One of the most effective band protectors is Artracam..
- Skier's thumb
- Acute thumb injury
- Types and causes of tendon injuries
- What are the symptoms of a torn tendon?
- Treatment of the different degrees of muscle tears
- prevention
- Diseases
- ailments and symptoms
- Diagnosis
- our prices
- Types of groin joint injuries
- Treatment of broken lanyards
- Arthroscopic reconstruction of the anterior cruciate ligament
- Preparation
- surgery
- Efficacy of surgical treatment of ACL rupture
- Priorities for a successful ACL reconstruction operation.
- finger tendon injuries; general information and special features
- Symptoms of a torn finger tendon
- Use of orthopedic splints for toe tendon tears
- surgical
- Conservative
- Immobilization – a prerequisite for recovery
- Treatment of a torn meniscus in the knee
- Physiotherapy for a meniscus tear
- Prevention of a meniscus tear in the knee joint
- DIAGNOSIS OF AXLE INJURIES
- CONSERVATIVE TREATMENT OF ACL INJURIES
- RECURRENT CRUCIAL LIGAMENT RUPTURE
- First phase of the operation Revisionplasty of the anterior cruciate ligament
Skier's thumb
Thumb injuries are often caused by falling with the hand resting on an object (e.g. a ski pole). Therefore, an injury to the ulnar collateral ligament of the first metatarsophalangeal joint is referred to as 'ski thumb'.
The term 'forester's thumb' can also be found in the literature. It's thought to be the same condition, but actually there are some differences. These consist of the injury mechanism, which is different for skiers and foresters.
The skier falls and suffers a torn thumb ligament, while the hunter regularly twists the rabbits' necks in such a way that the thumb experiences excessive lateral tension. This repeated microtrauma stretches the ligaments in the thumb.
As can be seen, the images of a skier and a forester were chosen to illustrate the patient model and to highlight the fundamental difference between these diseases. People who love animals and have never skied can face similar problems.
Acute thumb injury

Skier's thumb, injury mechanism.
Excessive abduction (in a fall) damages the ligament that stabilizes the thumb.

When diagnosing an acute injury, two very important questions arise: whether there is a broken bone (sometimes the ligament comes loose with a piece of bone) and whether the ligament is fully or partially torn. While the first question is easy to answer after taking x-rays, the second question is a much more difficult task as neither ultrasound nor MRI can provide an accurate answer.
These questions are critical as they influence treatment strategy.
The fracture may require surgical treatment if displacement has occurred. Namely, if the bone fragment is displaced by more than 2mm, it must be fixed in place with a screw (ie surgically). In contrast, a fracture without displacement has a good chance of healing.
Ligaments can be completely or partially torn. With a complete rupture, there is a good chance that chronic instability of the thumb will develop.
In 1962, Stener described the anatomy of a complete tear of the ulnar ligament of the first metatarsophalangeal joint.
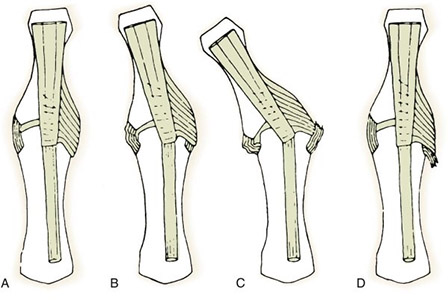
Anatomy of the ulnar collateral ligament of the first metatarsophalangeal joint.
Panel A shows the normal relationship of the ligament covered by the aponeurosis of the adductor muscle.
Panel B shows the location of a small radial detachment where the aponeurosis slides easily exposing the ligament.
Types and causes of tendon injuries
Tendons are tough connective tissue units. They represent the end portions of the muscles that attach them to the bone. An injury to the extensor tendon with a full or partial tear impairs the function of the muscle - its movements are restricted or become impossible.

- Subcutaneous closed injuries. These involve an unexpected blow to a tense muscle. A ligament tear occurs, although there is no open wound.
- open injuries. They are usually caused by cuts with sharp objects. In these cases there is always an open, deep wound.
- Phalangeal detachment injuries. These injuries are not uncommon at work: the tendon tears together with the bony muscle.
Subcutaneous tendon ruptures are less common than open injuries. Such injuries are more common in people with metabolic diseases such as diabetes or chronic kidney disease.

Fill out the form and we will get in touch with you.
What are the symptoms of a torn tendon?
Externally, a tendon rupture in the hand can be accompanied by the following manifestations:
- Suspension and deformation of the finger or fixed flexion
- Rapid decrease in arm strength - usual activities can no longer be carried out
- Sensory disturbances – fingers become numb
- Swelling and bleeding around the wound
- Dysfunction of the fingers (depending on the location of the injury site)

IMPORTANT: If you have symptoms of an extensor muscle injury, you need urgent professional help from a surgeon. Don't wait for the wound to heal and don't delay referral to a specialist practice!
Treatment of the different degrees of muscle tears
- immobilization of the injured area in a position in which the severed parts of the muscle are as close as possible;
- application of ice to stop bleeding;
- If there is an open crack, the edges of the wound should be treated with an antiseptic.
In the case of a partial tear, first aid measures may be sufficient. In this case, further fusion of the damaged tissues takes place in complete rest.
However, it is difficult for non-professionals to assess the severity of the injury.
- applying ice to the injured area on a specific schedule;
- subsequent treatment with heat;
- pain relievers and anti-inflammatory drugs;
- first rest and then physical therapy to help you work and recover.
A torn muscle fiber takes four to 12 weeks to heal and recover. This injury is dangerous in that the muscle may not heal properly, causing a lifelong defect. If you suspect that the rehabilitation process is dragging on or is not going well, you should see a trauma surgeon.
The doctor will conduct regular examinations and adjust the treatment tactics.
prevention
It is important to realize that these types of injuries (sprains, torn muscles and ligaments) are more common in physically inactive, unfit people with a sedentary lifestyle. To avoid these types of injuries, you should pay attention to your weight and fitness. Heavy physical exertion and sports activities should only be carried out after a warm-up program. Regular training that strengthens all muscle groups minimizes the risk of such injuries.
Diseases 
ailments and symptoms 
If you suffer from these symptoms, it could be a sign of an illness, which is why we recommend consulting a specialist.
Diagnosis 
our prices 
We strive to keep our prices up to date. To avoid misunderstandings, please ask the clinic for the exact prices.
This price list does not constitute an offer. The medical services are provided on a contractual basis.
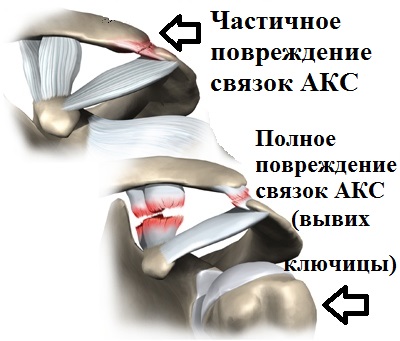
Types of groin joint injuries
Surgeons distinguish between complete and incomplete ischiofemoral joint tears. The joint injury can also result in a dislocation of the clavicle, whereby a dislocation of the clavicle upwards or forwards is also distinguished.

Depending on the degree of deformation, the rupture is divided into:
- Minor fracture without displacement of the clavicle. The crack has a minimum size of 2-3 mm;
- Moderate, resulting in ligament rupture and clavicle displacement. A widening of the joint space of up to 5 mm is noted;
- Severe, resulting in severe joint damage. The size of the crack exceeds 7 mm.
Depending on the time of injury, cracks are classified as follows.
- Fresh. The injury was sustained up to 3 days before seeking treatment;
- Continuous. The injury was sustained within 3 days to 3 weeks prior to seeking medical treatment;
- weeping. The tear occurred more than 3 weeks before seeking treatment.
Treatment of broken lanyards
A clavicle ligament tear can be treated conservatively or surgically.The treatment method depends on the extent of the injury and the condition of the injured person. Conservative treatment methods include:
For moderate tears, a bandage may be needed to protect the injured area and limit movement of the joint.
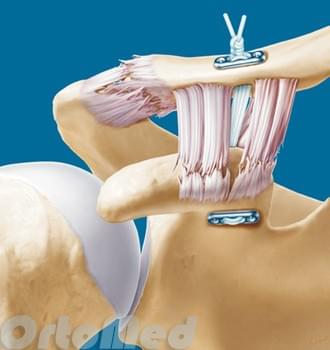
Surgical treatment involves repairing severe bony deformities. Surgery may be needed to remove the end of the collarbone and repair the ligaments.
Arthroscopic reconstruction of the anterior cruciate ligament
A reconstruction of the anterior cruciate ligament through conservative treatment is not possible - tears cannot be 'repaired' without direct access. Therefore, all repairs of the anterior cruciate ligament can only be performed surgically.
Preparation
Arthroscopic reconstruction is strongly recommended by a specialist. You are preceded by the following steps:
- Examination, collection of anamnesis.
- A consultation during which tests are carried out and any pre-existing conditions should be explained.
- blood and urine tests.
- Additional examinations (CT, MRI, X-ray, ECG).
surgery
First, the doctor makes small incisions in the skin. A fiber optic device with an integrated camera (arthroscope) and other surgical tools can be inserted into the joint cavity to reconstruct the damaged ligament fragment. The presentation is made using high-resolution images that are displayed in real time on a screen. In autotransplantation, the doctor transplants the tendon harvested from the hamstring muscle (semitendinosus muscle tendon). After the operation, the patient can go home the same day. Once the stitches are removed, the doctor guides the patient through postoperative rehabilitation so that they can quickly regain their joint function.
Efficacy of surgical treatment of ACL rupture
If a patient is attempting to return to sport, the only effective treatment option is anterior cruciate ligament (ACL) surgery. A satisfactory result is achieved in 85-93 % of surgical interventions (Hofbauer V., Valentine P., 2010; Mihelic R., Jurdana H. 2011). At the same time, in 50-70 % cases return to the previous sports level is achieved.
Reasons for not achieving maximum fitness and returning to the previous level of physical activity:
- Misjudgment of the instability variant – underestimation of the rotational stability. A ruptured ACL often occurs in conjunction with other knee joint injuries. Full functionality is not possible without rectifying them.
- Wrong reconstruction technique - surgeon's technical error or technique: fundamental - individual anatomy is not taken into account (errors in technique, 'guides', misinterpretation of the anatomical structure or negligence), etc.
- Violation of the biological conditions for the graft to be reconstructed: bone tunnel, peculiarities in the formation of the graft for subsequent augmentation and the ligament, peculiarities in its attachment (design features of the attachment devices).
- Lack of individual, adequate rehabilitation or its incompatibility with the capacity of the joint and graft.
- Lack of medical supervision of the knee and graft until full rehabilitation is complete (until the knee is acclimated and has adequate blood supply).
Priorities for a successful ACL reconstruction operation.
First and foremost is the consideration of biological processes, namely:
- Anatomy, ie the individual anatomical features of the joint – ie the correct placement of the graft. Although the knee joint is constructed in much the same way, everyone's characteristics are different, and the correct location for everyone is how the ligament was positioned prior to the injury.
- Choosing the shape and characteristics of the graft. The transplant must have an anatomically correct shape with high strength and healing.
- Creation of the biological conditions for the transplant on the bone substrate.
- During rehabilitation, it is important to have an active blood supply to allow the ligament to strengthen and fuse together.
- When active movements begin, it is necessary to ensure that the graft does not have the prerequisites for mechanical damage and retains the tension created during the operation.
finger tendon injuries; general information and special features
The tendon is the connective tissue part of the muscle that is directly attached to the bone. A tendon injury is always a tear (or cut) of the tendon tissue. There are two types of tendon injuries:
- incomplete – The tendon is partially intact and the function of the flexors and extensors is partially intact;
- Complete – The integrity of the tendon is completely compromised and the flexion and extension function is absent.
A characteristic of this type of injury is that it is virtually impossible for the tendon to heal itself without proper medical attention. This is due to the permanent contractile function of the muscle, which results in a significant diastasis (discrepancy) between the torn tendon fragments.
In the event of a finger tendon rupture, the situation is further complicated by the fact that primary tendon suturing (i.e. restoring the integrity of the tendon through surgery immediately after the injury) is required only 6-10 hours after the injury (up to 24 hours in some cases). ) is possible. If this period is missed due to increased swelling and/or hematoma, the injury must be allowed to heal completely before the patient undergoes elective surgery to suture the tendon tissue.
The second option has been shown to be the most common due to the specificity of the symptoms of a torn finger tendon.
Symptoms of a torn finger tendon
The clinical picture depends on the type of tendon injury, but the most common symptoms include.
- Impaired flexion and extension function in one or more phalanges of the finger;
- 'Sagging' of one or more phalanxes (the terminal phalanx, where the nail plate is located, is most commonly affected);
- The finger's ability to exert force is drastically reduced, to the point of total inability to exert any force.
Use of orthopedic splints for toe tendon tears
Tendon ruptures can be treated in two ways: surgically and conservatively
surgical
Sewing up the tendon with special surgical sutures. Suture is the primary and only effective treatment option for torn tendons. About 98 % of torn tendons can only be healed with sutures - and nothing else.
After the operation, patients receive long-term therapy (about 3-6 weeks) a special orthopedic splint to ensure complete immobilisation of the finger or hand, since careless movements of the finger during this period lead to new injuries to the tendon with surgical threads can.
Conservative
Prolonged immobilisation of the finger or hand with an orthopedic splint until the tendon has fully healed. This method is used in only one case: when the extensor tendon is torn at the point where it attaches to the nail phalanx.
In this type of injury, the phalanx of the toe is bent and cannot straighten itself out. A toe splint sometimes helps restore flexion and extension without surgical fusion of the tendon. However, if there is no improvement after six weeks of wearing the orthosis, the patient should be prepared for surgery.
Conservative treatment is also recommended if the patient refuses surgery (eg, for religious reasons). If the tear is incomplete, chances are that the remaining tendon will adaptively thicken over time, allowing partial restoration of motor function in the fingers.
Immobilization – a prerequisite for recovery
A finger splint is therefore always necessary after a tendon injury, regardless of the treatment method. As previously mentioned, complete immobilization with minimal muscle contraction is the most important requirement for tendon fusion, so recommendations for proper splint selection require special attention.
Treatment of a torn meniscus in the knee
First aid for painful knee injuries is to immobilize the knee (with a splint or splint) and cool the knee (with an ice pack or sports cooler). The injured person should then be taken to a trauma surgeon as soon as possible for appropriate treatment. This approach significantly reduces the risk of complications after a knee meniscus tear.
- a tear in the joint (the injury may heal with bed rest and immobilisation of the limb with a splint);
- a central tear (requires surgical treatment);
- a flap tear (the most serious injury).
The choice of treatment strategy for a knee meniscus tear also depends on which meniscus is injured. The medial (internal) meniscus has a much poorer blood supply, so its rupture requires prolonged treatment and medication (eg, intra-articular glucocorticoid injections).
After a thorough diagnosis, your doctor will decide on the best course of treatment. Conservative or Operative.. The former fights inflammation, promotes cartilage regeneration and relieves pain. The limb is immobilized or fixed with a compression brace, LP (removal of pooled blood or exudate) is done if necessary, and ice packs are applied (about 20 minutes per day).
The surgical treatment of a meniscus tear in the knee joint is carried out using arthroscopy.

Immobilization of the knee - first aid for a torn meniscus
Physiotherapy for a meniscus tear
Physiotherapy is indicated above all in the rehabilitation phase after a tear in the knee joint. It aims to strengthen the muscles of the upper and lower leg, naturally reducing the load on the knee joint and restoring full mobility of the joint. This is made possible by:
Prevention of a meniscus tear in the knee joint
So that you never have to wonder how to treat a knee meniscus tear, here are some precautions you should take:
- Make sure you warm up before any physical activity.
- Avoid deep squats, fast and twisting movements.
- Watch your weight and eat a balanced diet rich in vitamins and minerals.
- Do not neglect moderate movement to maintain the musculoskeletal system and stabilize the knee joint.
- From the age of 40 you should take prophylactic chondroprotectors, even if there are no symptoms of a meniscus tear.
DIAGNOSIS OF AXLE INJURIES
Acromioclavicular joint injuries are usually easy to diagnose. The examination of the patient begins with a careful history-taking. The physician must obtain detailed information about the mechanism of injury and previous ACL injuries. This is followed by a thorough clinical examination.
The doctor palpates the shoulder joint and performs special tests that can sometimes cause pain but are essential for an accurate diagnosis. An X-ray is taken based on the results of the clinical examination.

X-ray images can be used to exclude collarbone fractures and, in the event of a dislocation of the collarbone, the degree of displacement of the collarbone in relation to the acromion can be determined. An MRI scan can be performed if there is a suspicion of an accompanying shoulder joint injury. A large percentage of patients with ACS injuries coexist with a SLAP injury.
CONSERVATIVE TREATMENT OF ACL INJURIES
Patients with dislocated or partially injured ACL ligaments (types 1 and 2) are usually treated conservatively. Treatment in these cases aims to reduce pain and swelling. The patient is given rest, anti-inflammatory and analgesic medications, and the shoulder is fixed with an orthosis or corset. It is important to limit upper extremity loading for several weeks.

As soon as the pain subsides and the swelling subsides, the patient is prescribed exercises that first restore mobility to the shoulder joint, and then strengthen the muscles of the shoulder girdle. If the patient plays sports, he should wear shoulder protectors to avoid re-injury.
RECURRENT CRUCIAL LIGAMENT RUPTURE
_JPG.jpg)
Anterior cruciate ligament (ACL) failure, loosening, and tears occur in eight to 20 percent of all surgically repaired ACLs.
There are a number of factors that contribute to ACL graft damage and knee rupture.
If the surgery is performed correctly within six months of the injury and other ligaments are not torn at the same time, the probability of a rupture of the ACL graft is 3 to 7 percent according to the literature.
The possibility of a second tear depends on the age of the patient, the degree of rehabilitation after the operation, the type of sport played and the inherent flexibility of the ligaments of the knee joint.
The tactics of surgical treatment is determined by the correct location of the tunnels and the material of the ACL in the primary operation.
If the tunnels are not optimally (wrongly) positioned or the tape was fixed with metal screws, we perform the operation in two stages:
– First, we remove the screws from the previous operation and fill the cavities left by the screws with synthetic material.
– In the second phase, 6 months later, after the tunnels are completely closed with bone, we perform a revision operation, ie a second anterior cruciate ligament plasty.
If the tunnels were placed correctly in the first surgery, revision cruciate ligament reconstruction can be performed in one step.
By inserting a new graft in the same tunnels but with a slightly larger diameter than the previous graft.
The most common graft we use is a 12mm diameter quadriceps tendon graft, which has greater strength. It is attached to either end of the band with two absorbable fixators.
First phase of the operation
Revision plastic of the anterior cruciate ligament

1 Torn ACL graft.

2 Removal of the metal bracket (screw) holding the graft in place.

3 Status after removal of the bracket and the remnants of the torn graft.
Read more:- Torn ligament in leg how long will it take to heal.
- The long section of the big toe.
- Femoral collateral ligament.
- syndesmosis.
- Thigh tendon rupture.
- Partial tear of the ligaments of the ankle.
- Injury to the ligaments of the ankle.
- Rupture of the medial collateral ligament.
