Constant tiredness or weakness;
pallor of the skin;
rapid heartbeat;
loss of appetite and weight;
confusion and memory loss;
soreness of mouth and tongue.

- types of jumps
- cracked ribs:
- cracked ribs:
- Rittberger and Axel
- How to distinguish the Salchow
- Learn the high jump technique 'Overstep'
- Fesbury Flop High Jump Technique
- One Step Workout.
- Simultaneous one-step walking in place
- Simulation of a single step in the movement
- Learning to walk one double step at a time
- placental insufficiency
- Smoking
- Changes in fetal activity
- Determining the condition of the fetus
- Auscultation (listening)
- Ultrasound and Doppler examination
- Cardiotocography (CTG)
- When the fetus begins to move
- How the position of the fetus changes at different stages of pregnancy
- Pregnancy calendar by weeks. Pregnancy Weeks: What Happens to Your Future Baby?
- First trimester (1st day of last menstrual period – 13 weeks)
- Checklist for laboratory tests and ultrasound in pregnancy
- Symptoms of a panic attack
- Diagnosis of hypovitaminosis
- How to restore vitamin balance?
types of jumps
There are 6 types of jumps in figure skating:
cracked ribs:
cracked ribs:
Now how do you differentiate between these jumps, because it seems that athletes always jump in the same way. In reality, it looks complicated only at first glance, the following information will tell you some secrets.
The jumps differ in this, among other things. the way they are carried out.In fact, it's more important to pay attention to how a runner jumps on a particular jump.
Rittberger and Axel
For the casual skater there are only two jumps that are easy to remember - the Axel and the Rittberger.
The Rittberger jump is performed backwards, and the most important thing is that the runner runs backwards and keeps their legs crossed.


The axel, on the other hand, is performed face forward (video from a student at our school):

This is the easiest jump difference for a person who doesn't know much about figure skating. The other jumps, on the other hand, are a bit more complicated, but you can figure it out here too if you delve a little into the finer points.
How to distinguish the Salchow
A few words about the jump: The Salchow is a jump where the runner performs a backward jump on the inside edge. Of course, that doesn't mean anything to someone who just enjoys the sport, but how can you tell the difference?
If you've seen a figure skater do something similar to the video below, that's a salchow.
Learn the high jump technique 'Overstep'
It is advisable to learn the stepover in combination with the takeoff. Pay attention to the rhythm of the acceleration and make sure that the acceleration is gradual. If the jump is performed with a slower acceleration, its effectiveness is significantly reduced and leads to many errors in the later stages of the jump. The student is asked to quicken the rhythm of the final steps and take a wide stride with the foot on the heel. In the first phases, the run-up ends with the execution of the last steps either with a simple take-off without crossing the bar, or with a jump on or over low objects. Since straightness of approach is one of the most important prerequisites for the success of the vault, it should be maintained by straight-line markings on the ground or surface. It is also advisable to mark the place for the last three steps of the run-up, which will facilitate the transition to the take-off.
Numerous special and simulated exercises are used to learn the push-off:
- heel to the whole foot;
- Free leg swing with hand on support;
- Combination of resisted foot raise and free leg sweep;
- Jerk with a back swing followed by a back swing of the arms;
- The same applies to reaching for different objects with your arms, head and legs;
- Jump over the bar (elastic band) at the beginning by pulling up and bending the pushing leg.
Teach overcoming the bar in the following order.
- Teach how to carry the athlete's lunge and push leg over an obstacle. To do this, stand on the side of a low bar or resistance band (30-40 cm), lift the lunge leg, place it behind the obstacle, lift and move the pushing leg.
- The same applies to the combination of unsupported phase and arm swing.
- The same, but with a multi-tiered approach.
- Practice pushing off the bar with a short run-up (mark the place of the push-off with a circle 20-30 cm from the bar).
- Train the correct movement of the legs when pushing and pushing. Draw a landing circle in addition to the take-off circle. For a short push off, try to extend the swinging leg over the bar and lower it with an inward rotation of your foot and knee. At the same time pull up and lift the push-off leg vigorously.
- Practice correct trunk and shoulder posture during the jump. Straighten your torso and swing your arms into your elbows as you take off, bend your torso forward as you take off and push your arms down.
Fesbury Flop High Jump Technique
The advantage of this technique is better use of horizontal speed at take-off and more efficient use of height gained when jumping over the bar (Figure 22).
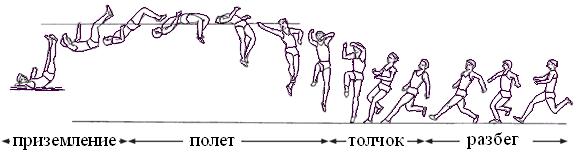
Figure 22: The Fosbury High Jump
The step starts in a straight line and then follows an arc of 3 or 5 steps at an angle of 35-38° to the bar. A 3-step arc is suitable for a slower ramp-up and a 5-step arc for a faster ramp-up. The length of the run-up is usually between 9 and 11 running steps.
During the descent it is necessary to give the body the maximum flight speed, create the optimal angle of flight and ensure an optimal position for an effective transition to the board. The take-off is performed with the leg farther from the pole, and the jumper performs an active, simultaneous movement with both hands and the swinging leg bent at the knee.
The foot position of the push-off is executed with a wide running movement on all feet at the same time (Fig. 23).
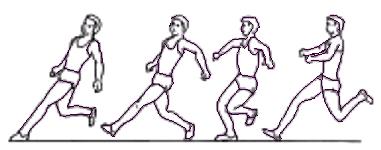
Fig. 23: Foot position in Fosbury high jump.
The lower the pressure on the 'heel kick', the faster the jump can be performed (see Fig. 24).
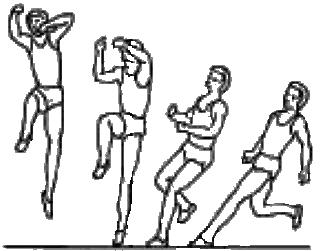
Fig. 24: Take-off phase in the Fosbury high jump
The jump over the bar takes place after the jump of the body with the back to the bar, arms stretched along the body. The performer squats with legs as low as possible and places head and shoulders behind the bar (Fig. 25).
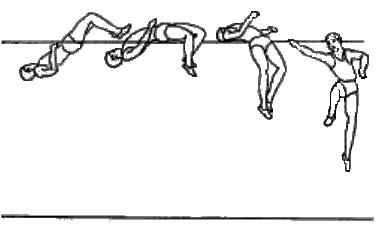
Fig. 25: High jump over the bar at 'Fosbury'.
The jumper must then push the pelvis up and lower the head and shoulders behind the bar. The head should be held with the chin pointing in. The jumper should then land on the upper back and roll backwards over the head (Photo 26).
One Step Workout.
The one-step is one of the running movements that allow you to move at high speeds - up to 8 m/s. If the conditions are suitable, you should train on level ground, otherwise on a gentle slope. Learning this jump begins with a story, demonstration, and explanation. It is also advisable to simulate the movement without bars.
The following exercises should be performed during this phase:
Simultaneous one-step walking in place
In the pp – skier stance.
1 – Without pulling your leg off the ground, pull your leg back until it is fully extended, swing while straightening your body and stretching your arms forward;
2 – Actively bend and stretch your arms backwards.
Simulation of a single step in the movement
Ip - Skier pose.
1 – Take a big step forward, place your foot on your heel and stretch your arms forward and up. Hold this position for 1 second (roll);
2 - Bring the swinging leg to the standing leg while leaning heavily forward and shoulders back - this is a two ski roll.
A quick straightening of the arms and a lunge of the legs increase the thrust of the standing leg. This is preceded by a short and quick squat.
In this movement, students make the following mistakes:
– Premature pushing off with the arms;
– Begin the cycle with a step on the same foot.
Learning to walk one double step at a time
It is not as fast as the one-step method and is therefore rarely used by experienced skiers. It is very popular with beginners, especially on tours and hikes. When explaining and demonstrating, students should pay attention to the following details of the jump:
– Abrupt erection of the upper body is not allowed, as this shortens the length of the glide;
– Poles should be brought forward in a smooth, relaxed swing motion, followed by a firm landing in the snow;
– The sticks should not be thrown up again after the push-off. To learn this jump well, you should first master all the components of the jump and also check your mastery of walking and walking in step.
You can do the following exercise:
P.—Skier's Pose.
1 – push off with your foot, bring the flying leg forward and place it on your heel;
2 – Swing the leg, straighten the knee forward, straighten the knee and place it on the heel. Stretch your arms forward while swinging evenly;
3 – abruptly bend the body forward, bringing the flying leg onto the supporting leg and withdrawing the arms;
4 - hP.
The most common mistake with this movement is short 'running steps'. This error can be corrected by moving on a lane marked with step-step markers spaced at the slide-step intervals.
Students sometimes make other mistakes as well:
– Incomplete pushing off with hands 'on the hip'. Here they should immediately put their hands behind their backs and link their arms together;
– Excessive bending of the upper body when pushing off with the hands (below the horizontal);
– Bending the legs when pushing off with the sticks.
The teacher or trainer should pay particular attention to the proper use of time to achieve the goals, taking into account each child's individual ability, age, gender and learning level. In elementary school ski lessons, it makes sense to schedule time for basketball or other sports and physical activity games at the end of the lesson, as these games bring an emotional dimension to the lesson and contribute to overall fitness.
placental insufficiency

The fetus needs both oxygen and nutrients supplied by the placenta to develop. If the body does not get enough of these two vital elements, the growth of the fetus comes to a standstill.
Placental insufficiency occurs when the placenta is not fully developed or has detached. Although the condition is rare, it carries serious risks for the baby, such as birth defects and low birth weight.
There are no obvious symptoms of placental insufficiency in pregnancy other than decreased or initially little movement of the baby.
There are now many mobile apps to help expectant mothers, including some that assess the baby's condition based on the number of movements you make. You should know that according to a study (published in Women Birth) not all apps work correctly. So first, make sure your app follows the recommendations for counting child movements - we'll write about that below.
Smoking
Smoking during pregnancy is strongly discouraged. Women who smoke during pregnancy are at higher risk of stillbirth, low birth weight and birth defects. You may have heard of these risks, but what you didn't know is that smoking also leads to decreased fetal movement.
If you smoke a cigarette, the movements of the fetus decrease in the next hour, both in strength and quantity. This is due to the increased levels of carbon monoxide and nicotine, which decrease the amount of oxygen in the blood. The baby gets less oxygen, which is comparable to having their nose and mouth partially covered.
In the first few minutes of hypoxia, the fetus may begin to move more - this is our natural reflex - and then the brain will tell it to be still and use less oxygen. The reduced oxygen levels affect the development and mobility of the fetus. If you smoke regularly, the harmful effects add up and lead to various abnormalities. It is not worth smoking even in small amounts.
Changes in fetal activity
Changes in fetal activity can be caused by external influences. For example, if a pregnant woman lies on her back for a long time, the enlarged uterus squeezes a large vessel - the inferior vena cava - and the blood supply to the fetus is cut off, which immediately triggers its rapid response - active movements. The same changes in baby's activity can also occur in any other uncomfortable position of the mother - when she leans forward, clutching her stomach, sitting with her leg over her leg, the baby's activity is forcing the mother into her posture change. The situation is similar when the baby itself presses or squeezes the loops of the umbilical cord, thus impeding the flow of blood through the umbilical cord. It then begins to move more actively, changing position and relieving stress on the umbilical cord. However, in some cases, the increased or decreased movements of the fetus can be a sign of a serious abnormality.
After 28 weeks of pregnancy, if the baby doesn't call for 3-4 hours, he may just be sleeping. In this case, the expectant mother should eat something sweet and lie on her left side for half an hour. If these simple moves don't work, it's worth repeating them again after 2-3 hours. If the baby doesn't speak up this time either, that's a reason to see a doctor. Rare and weak movements can also indicate that the fetus is not healthy, most often there is a lack of oxygen, that is, fetal hypoxia.
Determining the condition of the fetus
Your doctor will do a series of tests to determine if the fetus is fine:
Auscultation (listening)
The simplest of these examinations is auscultation (listening). The doctor listens to the baby's heartbeat using a special wooden tube (obstetric stethoscope) or a special device that picks up the baby's heartbeat. This is usually 120-160 beats per minute. A drop in heart rate below 120 or a rise above 160 indicates that the unborn child is suffering.
Ultrasound and Doppler examination
During the ultrasound examination, the doctor visually assesses the size of the fetus and whether it is developing in accordance with the gestational age, since hypoxia slows down the growth rate of the fetus, and its size lags behind the norm for the given gestational age. Also important are the structure of the placenta and the presence of signs of aging, which usually lead to impaired blood, oxygen and nutrient supply to the fetus. The ultrasound scan evaluates the amount and type of amniotic fluid, which can also change with intrauterine fetal distress. Dopplerometry of the vessels of the placenta and umbilical cord is a method of studying the speed of blood flow in these vessels. If the speed of blood flow in any of the vessels decreases, this may indicate fetal malnutrition of varying degrees of severity.

Cardiotocography (CTG)
This is an important method of assessing the condition of the fetus. A fetal CTG is performed from the 33rd week of pregnancy, since it is only at this stage of the baby's intrauterine development that the fetal circulation is fully regulated by the spinal cord and brain centers. The recording of the fetal heart sounds lasts at least 40 minutes and can be extended to an hour and a half if necessary. The device records and logs the baby's heart rate. For example, when the concentration of oxygen in the blood of the fetus decreases, the supply of oxygen to the nerve cells decreases, which in turn affects the heart rate, especially when the baby is awake. The gynecologist evaluates the curve of the heart rate recording, the episodes of shortening and rapid increase in the fetal heart rate, and from these data concludes how comfortable the baby is in the mother's womb.
When the fetus begins to move
The ultrasound examination shows that the baby is moving very early, in the 7th and 8th week. In the 16th week, the movements become more active. The baby already reacts to sounds and other stimuli. At the 17th and 18th week, the baby actively moves his hands, touches the umbilical cord, clenches and opens his fists.
The expectant mother usually notices the baby's movements by 16-20 weeks. When she is expecting a baby for the first time, she tends to notice the movements of the fetus later - in the 20th or 21st week.
Women who are pregnant again will feel the baby's movements 2-3 weeks earlier. And towards the end of the second trimester, as a rule, all expectant mothers feel the timid nudges of little feet. And from the 24th week of pregnancy, relatives can also feel the movements of the baby through the front wall of the abdomen.
It is important to understand that there is no universally accepted standard for when a woman will feel the first fetal movements during pregnancy. It depends on many factors: the thickness of the subcutaneous fat layer, the amount of amniotic fluid and the mother's individual sensitivity. Obese women, for example, notice the fetal movements later – usually in the 20th to 22nd week. In contrast, slim mothers already feel slight kicking in the 17th to 19th week.
How the position of the fetus changes at different stages of pregnancy
The first movements of the child during pregnancy are light and hardly noticeable. The mother-to-be feels them as tentative jolts, as movements inside her stomach. Some women say, 'It's like a swimming fish'. The baby grows, gains strength, and the nature of its movements changes. They become more frequent. Compared to the 20th week of pregnancy, at the 28th-32nd week the number of fetal movements triples and reaches 600 per day.
After the 30th week, the expectant mother's feelings change. The baby is already taking up all the space in your uterus. His motor activity decreases, and the woman feels only the strongest movements, sometimes she can even feel a hand or foot.
The nature of the baby's activity is an important diagnostic sign that you should inform your doctor about.
The movements of the fetus during pregnancy allow you to determine its biological rhythm, which does not always coincide with that of the mother. This is still his only way of communicating with his mother - he conveys a lot of useful information through his movements.
The position of the fetus can be determined by the location of the maximum intensity of sensation. If the mother perceives active movements of the fetus in the upper part of the abdomen, this means that the baby is in a head-down position and is actively 'kicking' its legs in the right subcostal region. On the other hand, if maximum movements are felt in the lower part of the abdomen, the fetus is in the breech position.
The closer the birth gets, the less room the baby has – and the less expansive its movements become. After 36 weeks, as the uterus descends into the pelvis, the baby's activity decreases. It doesn't stop moving, but it does so less frequently than usual. It prepares for birth - and settles into a position that's comfortable for birth.
Pregnancy calendar by weeks. Pregnancy Weeks: What Happens to Your Future Baby?
First trimester (1st day of last menstrual period – 13 weeks)
- 1-2 weeks: heavy body, severe pain in the right or left ovary, depending on where ovulation occurs.
- Week 4: Breasts begin to swell, toxicity is rare. Usually the woman does not feel anything, but changes are already taking place in the body or symptoms of premenstrual syndrome appear (enlarged breasts, a feeling of heaviness in the lower abdomen).
- The psycho-emotional state changes and the hormonal changes lead to tearfulness/exhaustion.
- The weight is usually unchanged.
- Symptoms of an ectopic pregnancy include severe abdominal pain and fever.
- 3 to 4 weeks: The placenta begins to form; the embryo develops three layers of cells. The first layer is the endoderm, which forms the epithelium of the gastrointestinal tract, respiratory system, and liver. The second layer is the mesoderm, from which the heart, muscles and connective tissues, urinary tract, genitals, and bones develop. The third layer of cells is the ectoderm, which is responsible for forming the nervous system, hair, skin, and eyes.
- 3 week: The fetal neural tube should form, which will later become the spinal cord and brain.
- 4th week: The size of the embryo is 2 mm.
- There are practically no sensations. In the 7th to 8th week, the embryo begins to swim in the amniotic fluid, an amniotic fluid sac forms, but it is only 2-3 cm long - you can hardly feel it.
- Toxicity becomes lively. The emotional state can be depressed and confused.
- The weight is lost or remains unchanged for the time being.
- Bright (scarlet) bloody discharge, severe abdominal pain, and fever are reasons to see a doctor.
- 5th week: The embryo looks like a tadpole. The heartbeat of the fetus can be seen on the ultrasound (it is clearly visible from the 6th week). The heart looks like a coiled tube.
- 6th week: The brain, inner ear, eyelids and kidneys begin to actively develop.
- 7th week: The embryo already resembles a seahorse; the legs continue to develop, the arms, which for the moment still look like flippers; the eyelids are almost formed, the complex structures of the eye are beginning to mature, the roots of the teeth.
- 8 week: The fetus is 1.5-2 cm long. The sex organs are developing (an ultrasound will not show this, but a non-invasive prenatal test (NIPT test) - a blood test that calculates the risk of chromosomal abnormalities and determines the sex of the fetus - is indicated; the heart has changed from 2 -chambered to 4-chambered hearts and resembles a smaller replica of an adult heart; the baby begins to writhe, his head, torso and limbs taking on distinct shapes.
- 9th week: The membranes disappear and become fingers and toes; the eyes on the sides begin to approach the nasal bone; the kidneys, liver and brain begin; the cardiac vessels are almost fully formed; the fetus is 3 cm long.
Checklist for laboratory tests and ultrasound in pregnancy
- Blood group, Rh factor
- Clinical blood count, serum ferritin and thyroid hormone (TSH)
- coagulation picture
- Biochemical blood test
- Determination of IgG and IgM antibodies against rubella and measles viruses
- Blood tests for HIV, hepatitis B, hepatitis C, syphilis
- Vaginal smear for flora: gonococci, trichomonads, yeast fungi
- PCR test for oncogenic human papillomavirus (HPV).
- Urine examination, microbiological examination of the urine for bacterial pathogens
- Clinical blood test, serum ferritin test
- urine test
- Urine protein (after 22 weeks at each visit)
- Clinical blood test, serum ferritin test
- Biochemical blood test
- Blood test for HIV, hepatitis B, hepatitis C, syphilis
- Vaginal smear for flora: gonococci, trichomonads, yeast fungi
- Vaginal swab for group B streptococci
- urine test
- coagulation diagram
- 1 screening test in 11-14 weeks
- 2 tests at 18-21 weeks
- Cardiotocography (CTG) from the 33rd week (every fourteen days)
- Cervical ultrasound from 15-16 to 24 weeks (one to two weeks)
Planning and preparing for your pregnancy is very important for the health of your future baby. Visit your doctor regularly, who should take care of you throughout your pregnancy. Comfortable communication with your doctor is an important part of a successful pregnancy. Learn to breathe properly and immerse yourself in what is happening to you and your baby. Knowing what to expect each trimester makes pregnancy easier. Remember that your body and your mental and emotional state will change during these nine months. You should be prepared for this, both you and your loved ones who will surround you and your baby with attention, support, love and care.
Symptoms of a panic attack
- hyperhidrosis (increased sweating);
- muscle tremors, chills;
- tachycardia;
- dystonic or physiological tremors;
- hot flashes (temporary sensations of heat);
- asphyxia (choking);
- dyspnea (shortness of breath, breathlessness, shortness of breath);
- pain radiating to left side of chest;
- nausea, desire to vomit;
- abdominal pain syndrome (abdominal pain);
- foreign body sensation, lump in throat;
- paresthesia (tingling in extremities, numbness);
- fainting, dizziness;
- Disorders of intestinal activity (constipation, diarrhea);
- dysbasia (walking disorder);
- High blood pressure;
- impairment of vision and/or hearing;
- rapid urination.
- derealization (feelings of unreality, strangeness, ambiguity of surrounding reality);
- Fear of schizophrenia, obsessive fear of going insane, loss of control over one's actions;
- disorientation, mental confusion;
- depersonalization (the patient perceives his actions as if from outside and feels that he has no control over them);
- Intermittent sleep, insomnia (insomnia), nightmares and dreams;
- thanatophobia (fear of death).
- More frequent recurrence of seizures with new symptoms;
- isolated seizures;
- occurrence of depressive symptoms (sleep disorders, loss of appetite, constantly depressed mood);
- Constant fear for one's own health;
- Refusal to perform the normal rituals of life (patients stop using transportation, stop going out, their fitness levels decline rapidly).

Diagnosis of hypovitaminosis
How to find out which vitamins are missing? This requires blood and urine tests in a medical laboratory. The test you take depends on the substance in question. B vitamin levels, for example, can be tested both ways. The vitamin D content can only be determined more precisely with a blood test. Your doctor should decode the tests. Your doctor may also order an endoscopy or colonoscopy to rule out Crohn's disease or malabsorption syndrome, which can cause vitamins not to be absorbed, even if you eat a balanced and varied diet.
– A lack of different vitamins can cause different symptoms: For example, a lack of vitamin C in combination with a lack of other vitamins leads to tiredness, dry skin and easy bruising. Don't expect a blanket answer of 'dry skin - take vitamin E, tiredness - take vitamin D'. Only research can help identify and eliminate the cause of your symptoms,' reminds Dr. mukhina.
How to restore vitamin balance?
If a vitamin deficiency is detected, the doctor prescribes drugs containing a specific vitamin, indicating the method of administration (tablets, powder, ampoules, capsules), as well as the duration of intake. If the hypovitaminosis is severe, the patient can be treated with injections. In the case of slight deficiencies, the diet should be varied and balanced. There is no need to worry about getting too many vitamins from normal food. With sensible food consumption, hypervitaminosis is unlikely to occur. However, buying vitamins, supplements and multivitamins from the pharmacy without consulting a doctor, diagnosing them 'by eye' and taking them 'just in case' is not a good idea as the doses are already higher.
During your treatment, do regular tests to check your nutrient intake under the supervision of your doctor.
- If you are deficient in several vitamins, in some cases you should take the vitamins one after the other two or three hours apart, or you can take some vitamins first and then switch to the others, otherwise you will not get any benefit from the adds Added Mariyat Mukhina.
What diseases can be caused by a vitamin deficiency in the body?
Persistent vitamin deficiencies, if not corrected in time, lead to illnesses that may be incurable. Persistent vitamin deficiency can result in:
- loss of sight;
- loss of memory;
- changes in behavior;
- breathing problems, shortness of breath;
- abnormal heart rhythm, tachycardia (rapid heartbeat);
- decreased sensitivity of the hands and feet and weakness of the fingers and toes.
Vitamin deficiencies during pregnancy can cause problems in the development of the fetus, especially in the first two months, when women are sometimes unaware that they are expecting a child.
Read more:- Breastfeeding a colicky baby.
- Child with Komarovsky clubfoot.
- Which leg is longer?.
- Which human leg is shorter?.
- The baby has short legs.
- Leg splint for newborns.
- pronator and supinator muscles.
- What the orthopedist pays attention to.
