It is not advisable to walk with a crutch if you have a lot of weight. A crutch can carry 80 to 120 kilograms. This means that a pair of crutches can carry twice as much weight. You should learn to walk on 2 crutches at the same time to avoid damage to the crutches.
- An amputation is an operation in which all or part of a limb is removed. Amputation may be necessary if you have suffered a serious injury or infection, or have a condition such as peripheral artery disease (PAD).
- Common types of amputation include:
- Preparing for surgery
- Amputation – surgery for bone cancer
- Toilet seat extension
- Who is it recommended for?
- Benefits of using
- Tips for choosing
- Toilet handrails
- Who is recommended?
- Suggestions
- How long do you have to walk on crutches after a fracture?
- How to walk with elbow supports (sticks).
- Symptoms of phantom pain
- Where phantom pains come from
- rehabilitation
- testimonials
- Consequences after the removal of the uterus and ovaries
- Menopause after removal of the uterus
- Causes of the disease
- symptoms of pathology
- Fistulas on the foot: causes, symptoms
- Symptoms of fistulas
An amputation is an operation in which all or part of a limb is removed. Amputation may be necessary if you have suffered a serious injury or infection, or have a condition such as peripheral artery disease (PAD).
Many people lead healthy, active lives after an amputation, but it can take time for them to adjust to life without a limb.
An amputation is an operation in which one or more limbs (external limbs) are completely or partially removed.
Common types of amputation include:
- Transfemoral amputation, in which part of the thigh, knee, shin, foot and toes are removed.
- Amputation below the knee, removing the shinbone, foot and toes.
- Amputation of the hand.
- Amputation of the hand.
- Amputation of fingers.
- Amputation of the foot, removal of part of the foot.
- Amputation of a toe.
Amputation may be necessary to prevent infection from spreading to the limb and to relieve pain.
The most common cause of amputation is a non-healing wound.
The cause of this is often insufficient blood flow to the affected limb.
After a serious injury, e.g. B. a contusion, amputation may be necessary if the surgeon cannot repair the limb.
Preparing for surgery
Before surgery, the patient must undergo a series of diagnostic procedures to confirm the diagnosis and determine the appropriate level of amputation (MRI, blood tests, etc.) so that as much healthy tissue as possible can be preserved and the cancerous tumor can be completely removed. To assess the patient's condition, tests can be carried out:
- A thorough physical examination - to assess the patient's physical condition as well as nutritional status, bowel, bladder, cardiovascular and respiratory function.
- Examination of the condition and function of the healthy limb.
- Psychological assessment – required to determine how the amputation affects the patient's mental and emotional health and whether they require additional support.
The patient should also inform the doctor about the following factors:
- Allergic reactions to medications, anesthetics, latex.
- Pregnancy or suspected pregnancy.
- Circulatory disorders and taking medications that affect blood clotting (anticoagulants, aspirin). It is likely that the patient will need to stop taking blood thinning medications before surgery.
Amputation – surgery for bone cancer
The operation can be performed under general anesthesia or epidural anesthesia (spinal anesthesia). During the operation, the patient's heart rate, blood pressure and breathing are continuously monitored. A bladder catheter may also be inserted.
First, the surgeon treats the surgical field with an antiseptic solution and makes an incision at the amputation site, after which he removes the diseased area - the cancerous tumor and the surrounding healthy tissue. This is necessary to stop the pathological process and prevent possible recurrence of the disease.
Once the surgeon is satisfied that the malignant cells have been removed as accurately as possible, he flattens the bone and forms a rudimentary limb to which a prosthesis is then attached. This creates a flap of muscle, skin and connective tissue that covers the end of the bone. The doctor then sews the stitches, which remain in place for a month. A tight bandage or cast is often used to prevent the limb from swelling.
Toilet seat extension
With the help of special toilet attachments, the height of a standard toilet bowl can be raised to make the task easier for people who cannot sit or sit down because they are physically unable to do so.
The attachment adapts to the contour of the toilet bowl, giving the impression that the toilet bowl has been 'raised'. Some attachments have a side handrail that the person can hold onto when entering and exiting the toilet. The accessories also differ in the type of attachment, which can be permanent (i.e. it cannot be removed too often) or temporary (it is attached only when the disabled person uses the toilet).

Who is it recommended for?
Indications for using a toilet seat include the following medical conditions:
- Osteoarthritis of the knee or hip, stage II or higher;
- degenerative and dystrophic diseases of the spine (osteochondrosis, intervertebral fractures, radiculitis, lumbago);
- Rehabilitation period after operations and/or injuries to the lower limbs, spine or abdomen;
- Paralysis or prosthesis of the lower limbs
- amputation of a lower limb;
- Significant impairment of physical performance.
Benefits of using
The main purpose of the toilet head is to relieve pressure on the injured body part commonly used for traditional toileting (legs, stomach or back). The absence of significant physical exertion, which undoubtedly includes squatting, improves the overall clinical or medical-rehabilitative prognosis.
In the case of irreversible disabilities, the slipper makes it easier to go to the toilet and protects to a certain extent against falls due to balance disorders.
Tips for choosing
The most important criterion for choosing a toilet seat attachment is the height of the product. Ideally, the attachment should result in the person sitting on the 'extended' toilet seat having their hips together with their knees at an angle of at least 90⁰.
Toilet handrails
A toilet railing is an easy way to provide additional support. This product is essentially a pipe with a specific shape that is attached to the side of the toilet bowl in the washroom.


By grasping the handrail, a disabled person can sit down to use the toilet without putting undue strain on their legs, spine or stomach, and then stand up again using the strength of their arms, which is the main advantage of this product.
Who is recommended?
The installation of a handrail requires a permanent disability, whereby the ability to move independently must be maintained, and is therefore recommended for the following illnesses
- Degenerative-dystrophic diseases of the spine and/or joints of the lower limbs, requiring limitation of physical activity to a minimum;
- Partial or total amputation of a lower limb;
- prosthesis of one or both lower limbs;
- Moderate degree of physical impairment.
Suggestions
When choosing a handrail for a toilet, the following two features should be considered:
- The maximum permissible load on the product must correspond to the body weight of the disabled person, otherwise the fastening may fail and the handrail may come loose.
- Ideally, the handle should be made of non-slip material to prevent accidental slips and falls with wet hands.
It is also advisable to ensure that the fixing method provided by the manufacturer is secure so that you do not have to resort to local 'craftsmen' to give the handrail the right level of strength.
How long do you have to walk on crutches after a fracture?
In case of a hip fracture. First, skeletal traction is performed. This takes between 1.5 and 2 months. After this time, a plaster cast is applied and you can only put weight on the leg again after three to four months.
The fracture of the femoral neck is treated in different ways:
- Immobilization – a plaster cast is applied and the leg is immobilized. It is not recommended to treat a femoral neck fracture this way because muscle loss can occur.
- Osteosynthesis – the bone fragments are reduced using screws or pins. This method is slightly better, but scarring may occur.
- Endoprosthesis – a metal prosthesis is inserted. This is the best option. However, walking with crutches is also required here. 3-6 months.
If ankle fracture If treated without a cast, you will only need to use crutches for 1.5 to 2 months. With a cast and surgical treatment, this time can be slightly longer, 2-2.5 months. In the worst case of skeletal traction, the treatment time can extend to 4-6 months.
How to walk with elbow supports (sticks).

Walking with elbow supports is not much different than walking on crutches. If you have weak hands, you should prefer armpit crutches. This makes walking easier.
Elbow crutches have the advantage that they are lighter and take up less space.
You can read about walking techniques at the beginning of this article. It is important to choose the right size crutches. When walking with crutches, the weight of the load is not on the armpits, but on the hands.
How to find the right elbow supports:
- Stand upright with the tip of the crutch about 6 inches from your foot.
- Bend your arms 15-20 degrees at the elbows.
- The cuff that wraps around your forearm should be 5-10 centimeters from your elbow.
- The cuff should be neither too tight nor too loose.
Symptoms of phantom pain
Phantom pain is an extremely worrying phenomenon. They may be persistent or intermittent; they may burn, be experienced as painful cramps, or feel like an electric shock. The intensity of the pain can be very severe. The prerequisite for phantom pain (in contrast to stump pain) is that the patient does not feel any pain in the area of the surgical wound. The patient feels that the amputated or missing part of the limb hurts. However, the pain can often be described in a very specific way. For example, an amputee may experience pain in the missing foot that is equivalent to stepping on a nail with the sole of the foot.
Another specific symptom of phantom pain is that touching other, healthy parts of the body can trigger an attack. For example, touching the cheek causes phantom pain in the amputated hand. Physiological processes such as urination and bowel movements can also trigger a pain attack.

Where phantom pains come from
Phantom limb pain is reportedly more common in patients who have suddenly lost a limb and were experiencing severe, acute pain at the time of injury. This is the case in armed conflicts, explosion injuries, natural disasters and industrial accidents. When routine amputation is performed on a patient suffering from a chronic illness that requires the removal of part of a limb, phantom limb pain is much less likely to occur. This phenomenon is directly related to the mechanisms of phantom pain.
The nature of phantom pain is very complex and represents a multi-layered change in the nervous system at the level of damaged nerves in the limb, spinal cord and cerebral cortex. Changes at the level of the cerebral cortex are now considered the main cause of phantom pain.
There is a special area in the cerebral cortex called the somatosensory cortex. This area receives signals from sensitive receptors located in the skin, joints, and muscles of the body. Each anatomical area sends signals to a precisely defined area of the cerebral cortex. In all humans, the cerebral cortex is organized almost identically in this respect. A 'sensitivity homunculus' is used to represent the distribution of the sensitivity zones. This is shown in the figure in section.
After a sudden amputation, the sensitive area of the somatosensory cortex, which is responsible for the amputated part of the limb, begins to experience a deficit of information - signals originating from the missing limb. A process such as the reorganization of the somatosensory cortex plays an important role in the development and maintenance of phantom limb pain. As this occurs, the zones adjacent to the amputated limb (e.g., the facial sensory zone adjacent to the hand zone) begin to expand toward the cortical area that previously received signals from the amputated limb. This leads to a distorted body schema and inadequate evaluation of tactile and other stimuli from certain anatomical areas of the body. Simply put: the area responsible for interpreting signals from the amputated limb begins to receive signals from other anatomical areas, but is unable to adequately process this information and interprets it as pain in the amputated arm or Leg.
rehabilitation
You can resume your normal life three to five days after the operation. However, to avoid complications, you should follow the following recommendations:
- Taking blood-thinning medications such as anticoagulants and agents to normalize blood circulation in the limbs, as recommended by your doctor;
- taking vitamins and antioxidants to stimulate the immune system;
- Wearing compression garments for the first three days after thrombectomy;
- Avoid physical activity for a month after surgery and then do gentle exercises to tone the leg;
- Follow a sensible diet;
- Avoid hot baths, saunas and steam rooms;
- Do your own physiotherapy and light massage;
- Avoid bad habits such as alcohol and smoking.

The duration of the rehabilitation period is determined individually and depends on the patient's condition. Visit your doctor for a check-up a few months after your thrombectomy.
The operation does not solve the problem of blood clots, so after the operation it is necessary to return to drug treatment of the veins of the lower limbs.
testimonials
Many patients have already tried surgery to remove blood clots. Most patients respond positively to the operation.
My mother's legs had been hurting for a long time, so the question of treatment was open for a long time. And after another visit to the specialist, it turned out that she had an aggravated thrombosis and conservative methods would no longer help her. The doctor suggested surgery and a classic procedure was chosen with an incision in the affected blood vessel. It took several months for her to fully recover, but the problem is now resolved. Ms. Irina takes anticoagulants and a vitamin complex to prevent this disease.
Irina, 39, Ryazan.
I was diagnosed with thrombophlebitis a long time ago, so thoughts of treatment had been floating around in my head for a long time. After researching online, I visited my doctor, who explained to me modern methods of removing blood clots. I hesitated for a long time - the operation is safe but expensive - but the doctor convinced me to do it. It turned out that I had nothing to worry about - for the first few days I had to wear compression stockings, and after a few days I was able to move freely, do gymnastics and lead a normal life.
Mikhail, 54, Novy Urengoy.
Blood vessel problems in the legs may require surgery. Thrombectomy is the modern method to eliminate a thrombus, eliminate pain and tension in the legs and protect against complications that can lead to circulatory disorders. The optimal method is endovascular surgery, in which general anesthesia is not required and postoperative vascular healing occurs in the shortest possible time. A phlebologist and vascular surgeon should be consulted before the procedure.
Consequences after the removal of the uterus and ovaries
The fear of many women about removing the uterus and ovaries is that the quality of life could be significantly impaired and incomplete. In reality, after a recovery period, patients return to their normal lives, but without pain. The most important consequence of removing vital organs is loss of fertility, which is difficult for girls who have not yet given birth and are young. A woman undergoing such a procedure should remember that it prevents the development of cancer and saves her life.
The occurrence of complications after hysterectomy and oophorectomy depends on the characteristics of the body and appropriate rehabilitation. But even if the regulations are followed, complications such as inflammation, abdominal pain during wound healing, blood clots, bleeding and urinary tract disorders can occur. In addition, after amputation of the uterus and ovaries, menopause occurs earlier, which is largely psychological. If complications arise, it is important to see a doctor to resolve the problem.
Menopause after removal of the uterus
Surgical menopause is one of the consequences of uterine and ovarian amputation. It is a condition that occurs in every woman at a certain age. If surgery removes only the uterus but leaves at least one ovary and fallopian tube intact, menopause occurs naturally at a genetically determined age.
Menopause after a uterine amputation with preservation of both ovaries is more difficult to endure. During natural menopause, hormone production in the ovaries gradually decreases over several years. When the uterus and adnexa are removed, rapid changes in the hormonal balance occur, making menopause more difficult for the patient to endure, which is particularly true for women of childbearing age. In the first days after surgery, the first symptoms of surgical menopause may appear: increased sweating, frequent hot flashes, emotional instability, dry skin, brittle hair and nails, reduced sex drive, depression.
After removal of the uterus and ovaries, hormone replacement therapy is required, which involves injecting hormones from outside the body. This therapy helps to compensate for the loss of hormones that the body no longer produces. Not all patients suffer from menopausal symptoms. Hormone replacement therapy is part of a complex of measures for women after menopause. Patients are also recommended to follow a diet, eliminate bad habits and exercise in moderation.
Causes of the disease
Why does a large toenail grow in? There are several groups of causes for this condition.
On the one hand, there are external causes for ingrown toenails, such as improper nail care and uncomfortable shoes. On the other hand, there are diseases that promote onychocryptosis.
- Improper hygiene measures and pedicures. One factor that causes ingrown nails is negligence in cutting the nails. For example, you accidentally or intentionally cut into the corner of your nail and don't notice the resulting burr or sharp edge. A badly ingrown nail also occurs when the nails are cut too short. Ignorance of the rules for foot care leads to inflammation and ingrown nails.
- High strain on the feet. An ingrown nail can be caused by excessive stress on the feet due to work or other circumstances. This refers to the pressure that the body puts on the feet and nail plate, which inevitably affects the growth of the nail.
- Uncomfortable or tight footwear. Wearing smaller shoes reduces the space for the toes, putting the nail plate at risk of abnormal growth. And a narrow shoe nose makes the situation even worse: the toes are forced and the nail does not grow according to the norm.
An ingrown nail can occur as a result of certain pathological conditions:
- Flat feet and clubfoot. The deformation of the foot creates increased pressure on the second toe and causes the big toe to bend.
- Pregnancy and postpartum period. It is not uncommon for nails to grow into women's skin during pregnancy or within a month after delivery.
- Abnormalities associated with metabolism and oxygenation of the nail plate. Diabetes, cardiovascular disease and endocrine disorders result in the nail not receiving enough minerals for proper growth and development. Obesity is also a common cause of brittleness, brittleness or complaints that the nail has grown into the skin.
- Treatment of cancer. Radiation or chemotherapy causes significant damage to body systems and organs. This also applies to the nail plate - it can grow in due to the pathological direction of growth.
- Fungal diseases. As a result of fungal infection, the nail thickens and the nail plate loses its anatomical shape. In this case, the nail grows in, which is very uncomfortable for the person affected.
- Overgrowth of the soft tissues in the nail bed. This disorder is considered a congenital trait. If the ingrown nail becomes infected and unpleasant symptoms appear, the alarm should be raised.
- Dermatological pathology. Certain dermatological diseases such as psoriasis, various types of shingles and warts can affect the growth of the nail plate.
- Mechanical trauma to the extremities. Trauma or frostbite to the fingers can lead to ingrown nails. In this case, qualified medical care is essential.
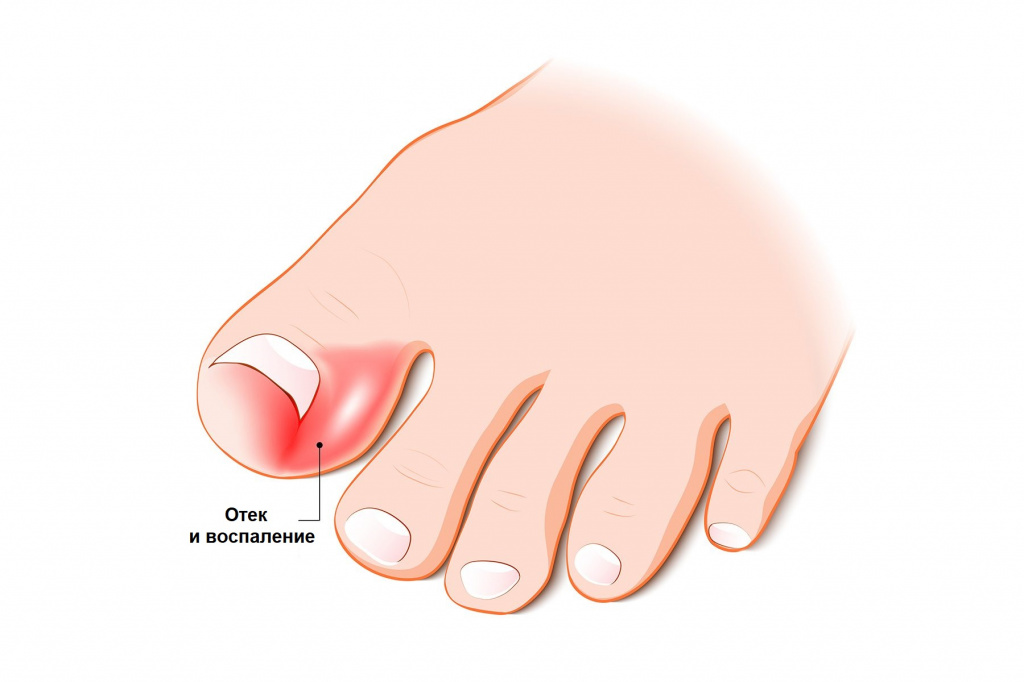
symptoms of pathology
How to tell if a nail is ingrown...? The patient feels the typical symptoms of the disease:
- Intense pain syndrome. The patient feels severe pain in the nail area, which increases when walking or wearing street shoes. The pain is associated with the inflammatory process, and tight shoes aggravate the situation: the space between the toes is reduced and pressure is put on the ingrown nail plate.
- Redness, swelling and bright pulsation in the nail area indicate the need for urgent medical intervention: the pathology can be complicated by an infectious process.
- Purulent discharge under the nail plate is a sign of infection in the inflamed area. Urgent treatment of the ingrown nail and consultation with a doctor are required.
- Formation of small ulcers. Ulcers form when the ingrown nail has been exposed to trauma or mechanical impact (severe impact or crushing).
- Growth of abnormal tissue around the nail – the patient should pay attention to this symptom as such tissue looks like raw meat.
- Impairment of the normal shape of the nail plate. The nail may shrink in length, its thickness increases, and the soft tissue thickens - these symptoms indicate that the disease has acquired a chronic form.
Treatment can be therapeutic and non-surgical if you consult your doctor in a timely manner. The doctors of the medical center in Minsk 'Clinic in Uruch' will help you treat onychocryptoids quickly and painlessly!
Fistulas on the foot: causes, symptoms
A fistula is an opening through which body cavities or organs communicate with each other or with the external environment; normally they are not present. The most common cause of fistulas is the purulent dissolution of tissue. When inflammation occurs in a closed space, it either shrinks (closed abscess) or spreads through tissues and cavities (phlegmon), but sooner or later it still discharges pus into the surrounding area, either through natural openings or through fistulas.
- Bone inflammation (post-traumatic, endogenous, etc.)
- diabetes
- Infection as a result of osteosynthesis
- purulent abscesses in soft tissue infections
Symptoms of fistulas
- Hole in the skin
- purulent discharge from the opening
- intermittent pain in the fistula area
- Weakness, fatigue, subfebrile fever and other symptoms of intoxication
A fistula is a constant source of infection and indicates a weakened immune system, which is why its treatment is essential! Ideally, the problem should be treated by a qualified doctor, a surgeon in collaboration with an immunologist, endocrinologist, etc.
If a patient is diagnosed with a leg fistula, treatment consists of the following steps:
- Treatment of the underlying disease (diabetes, etc.)
- Immunomodulators
- Systemic and topical antibiotics for the treatment of chronic infections and the fistula itself
- vitamins
- Physiotherapy (laser, etc. in the fistula area) without active inflammation
- Topical treatment (ointments, rinses, etc.).
If the fistula has existed for a long time or the patient's immune system is extremely weakened, the fistula rarely closes spontaneously and then requires surgical treatment: removal of the fistula, drainage of the purulent cavities and sanitation of the source of infection. Sources of infection can be osteosynthesis constructs (plates, pins, wires, staples), foreign bodies, unrepaired bone fragments, etc. Only a highly qualified surgeon is able, based on the patient's history and scans (endoscopy and fistulography), to suggest and perform an effective surgical procedure that eliminates the problem instead of creating a new one.
We are committed to providing high quality service. We would like to thank our patients for their trust and feedback on our medical center.
- The reamputation is.
- Medial sphenoid of the foot.
- Where do the body parts go after the operation?.
- What to do with amputated limbs?.
- Life after a leg amputation.
- Limb amputation.
- The toe formation.
- Indications for amputation.
