With a small hole, the eardrum can repair itself within a few weeks. For a larger lesion, an otolaryngologist will help repair the perforation.
- Perforated eardrum. Causes, symptoms and treatment of a ruptured eardrum
- Symptoms and possible complications
- Intercostal membrane of the forearm
- Injury
- Causes of eardrum perforation
- Why SM Clinic?
- Before you go to the doctor
- Causes of eardrum injuries and main symptoms
- Causes of eardrum perforation
- Restrictions in the event of a perforated eardrum
- Perforation after perforation injury
- Perforation after middle ear infection
- Perforation after paracentesis
- Physiotherapy for eustachyitis
- How is the treatment carried out?
- Medication
- folk remedies
- Non-surgical methods for healing
- Methods for diagnosing the lesion
- Symptoms of a ruptured eardrum.
- The diagnosis.
- middle ear (auris media)
- The inner ear (auris interna)
Perforated eardrum. Causes, symptoms and treatment of a ruptured eardrum
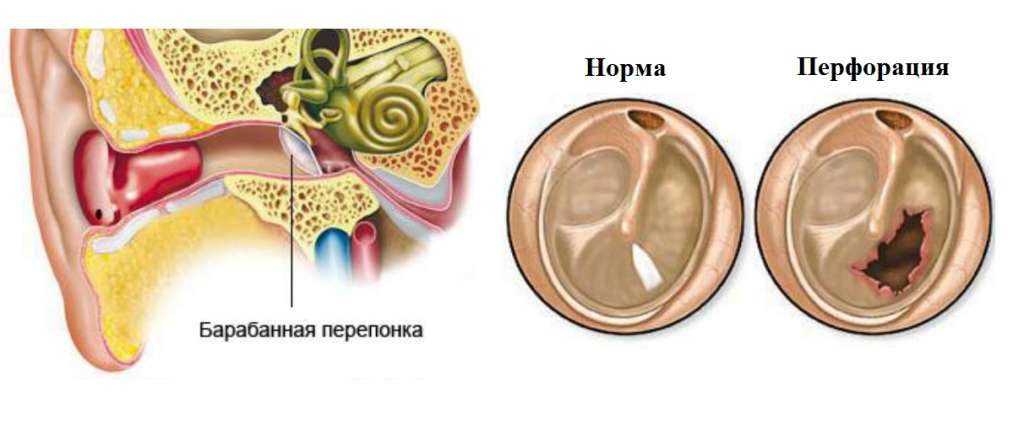
The eardrum (tympanostomy tube) – is the thin skin that separates the middle ear from the ear canal. However, its main function is not to separate parts of the ear, but to transmit sound. The eardrum is the first link in the chain of sound transmission. When it vibrates, it sends sound waves through the ossicles to the deeper parts of the hearing. The sound is not attenuated or distorted. Perforation of the eardrum is a rupture of the eardrum. This condition leads to reduced or complete hearing loss because sound waves can no longer be transmitted. In addition to hearing problems, a ruptured eardrum can also allow infection to enter the middle ear, leading to otitis media.
The most common causes of a ruptured eardrum:
- Severe sclerosis as a result of otitis media can lead to perforation of the eardrum caused by the pressure of accumulated secretions and thinning of the eardrum itself as a result of infection;
- External pressure from hitting the ear with a flat hand or other object, or pressure differences during a flight, can damage the integrity of the eardrum;
- Acoustic trauma from very loud events (e.g. an explosion);
- Direct mechanical trauma to the ear (including ear cleaning);
- Swallowing small objects in the ear.
Symptoms and possible complications
Symptoms of a ruptured eardrum:
- Severe pain in the ear;
- ringing in the ear;
- Hearing loss (partial or complete), distortion of sound;
- Sudden discharge of pus from the ear with simultaneous cessation of pain;
- bloody discharge after mechanical impact on the ear or ear canal.
A ruptured eardrum poses the risk of the following: Complications:
Intercostal membrane of the forearm
The interosseous membrane of the forearm (less often the medial or intermediate radius bone) is a fibrous lamella that connects the interosseous edges of the radius and ulna. It forms the main part of the syndesmosis of the radius-elbow joint, the fibrous connection between the two bones.
The interosseous membrane divides the forearm into an anterior and a posterior compartment, serves as an attachment point for the forearm muscles and carries the loads acting on the forearm.
The interosseous ligament serves to transfer pressure loads (such as when standing on the hand) from the distal part of the radius bone to the proximal part of the ulna. The fibers within the intercondylar network are oriented obliquely so that when force is applied, the fibers are tightened and the majority of the load is transferred to the ulna. This reduces the wear and tear associated with putting stress on a single joint. The role of the diaphysis in load transfer is illustrated by the crossing of the intercostal diaphysis; the forces acting on each bone balance each other while maintaining their natural proportions.
As the forearm moves from pronation to supination, the fibers of the interosseous membrane transition from the relaxation to the tension of the neutral position. They relax again when the forearm moves into pronation.
The interosseous membrane is composed of five ligaments:
- – Medial ligament (an important part that needs to be reconstructed in the event of an injury)
- – Additional volume
- – Distal oblique ligament (ligamentum obliquum)
- – Proximal oblique ligament
- – Anterior oblique ligament (ligamentum collaterale anterior)
Injury

The intercostal network consists of 5 ligaments: – medial ligament (most important part for reconstruction in case of injury) – accessory ligament – distal oblique bundle – proximal oblique bundle – posterior oblique accessory bundle.
Severe injuries to the forearm with separation of the radius and ulna can be caused by a tear in the intercostal mesh. The tear may result in proximal migration of the radius bone and apparent elongation of the ulna at the wrist. Rupture of the interosseous network is often associated with negative effects on the rotation of the forearm. MRI diagnosis is used for ruptures of the medial intermetatarsal membrane, but it is expensive and not widely available. In contrast, ultrasound has proven useful in the diagnosis of tibial interosseous membrane ruptures, and this technique can also be used in acute forearm interosseous membrane ruptures due to its low cost and portability.
Causes of eardrum perforation
Damage to the membrane between the outer and middle ear can result from:
- Trauma (plucking the ears with ear sticks, matches and other foreign objects, careless playing of the child with sharp objects);
- Barotrauma (flying on an airplane, sneezing with a closed nose);
- Exposure to strong, sudden noise (explosion, gunfire);
- Infections, especially acute or chronic middle ear infections (in the case of a middle ear infection, the diseased contents cannot escape because the opening of the ear canal is narrowed by the swelling; it builds up, presses on the eardrum, the purulent mass damages the sensitive membrane tissue and perforation occurs ).
Why SM Clinic?
An ear injury is a reason for an urgent consultation with an otolaryngologist.
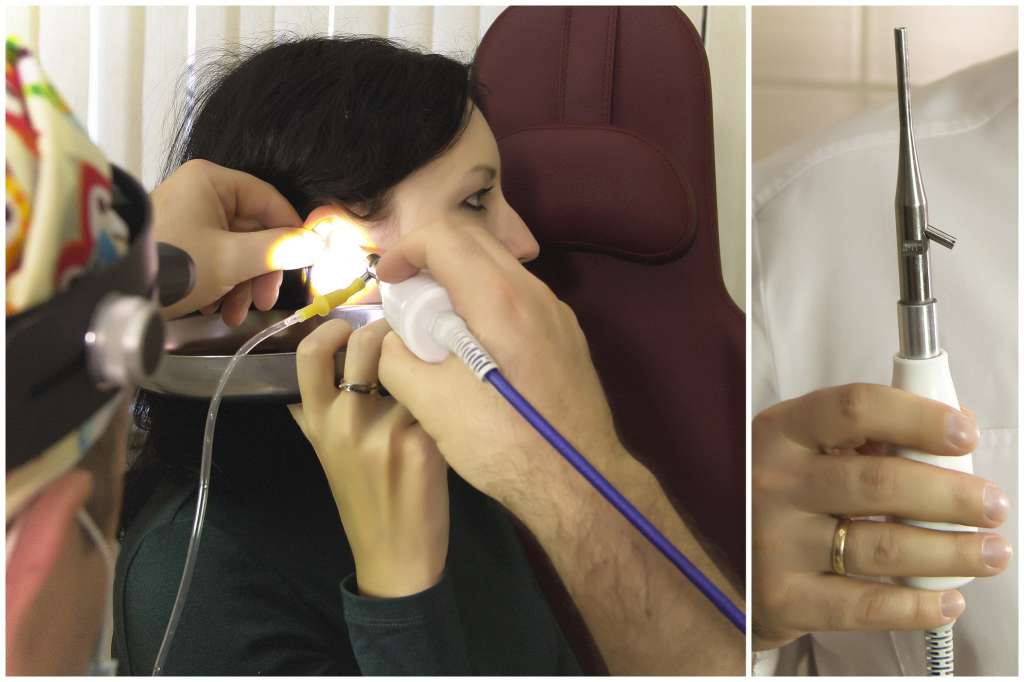
When the patient reports, the otolaryngologist explains all the symptoms and factors that precede the perforation of the ear canal. This is followed by an examination of the ear canal – otoscopy. To do this, he needs an otoscope, a small device with light optics that allows him to view the structures of the auricle and eardrum down to the smallest detail. If necessary at this stage of diagnosis, the ear can also be examined with an endoscope.
If the doctor finds pus in the ear canal, he will remove this fluid for bacteriological examination in order to identify the pathogen and initiate effective antibiotic treatment.
Before you go to the doctor
If you suspect that your eardrum may be ruptured, the symptoms are a relatively accurate indication of the injury. If you notice a deterioration in hearing quality, you should make an appointment with a specialist. You can start by visiting your family doctor, but to save time, it's worth seeing an ENT doctor straight away.
Before you see a specialist, you should think about what you want to say about your problem. To avoid forgetting anything, you should write down the most important information. It is advisable to describe in detail
- any symptoms you experience, including those that you believe are not related to an eardrum injury and do not include hearing loss, watery discharge, or other typical signs of injury;
- recent events in your life that may have resulted in damage to your ear, including infectious diseases, sports injuries, air travel
- medications, including vitamin and mineral supplements and dietary supplements you are currently taking;
- Questions to ask your doctor.
If you suspect that your eardrum has ruptured due to a middle ear infection or a blow to the eardrum, you should ask your otolaryngologist the following questions
- Has my eardrum ruptured?
- If not, what is the cause of my hearing loss and other symptoms of impairment?
- If my eardrum is damaged, what can I do to protect my ear from possible infections during its natural healing process?
- Do I need to make another appointment to check how well the tissue has healed?
- When do I need to consider special treatment?
Causes of eardrum injuries and main symptoms
The eardrum separates the outer ear from the middle ear. It consists of 3 layers: 1 from the epidermis and is an 'extension' of the skin of the external auditory canal; 2 from the fibrous membrane; 3 from the mucous membrane that lines the entire middle ear cavity. The BP can be damaged by even the slightest impact.
A perforation can have the following causes:
- Inflammation of the middle ear When pus accumulates in the eardrum cavity and puts strong pressure on the eardrum.
- For example, damage to the eardrum can be caused Damage to the eardrum can e.g. B. caused by a blow to the ear or by an object, e.g. B. a cotton swab if the ear canal is not cleaned properly.
- Sudden loud music.
- Stay near an explosion. Damage to the eardrum, which often occurs in military operations.
- Sudden changes in air pressure.E.g. when flying at high altitudes or diving.
Causes of eardrum perforation
- Ear trauma. The eardrum can rupture due to a sudden change in pressure (strong blow to the ear, kiss to the ear). It is also possible to damage the eardrum with a cotton swab by brushing too deeply and carelessly. A foreign object deep in the ear canal (a small bead or even an insect) can also damage its integrity.
- Acute purulent inflammation. With purulent inflammation in the middle ear, part of the band can be melted by the purulent secretion and its pressure on the band, which leads to perforation and the discharge of pus.
- Perforation after paracentesis or bypass. Tympanic membrane paracentesis is a procedure in which the eardrum is intentionally perforated to remove excess fluid from the tympanic cavity. It is performed in the posterior/lower quadrant of the eardrum, where the risk of damage to other ear structures is minimal. If it is necessary to maintain fluid drainage for a long period of time, a shunt (creating a stable outflow from the tympanic cavity by inserting a special tube that prevents the opening of the eardrum from closing) is used.
The symptoms of a perforated eardrum vary depending on the cause.
The injury causes severe pain in the ear, especially when trying to tilt the head in the direction in which the injury occurred. The pain gradually subsides and is replaced by a feeling of congestion, ringing in the ears and hearing loss. Bloody discharge may occur.
When the middle ear is inflamed, pus collects in it, which is also accompanied by severe pain and possibly fever. However, once the pus ruptures the eardrum and escapes, the pain subsides and the temperature returns to normal. The pus may persist for up to a week.
Restrictions in the event of a perforated eardrum
- It is strictly forbidden to moisten the ear:
- When showering, the ear should be covered with a cotton ball moistened with oil.
- When visiting swimming pools or bathing in bodies of water, the head should not be held under water and the ear should be protected with cotton wool or plugs.
- Don't go diving.
- If unsterile water enters the middle ear through the perforation, it can cause inflammation!
- Limit the use of ear drops. Many ear drops contain substances that are not intended for the middle ear. Drops with a pain-relieving effect, which many consider as first aid (e.g. Otipax), can only do harm in this case.
In most cases, the perforation will heal on its own. How long this takes depends on the size, location (perforations close to the edge of the membrane are more difficult to heal), and the body's ability to regenerate.
Perforation after perforation injury
In the case of a post-traumatic perforation, it is important to monitor the healing process to prevent infection, which can slow or stop the regeneration process.
If the perforation is very extensive (subtotal or complete, when the membrane itself has almost disappeared), the chances that the perforation will close spontaneously are low.
Perforation after middle ear infection
If the perforation occurs during otitis media, it is important to completely eliminate the acute condition, remove the pus and try to prevent recurrence.
If exacerbations occur frequently or the process has become chronic, the perforation does not close completely, begins to increase in diameter and becomes permanent (that is, it no longer heals).
Perforation after paracentesis
After a professional paracentesis, the perforation usually heals quite quickly (within a few days). The technique dictates that the procedure should be carried out in a place where nothing obstructs the closure of the hole and the hole is not too large. The perforation can persist for a long time if tissue regeneration is impaired (more common in older people) or if the procedure was not performed correctly.
Physiotherapy for eustachyitis
Physiotherapeutic treatments are essential to treat the disease:
- Air massage of the eardrum improves its elasticity, reduces tension and can normalize the mobility of the auditory ossicles.
- Laser therapy helps treat inflammation, reduce swelling, cleanse the body of toxins and reduce allergic reactions.
- UVB has an immune-stimulating, pain-relieving and regenerating effect.
- UHF therapy stimulates lymphatic and blood circulation and accelerates the function of internal organs.
How is the treatment carried out?
Choosing the right treatment is crucial and can only be done once the cause has been identified and a specialist has been consulted. Several methods are available.
Medication
If the cause of the retraction is inflammation in the ear canal, which leads to reduced permeability, drug treatment is necessary.
Vasoconstrictor nasal drops can relieve inflammation and swelling by helping to eliminate swelling in the nasopharynx and open the ear canal, ultimately reducing pressure in the ear canal. Naftizine, Rinonorm, Xylometazoline are suitable for this purpose.
If the patient develops a purulent process, topical or systemic antibiotics are prescribed. For injection into the ear, the doctor may prescribe: Normax, Otofa, Cipromed, and for oral administration: Amoxicillin, Ampicillin, Azithromycin. In some cases, injectable antibiotics such as cefazolin or netilmicin are also indicated.
Antibiotics should only be prescribed by a doctor; Self-treatment in this case can only worsen the situation and lead to the development of side effects.
If allergies are the cause of the condition, antihistamines such as Claritin, Suprastin, Loratadine, Cetrine and others can improve the condition.
In addition to drug treatment, vitamin therapy is also recommended. Choose a complex of vitamins and minerals to strengthen the immune system and speed up recovery, and supplement the diet with nutrients.
folk remedies
Traditional methods can be supplemented with folk remedies to reduce swelling. However, these should only be used with the consent of the treating doctor. The most commonly used formulas include:
Non-surgical methods for healing
Repairing a perforated eardrum without surgery is an alternative treatment and is not evidence-based medicine. Japanese researchers have suggested using a sponge soaked in a special solution to treat the defect. The size of the sponge is no more than 0.5 cm in diameter. The solution is a mixture of animal fibroblasts that produce elastin and collagen. These promote tissue growth and repair.
The sponge is inserted into the ear and fixed at the site of the ruptured membrane. By reaching the damaged tissue, the released solution promotes its regeneration. Complete healing occurs within 2-3 months. The sponge itself dissolves completely. The manipulation is always carried out on an outpatient basis. It is completely painless and does not require anesthesia.
This type of eardrum reconstruction without surgery is already actively used in various countries today. The technology was examined in a research institute. Fifty-three patients with perforations participated. The therapy led to positive results in 52 patients.
Methods for diagnosing the lesion
If symptoms appear that suggest perforation of the eardrum, the patient should consult a traumatologist or otolaryngologist. After examining the affected area, an otoscopy is performed. If membrane defects are detected, a more accurate diagnosis of the pathology is carried out. This consists of the following measures:
- stylography;
- audiometry;
- vestibulometry;
- electrocochleography;
- acoustic impedance;
- ventricular examination.
A comprehensive diagnosis enables possible damage to be assessed and therapy to be initiated. Therapy can be surgical or non-surgical.
Symptoms of a ruptured eardrum.
The symptoms of a ruptured eardrum vary slightly depending on the cause that preceded the perforation.
When the middle ear becomes inflamed, the patient feels severe pain in the ear and fever may increase. During this time, pus accumulates in the ear. However, as soon as the pus penetrates the eardrum and drains away, the pain subsides, the body temperature normalizes and the patient feels significant relief. The pus will continue to drain for a week, then the tear will heal.
If the injury is severe, the pain in the ear will gradually subside and be replaced by tinnitus, blocked ear, and hearing loss. The ear canal may bleed. In severe cases, nausea, vomiting, dizziness, temporary hearing loss, and discharge from the affected ear as well as from the eardrum and inner ear structures occur.
The diagnosis.
An ear perforation cannot be self-diagnosed. It can only be diagnosed by an ENT doctor during an ear examination. Diagnosis may include:
- Otoscopy or endoscopy – a direct examination of the ear canal to assess the condition of the membrane and the size of the perforation;
- Audiometric examination to assess the degree of hearing loss;
- Tympanometry – a method for examining the structures of the middle ear (tympanic membrane and ossicles);
- X-ray or CT scan in the case of a traumatic brain injury.
The symptoms of an ear perforation are not always clear, so if discomfort or unusual symptoms occur, an ENT doctor should be consulted immediately, otherwise the patient will have to expect unpleasant consequences. Possible complications include deafness, hearing loss, frequent otitis media, cholesteatoma formation (swelling in the ear cavity), labyrinthitis (inflammation of the inner ear), facial neuritis, and intracranial complications.
middle ear (auris media)
- Eardrum;
- Tympanic cavity with chain of auditory ossicles (tympanic region);
- ear canal (tubotympanic region);
- Mastoid process (mastoid region).
The eardrum is 0.1 mm thick, oval in shape and measures 9 x 11 mm. It consists of three layers: dermal, fibrous and mucous. The dermal layer is an extension of the skin of the external auditory canal. The fibrous layer consists of bundles of collagen fibers arranged in a circular and radial manner. The radial fibers are arranged around the central point of the membrane, the umbilicus. The radial fiber bundles extend from the umbilicus of the eardrum to its circumference, similar to the spokes of a wheel. At the periphery they merge into a fibrocartilage ring that connects the sheath to the bone. The radially arranged fiber bundles adhere closely to the malleus stalk and merge into its periosteum. The stalk of the malleus forms a protrusion on the eardrum that ends in a funnel-shaped depression - the umbilicus of the eardrum. From the contour of the malleoli, the tympanic membrane bends upward at an almost right angle, exposing a loosened portion of the tympanic membrane that lacks a fibrous layer and adheres directly to the tympanic notch of the temporal bone. The remaining 2/3 of the eardrum is a dense, vibrating surface that forms the taut part of the eardrum that is connected to the fibrocartilage ring. The mucosal layer is an extension of the middle ear mucosa.
Lines drawn along the contour of the malleus handle and perpendicular to it divide the tympanic membrane into anteroposterior, anterolateral, posterolateral, and posterior-inferior upper quadrants.
The eardrum forms the lateral wall of the tympanic cavity. The medial wall is formed by the side wall of the bony labyrinth with the protrusion of the main cochlea - the promontory. On the central wall there are two windows of the labyrinth, an oval window (vestibular window) and a round window (cochlear window), which are closed by an elastic connective tissue membrane, the so-called secondary membrane.
The inner ear (auris interna)
It is located in the temporal bone, is anatomically represented by the labyrinth and is functionally divided into different receiving apparatuses:

Morphologically, i.e. in terms of anatomical structure, a distinction is made between the bony and the membranous labyrinth. The bony labyrinth is a bony shell of considerable density, the only bony structure in the body in which the mechanism of bone remodeling does not stop. In the cochlea, the bony part is represented by the spindle and the spiral canal of the cochlea, which surrounds the spindle 2.5 times. From the spindle branches the bony spiral lamina, which, together with the primary membrane of the spiral cochlea, extends the lumen of the canal into a foramen magnum staircase, which is connected to the oval window, and together with the Reissner membrane of the cochlea divided into a tympanic staircase, which is closed by the secondary membrane of the round window (Fig. 8). The tympanic staircase and vestibular staircase are composed of a fluid called perilymph and are connected at the tip of the cochlea by the heliotrum.
The membranous part of the cochlea forms a spiral cochlea with a triangular cross section formed by the membranes mentioned: the main membrane in the lower part and the Reissner membrane in the upper part. The cochlear passage, located between the vestibular staircase and the tympanic membrane, forms a central staircase filled with endolymph. It ends with blind ends on both sides: the upper one borders the heliotremes and the lower one borders the vestibule.
On the basement membrane is the cochlear spiral organ or organ of Corti with hair receptor cells and supporting cells. Sensory spoon cells penetrate the reticular membrane that covers the spiral organ. The fibers of the ganglion cells are directed to the receptor cells of the organ of Corti, whose branches in turn form the auditory nerve and reach the cochlear nuclei in the brain stem. The hair-like receptor cells are divided into inner and outer cells. The inner cells are arranged in a single row: each is connected to an afferent fiber that transmits the stimulus to the auditory centers of the brain. These fibers account for 95 % of all afferent fibers of the auditory nerve. The external auditory cells are arranged in three rows, with a specific group of these cells being supplied by a single fiber. The afferents of the external auditory cells make up only 5 % of the fibers of the auditory nerve. The contraction of the outer cells causes the phenomenon of otoacoustic emission - signals that emanate from the inner ear (usually after sound stimulation).
Read more:- interdental membranes.
- Membrana interossea tibiae in Latin.
- Gum disease on feet.
- Earplugs to buy.
- hole in the heel.
- Child walking with clubfoot aged 2 years.
- sphenoid sinusitis.
- pain in the elbow joint.
