After a shoulder injury, whether it's a fracture or a dislocation, your life can change for weeks or even months. Most shoulder injuries, regardless of treatment tactics chosen, typically require immobilization for a period of time before rehabilitation begins.

- Dislocated shoulder
- author
- causes
- causes of occurrence.
- types of deviation
- causes
- diagnosis
- Specific symptoms: Dislocation of the shoulder joint (shoulder dislocation)
- collarbone fractures
- diagnosis
- Treatment
- Conservative therapy
- General information.
- treatment methods
- Types of surgical interventions
- Operations on muscles and tendons
- Types of habitual dislocations
- Symptoms of a habitual dislocation
- Main benefits of shoulder arthroscopy
- If an operation is necessary
Dislocated shoulder
Shoulder dislocations are more common in younger patients. Recurrence is very common after the first dislocation. The younger the patient, the greater the likelihood that they will dislocate their shoulder again. Between the ages of 16 and 30 the probability of dislocating the shoulder is 67 %, after the age of 40 it is 38 %. If the shoulder becomes unstable, surgery can prevent recurring dislocations.
Shoulder dislocations are more common in younger patients. Relapses are very common after the first dislocation. The younger the patient, the greater the likelihood that the shoulder will dislocate again. Between the ages of 16 and 30 the probability of a renewed shoulder dislocation is 67 %, after the age of 40 it is 38 %. If the shoulder becomes unstable, surgery can prevent recurring dislocations.
- Affordable Clinical consultation with an orthopedic trauma surgeon, MD from 4,000 rubles
- Urgent Prompt appointment on the day of treatment
- Near 8 minutes from Prospekt Mira metro station
- Comfortable Individual appointments by arrangement
Shoulder dislocations are more common in young patients. After the first dislocation, there is often another dislocation. The younger the patient, the more likely it is that the shoulder will be dislocated again. Between the ages of 16 and 30 the probability of a shoulder dislocation is 67 %, after the age of 40 it is 38 %. If the shoulder becomes unstable, recurrent dislocations can be stopped with surgery.
As a specialist clinic for traumatology and orthopedics, we are familiar with joint pain and know how we can help you. Our patients receive 24-hour care until they are fully recovered.

author

causes
When a person experiences a dislocated shoulder for the first time, there's a good chance it's the result of trauma. Even if the shoulder is dislocated with little effort, the head of the humerus will detach from the base of the shoulder blade.
Anterior dislocations account for 90% of all dislocations. It occurs at 1.7 % of all humans. The type of injury and treatment depends on the future stability of the shoulder joint. Joint instability is common. The instability manifests itself not only in repeated dislocations, but also in painful clicking movements and transient subluxations (displacement of the humeral head during large-amplitude movements). The constant fear of a dislocation again forces those affected to limit their physical activity and give up sports.
Why does a recurring shoulder dislocation occur? It is the result of a loss of stability. Stability is ensured by multiple anatomical structures. The deltoids and rotator cuff only prevent the shoulder from folding out when it's extended to 90 degrees. From this point, movement is restricted by the synovial membrane of the scapula and the joint capsule. The joint capsule acts like a 'hammock', holding the humeral head in place and preventing it from deviating excessively.
If the shoulder occasionally jumps out of the joint after the first dislocation, the causes may be one of the following
- tearing of the joint jaw;
- damage to the joint capsule of the shoulder joint;
- damage to the long head of the biceps and rotator cuff;
- muscle imbalance between the internal and external rotators of the shoulder;
- broken bones (articular surface of the shoulder blade or humeral head);
- Increased joint capsule volume.
The risk of shoulder re-dislocation depends not only on the factors that led to the injury, but also on the quality of medical care the patient received after the initial dislocation. Risk factors for instability:
causes of occurrence.
The shoulder joint is one of the most complex joints in the human body and is therefore frequently injured. It is a spherical joint surrounded by a joint capsule. The head of the humerus rests directly against the socket and the rotator cuff sits on top of it. In addition to the shoulder blade process, the bone head, the ligaments and the muscle tissue, it has a stabilizing function.
The following abnormalities can cause instability of the shoulder joint:
- dysplasia.
- Injuries to the back muscles and ligaments.
- Changed position of the head of the humerus.
- Increased Agility.
- Complications of recovery from injury.
- curvatures of the spine.
- Axial loads on the spine.
Shoulder instability can be recognized by the following symptoms:
- Formation of a bulge on the joint capsule.
- Acute pain after bumps, dislocations, bruises.
- Crunching when moving the shoulder.
- Dislocation of the shoulder joint during smooth or sudden movements.
- Regular dislocations or subluxations.
- weakness in the shoulders.
types of deviation

The type of pathology depends on the severity and type of deformity. The joint can deviate either vertically or horizontally (combined displacements also occur).
There are 3 types of anomalies, which can be caused by the following causes, among others
- Major Trauma - Dislocations or subluxations caused by blows and contusions. A dislocation occurs, causing rotator cuff instability. This leads to functional limitations and limited mobility. Gradually, scar tissue forms, progressively reducing function and causing chronic pathology.
- Stretching of the joint capsule – caused by increased mobility or regular physical activity. This leads to instability of the joint capsule, which can lead to dislocation or subluxation.
- Horizontal or vertical instability – occurs in childhood and represents hyperelasticity. It manifests itself as discomfort during exercise because the shoulder joint is severely dislocated.
causes
There are three common causes of joint instability.
severe trauma – A common cause of shoulder dislocation. A dislocation often injures the ligaments, synovial membrane, and the bone that forms the anterior rim of the socket of the shoulder joint. These injuries are sometimes referred to as Bankart injuries.
A severe primary dislocation, even after appropriate treatment, in most cases leads to future instability of the joint.
Constant overload. Swimming, tennis, and volleyball all involve repetitive overhead movements of the shoulder, which can stretch the ligaments of the shoulder joint. Many professions also require overhead movements of the shoulder. These activities put stress on the joint, weaken the ligaments and tendons, and can cause instability.
Multiplanar instability. A small percentage of patients with instability have no history of trauma and their regular activities do not result in permanent stress on the joint. However, in these patients, the shoulder can be repeatedly dislocated in multiple directions. This instability is caused by a congenital weakness of the ligaments throughout the body.
Generally Symptoms of a habitual dislocation These include pain, a history of repeated dislocations, a constant feeling of instability, and anticipation of dislocation of the joint.
In our clinic, arthroscopy and other minimally invasive methods of treating shoulder diseases are used extensively. The operations are performed on state-of-the-art medical equipment with high-quality and proven consumables, fixators and implants from the world's largest manufacturers.
diagnosis
The doctor makes the diagnosis based on the history and clinical examination.
The clinical examination includes palpating the shoulder joint area, conducting special tests, and determining strength and range of motion. These tests can be used to determine the degree of instability.
X-rays are usually taken to provide information about possible causes of instability and other causes of shoulder pain, such as: B. a fracture to rule out. Further examinations such as MRI or CT examinations are carried out to examine the soft tissue of the shoulder joint more closely and to assess the bony structures.
Specific symptoms: Dislocation of the shoulder joint (shoulder dislocation)
- Bony prominence on the anterior surface of the shoulder joint
- Inability to move the shoulder joint
- outward rotation of the shoulder
- Frozen Shoulder

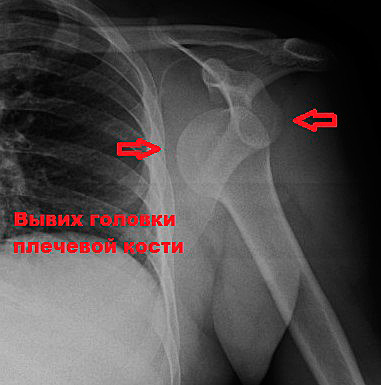
Unstable shoulder joints (as in the picture) can dislocate one of the joints in the shoulder girdle.
Most shoulder rim fractures are diagnosed by examination and x-rays. Occasionally, more complex additional examinations such as computed tomography are required to clarify the diagnosis.
collarbone fractures
Most collarbone fractures require surgery. Surgical intervention is indicated when the fracture is complex with skin trauma or a major displacement. During surgery, the bone fragments are usually fixed with a plate and screws or a rod that is inserted into the intramedullary canal of the clavicle.
Most fractures of the proximal end of the humerus can be treated conservatively if there is no displacement of the fragments. Displacement fractures usually require surgical treatment. Surgical treatment options include immobilization of the fracture with plates and screws, plexi, or a shoulder joint replacement.
diagnosis
The doctor makes an initial assessment of the condition based on a clinical examination. This includes a detailed discussion with the patient about the age and frequency of the dislocations and the strength required. A specialist is then consulted:

He makes the diagnosis
- Examine the joint;
- determining the configuration, the presence of an inflammatory reaction (reddening of the skin, swelling of soft tissues);
- assesses the ability to perform active and passive movements, as well as their extent.
- If necessary, he orders an additional objective examination to determine the nature and extent of any damage to the joint structures.
The objective diagnosis is made using imaging techniques such as X-rays (direct and lateral views), computed tomography (CT) or magnetic resonance imaging (MRI), which are slice-by-slice images of easily separable tissues, and ultrasound.
In modern medical clinics, diagnostic arthroscopy, which is the visualization of internal structures by inserting a small tube with a camera and light, is used to examine internal structures. It can be used as a curative operation (habitual shoulder dislocation). The prices for diagnostics depend on the scope and the technique used.
Treatment
The treatment of this pathological condition, in which there is a recurrent dislocation of the humeral head from the acetabulum, is complex. It includes conservative and surgical treatment and rehabilitation.
All interventions are carried out gradually and sequentially. As a rule, in the preoperative preparation phase, conservative treatment is carried out first. This is followed by the surgical treatment. This aims to restore the stability of the joint that has been disrupted by the habitual shoulder dislocation. After the operation, rehabilitation measures are carried out.
Conservative therapy
Drug treatment is usually prescribed in preparation for the operation. When there is an inflammatory response, non-steroidal anti-inflammatory drugs are used. If necessary, drugs to improve blood clotting and antibiotics to prevent secondary bacterial infections are also used.
Physiotherapeutic treatments, including electrophoresis with anti-inflammatory drugs, magnetic therapy, mud baths, ozokerite, are carried out to improve the ligamentous apparatus and increase the strength of connective tissue fibers. The range of conservative measures is usually larger when open-access surgery is planned.
General information.
The shoulder joint is the most mobile joint in the human body. It consists of the socket of the shoulder blade and the head of the humerus. The joint is stabilized and controlled by the muscles of the shoulder girdle and upper limbs and contains many tendons but almost no ligaments.

Shoulder disorders arise from trauma, strenuous physical work, and less commonly from autoimmune inflammation, infection, and metabolic disorders. The doctors in our clinic treat all shoulder diseases successfully, mostly with conservative methods.
treatment methods
Treatment of shoulder diseases can be carried out using both conservative and surgical methods.
At the clinic of Dr. Glazkov prefers conservative therapy. We use the following methods:
dislocation of the limb. Effective in conditions associated with long-term microtrauma. In addition to load limitation recommendations, orthoses that limit unwanted movement and kinesiology taping can be used.
Medical therapy. Patients are prescribed non-steroidal anti-inflammatory drugs (NSAIDs), and depending on the cause of the disease, muscle relaxants, glucocorticoids, agents affecting uric acid metabolism, antibiotics, etc. are also used. The drugs are mainly taken orally. Occasionally, intramuscular or intravenous injections are also required. Drugs to be applied externally are also used, but their effectiveness is usually low. Some people get relief from warming creams (topical irritants).
Massage. Used to relax muscles, improve blood circulation and relieve pain.
Physical therapy. In the acute phase of inflammation or injury, cooling treatments are effective. This reduces pain, swelling and inflammation. A few days after the injury or operation and in the case of chronic diseases, 'warming' variants of physiotherapy, such as laser therapy, are used. In addition, in our center we use a very effective method of physiotherapy for shoulder diseases - shock wave therapy. With this technique, the tissue of the shoulder joint is damaged on a micro level, which stimulates repair processes. Shockwave therapy reduces pain and inflammation.
joint puncture. May be needed in trauma to remove blood, in synovitis to remove inflammatory fluid from the joint. With purulent shoulder arthritis (septic arthritis), joint puncture is considered a mandatory procedure. It is important not only for treating the disease, but also for diagnosis, as doctors can identify which bacteria are causing the inflammation and obtain data on the susceptibility of the isolated germs to different antibiotics in order to determine the best drug to kill them to select.
Types of surgical interventions
In modern traumatology there are about 300 surgical procedures that are used for frequent shoulder dislocations. All surgical options can be divided into three groups: capsule, tendon and muscle and bone. The various surgical treatment methods can be combined with each other (e.g. capsule reinforcement with simultaneous tendon and muscle stiffening, etc.). Anesthesia or general anesthesia is used as a method to treat pain in operations for habitual shoulder dislocations.
These include the techniques according to Turner, Putty and Boicev I. In the Turner operation, the lower pole of the joint capsule is sutured. The procedure is performed through a longitudinal incision in the armpit and is not commonly performed because of the proximity of the neurovascular bundle. In the Putti procedure, the joint is opened wide with an anterior or T-shaped incision, overlapping the outer and inner edges of the capsule and reinforcing duplication of the remaining capsule.
The Bojčev I operation is performed through a T-shaped incision. The tip of the beak is cut off along with the muscle attachment points. A triangular flap is placed on the front of the pouch. The triangular opening is sewn up vertically. The triangular flap is pulled up and its upper part sutured to the cranial process. The muscles cut off at the beginning of the operation are then sewn back on.
Operations on muscles and tendons
This is the largest group of interventions for frequent dislocations of the shoulder joint. It includes the following techniques:
- Boicev II operation. It is performed through an anterior approach. A tunnel is made under the scapular muscle to the styloid process. Muscles that have an attachment point at the top of the metacarpal process are loosened, guided through the created tunnel and reattached to the attachment point.
- Weinstein operation. It is performed through an anterior internal incision. The tendon of the long head of the biceps is advanced to the anterior articular surface and reinforced with U-shaped sutures.
- Sverdlow operation. The joint is opened via an internal anterior approach. A tendon-muscle flap is formed from the tendons of the beak muscle and the short head of the biceps. The muscle defect is sutured. A tourniquet is formed from the flap. Just below the head of the humerus, a hollow is created to the inside of the tuber, into which the newly formed ligament is inserted.
- The Gurov operation is performed through an anteromedial approach. The joint capsule is reinforced with a tendon-muscle flap formed from the scapular muscle.
- The Bratanchuk procedure is performed through an anteromedial approach. The tendon of the scapular muscle is cut and the two heads of the biceps muscle are slipped underneath. The tendon is then sewn up over the heads.
Types of habitual dislocations
As with the primary shoulder injury, the following subtypes are also distinguished with the habitual dislocation:
- anterior The most common case, since the humerus is weaker at the back due to ligaments and tendons and a less pronounced head of the deltoid muscle, including in athletes. It occurs during batting, wrestling, or ring or horizontal bar exercises.
- The backstage area. In this case, the front part of the joint capsule is damaged and the head of the humerus turns backwards unnaturally. The shoulder is dislocated forward and forward. This can be caused by the arm falling onto the straight arm or by improperly distributing the dumbbell on the bench press.
- deeper. The head of the joint bone slides under the notch of the shoulder blade. Rarely occurs when the arm is raised, e.g. B. when walking on the hands.
In a habitual dislocation, it is not uncommon to have a combination of these conditions.
Symptoms of a habitual dislocation
The symptoms of a habitual dislocation are less pronounced than those of a primary injury.
- Pains. It may be mild or absent with only mild discomfort in the injured shoulder. The more frequent the habitual dislocation occurs, the less pain there is, which is due to the degenerative processes of the cartilage tissue and articular apparatus associated with the pathology.
- external deformation. A habitual dislocation is recognizable by the angular contour of the joint.
- Impaired motor function due to pathologically abnormal alignment of joint components, constrained posture of the limbs. The arm is usually pressed tightly against the trunk or is displaced to the side.
- Sometimes there is a temporary loss or reduction of feeling in the arm (hand, forearm, shoulder, skin) due to the compression of the nerve bundle.
- There is no local swelling initially, but it can develop if not treated properly or if the patient does not self-heal. Over time, this can develop into an extensive bruise at the injured area.
Main benefits of shoulder arthroscopy
Arthroscopy of the shoulder area has several advantages over open joint surgery, which greatly facilitate the surgeon's work and the patient's recovery. The arthroscopic technique is used in the majority of clinical cases; open surgery is used for ankylosis, fibrosis and other serious complications of the disease. The main benefits of the surgery are summarized below:
– Reduced anesthetic stress;
– Inexpensive treatment; – rapid intervention; – reduced risk of postoperative complications; – shorter rehabilitation time; - good aesthetic effect;

Due to the excellent visualization of the intra-articular tissue, several joint surgery problems can be solved simultaneously. Thanks to this unique device, the surgeon can use the laparoscope to perform microsurgical interventions without injuring the large vessels with bleeding and without touching the large nerves, which are particularly numerous in the shoulder due to the brachial plexus. The greatest challenge in hand surgery is the large number of vessels and nerve bundles that lie on the surface of the tissue. Damage to even one of these vessels results in severe hand deformities, neuralgia, myofascialization, and paralysis that require separate surgical intervention by a neurosurgeon. Therefore, subtle manipulations with the arthroscope ensure that nearby nerves are not damaged.

It takes doctors about an hour or more to complete an arthroscopy, so many patients can be operated on in a day. Patients benefit from the fact that deep sedation is not used, rather than heavy anesthesia, so arthroscopy is indicated for patients with severe lung, heart, liver, or kidney disease. Even if the surgery is to be performed on a very frail patient, the doctor often chooses arthroscopy to avoid complications after anesthesia.
If an operation is necessary
Surgery is the method of choice because it has practically no disadvantages. For example, if a patient complains of pain, the diagnosis of joint damage is often made by arthroscopy. Arthroscopy allows high-quality visualization of the underlying cartilaginous tissue of the articular surfaces, synovial membrane and intra-articular pathological formations.

In all patients, an X-ray in two projections of both shoulder joints and, for certain indications, computer tomography or magnetic resonance imaging are first carried out for diagnosis. Diagnostic arthroscopy is also used for pathologies such as shoulder joint instability, humeral head fractures and to identify bony deficits in the shoulder joint socket. Arthroscopy is also used to clarify the location of osteophytes, corpus cartilage and other pathological intra-articular masses, since due to the complex configuration of the joint, even such a sensitive procedure as computed tomography is not enough to locate a mass with millimeter precision, which is essential for planning a surgical one intervention and is therefore essential for the selection of the approaches.
Another important indication for arthroscopy is a pronounced pain syndrome, the cause of which is not known for sure. The goal of arthroscopy is to find and eliminate the cause of the pain. In most cases, they are caused by pathological intra-articular masses or neuralgia due to a compressed nerve.
Statistically, arthroscopy is most commonly used for unstable shoulder joints or, more commonly, for recurrent shoulder dislocations. The main indication is repeated dislocation of the shoulder joint, which is accompanied by dysplasia of the articular surfaces and causes unbearable pain. The operation consists in dividing the capsular complex at the level of the labrum tear and then fixing it in the right position with special fixation devices. A distinction is made between an anterior and a habitual posterior dislocation. For anterior dislocations of the shoulder joint, arthroscopy aims to restore alignment of the labrum as described above.
Read more:- Diagram of a joint with and without a dislocation.
- How much does shoulder surgery cost?.
- tearing of the joint capsule.
- Pronation of the shoulders - what is it?.
- This is what a dislocated leg looks like.
- How do you treat a sprained ankle?.
- How much does bunion surgery cost?.
- tarsal joint.
