaphyseal dysplasia (Olier's disease, etc.), physeal dysplasia (Blount's disease, etc.), chondrodysplasia (achondroplasia, etc.) ) and mixed forms (Volkov's disease, etc.).
Deformities and shortenings that occur after birth are called acquired deformities. Growth malformations can be caused by trauma (osteoepiphysiolysis), infectious diseases (hematogenous osteitis), neurological pathologies (cerebral palsy, polio) and cancer. Various metabolic diseases such as rickets, phosphate diabetes, de Toney-Debre-Fanconi syndrome and others lead to the development of limb deformities. Unfortunately, defective fractures also lead to shortening and deformation.
diagnosis
The diagnosis of a limb deformity or shortening is made on the basis of the medical history, physical examination, an X-ray and, if necessary, a computed tomography. In any case, the cause of the deformation and shortening must be determined, since the nature of the underlying disease has a significant impact on the patient's treatment. In some cases, biochemical and genetic testing is required for differential diagnosis.
Correction of deformity (reconstruction) of the limb can be done by two approaches - one-stage or step-by-step. In the first approach, a corrective osteotomy is performed, the axis of the limb and the correct orientation of the joints with respect to this axis are restored, followed by plunge fixation of the bone fragments in the position achieved with an LCP plate or intramedullary fixation with a locking pin. In some cases, due to the severity of the deformity or in combination with a shortening of the limbs, it is not possible to correct it in one step. In these cases, a second approach is stepwise correction with external fixation (Ilizarov method). This procedure involves using an external fixation device, performing an osteotomy (cutting the bone), and then working with the device to position one bone fragment relative to the other in a dosed corrective position. When the limb is shortened at the same time as the deformity is corrected, the bone fragments are separated (distraction) to create regenerating bone in the space (distraction). In this case, the lengthening of the limb occurs simultaneously with the elimination of the deformity. Both the Ilizarov apparatus and the new generation of orthopedic hexapods are used as external fixators: the Ortho-SUV apparatus, the use of which is based on computer navigation. In all cases, preoperative planning is performed using the CORA method.'CORA' (CENTER OF ROTATION OF ANGULATION), developed by Dr. D Paley. For this purpose, full-length X-rays of the limbs (FLFS) are taken and evaluated with the special software TrumaCad, MediCad.
Read more:- longitudinal ectromelia.
- ectrodactyly.
- One leg is shorter than the other.
- Shortening of the lower limbs.
- How to balance leg length.
- How to determine the type of pronation.
- On the short leg.
- difference in leg length.
