If you delay going to the doctor or treating yourself, you could end up with serious problems such as increased pain or further spread of inflammation.
- Heel pain: who should go to the doctor, symptoms and treatment blocks
- causes
- Clinical picture of medial and lateral neuropathy of the soleus nerve
- Clinical examination of medial and lateral soleus neuropathy
- Symptoms and signs of the disease
- diagnostic procedures
- When should you see a doctor?
- Causes of heel pain when pedaling and walking
- What can I do if my heel hurts when I walk?
- Inflammatory diseases
- How to diagnose and treat heel pain
Heel pain: who should go to the doctor, symptoms and treatment blocks
Pain in the heel is unpleasant. They hinder standing and walking, disrupt the normal rhythm of life and affect general well-being. Heel pain is rare (about one in ten musculoskeletal system patients seek help for such a problem), but can be a symptom of various rheumatological, orthopedic and neurological diseases. The most common causes are plantar fasciitis and heel spurs.
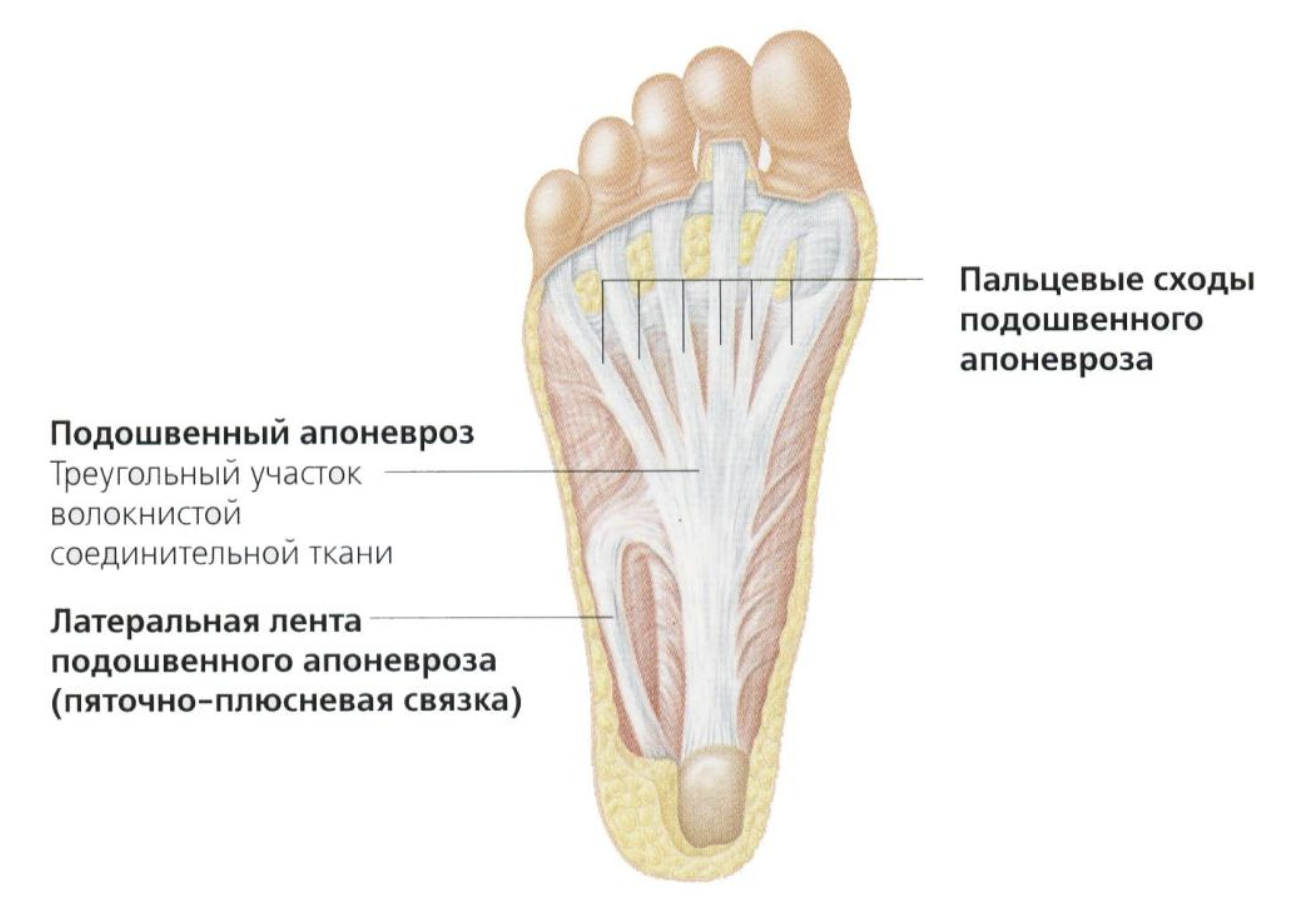
Despite its small size, the human foot is a complex structure and must support the weight of the entire body on a daily basis. It consists of 26 bones connected by joints, numerous ligaments, muscles, nerves and blood vessels. The balls of the toes are connected to the heel bone via the plantar fascia, a bundle of thick connective tissue fibers. The plantar fascia belongs to a special anatomical group, the aponeuroses (band-like, lamellar structures with a silvery-white color), which is why it is also called the plantar aponeurosis. The plantar fascia provides flexion of the foot and cushioning of the heel area during movement.
If pathological changes develop at the point where the fascia connects to the heel bone, this is called plantar fasciitis. It used to be assumed that it was an inflammatory disease (hence the ending '-it' in the name). However, modern research believes that the disease is caused by degenerative processes. Osteophytes, bony growths also known as 'heel spurs', occur as a side effect of the disease.

causes
A painful heel can be caused by
- Incorrectly chosen footwear (high heels or, conversely, flat soles);
- Excessive strain on the foot when standing, walking or running for long periods of time;
- Rapid weight gain (including pregnancy);
- Injuries such as bone fractures (including pathological ones in osteoporosis), bruises after jumping from a height, damage to the Achilles tendon, etc.;
- Inflammatory pathologies of ligaments, tendons, joint capsules (tendinitis, bursitis, etc.);
- Joint diseases (arthritis, arthrosis);
- osteochondropathies (Haglund-Schinz disease);
- neuropathies, etc.
Of the many diseases that can be associated with heel pain, plantar fasciitis and heel spurs are at the forefront.
In 9 out of 10 people, flat feet are the cause of the disease. In addition, the following factors play an important role in the development of pathology:
- Heel bone injuries (acute or chronic);
- Obesity;
- metabolic disorders (especially gout);
- circulatory disorders (obliterative arteritis, atherosclerosis, etc.);
- chronic joint and spine diseases (spondyloarthritis, psoriasis, rheumatoid and reactive arthritis) and other factors.
When the body is in an upright position, the greatest pressure is exerted on the attachment of the longitudinal fascia to the heel bone. This can lead to microtrauma. Constant microtrauma leads to inflammation and degenerative changes in the tissue. As the lesions progress, the marginal areas of the bone become hypertrophied and heel spurs form. This hypertrophy, in turn, increases inflammation caused by friction.

Clinical picture of medial and lateral neuropathy of the soleus nerve
– anamnese. The pathology of these nerves is first discovered when sensory disturbances are detected, since pain or discomfort in the foot is more often of orthopedic origin. Sensory disturbances can occur in the sole and/or heel region and sometimes occur in certain foot positions. The muscle weakness in the foot is usually not pronounced.

Clinical examination of medial and lateral soleus neuropathy
– Neurological. It should aim to detect loss of sensation in the area where the longitudinal nerves or their distal branches pass. If the lesion in the foot is asymmetrical, muscular changes such as weakness can be assessed, although usually only toe flexion can be assessed clinically.
– Generally. Careful examination of the nerve along its course in the ankle joint and attempting to elicit Tinel's sign by gently tapping along the nerve may help confirm the presence of plantar nerve neuropathy. Changes in the joint, deformity, or swelling can also help identify the location of the nerve injury.
Differential diagnosis of medial and lateral plantar nerve neuropathy. Watch for lesions of the proximal (tibial) or radial (S1) nerve, which can also cause pain and paresthesia in the foot. Changes in motor function and reflexes may help in the differential diagnosis of these lesions. Although polyneuropathies may also be included in the differential diagnosis, the bilateral nature of the lesion, depression of distal reflexes, and sensory abnormalities beyond the spread of the soleus sensory nerves may aid in the diagnosis.
Symptoms and signs of the disease
In the early stages of a foot neuroma, patients often don't notice any major changes, just mild pain when they squeeze the area between the toes.
A foot neuroma manifests itself as follows Symptoms:
- Pain and burning sensation between third and fourth toes; the photo shows where Morton's neuroma occurs most often
- a slight tingling sensation;
- discomfort when walking;
- decreased feeling in the third and fourth toe area;
- numbness in the foot;
- Pain radiating to the fingers or foot.
These symptoms of Morton's neuroma may resolve over time and may not recur for several years.
The pain only occurs when walking in high heels or wearing tight shoes, and the discomfort subsides immediately when you take them off.
The longer treatment for Morton's neuroma continues, the worse the symptoms become and the more severe the pain becomes, regardless of the footwear worn.
diagnostic procedures
The diagnosis of Morton's neuroma is made primarily on the basis of the complaints and symptoms.
Doctor in charge should take a medical historyFind out what footwear the patient wears, how often the feet are used, and whether the feet are affected by any diseases (e.g., muscle disorders, arthritis, osteoarthritis) or injuries, and then perform additional diagnostic procedures if necessary.
To confirm the diagnosis, the doctor will examine the foot and palpate the most painful areas.
If the doctor is unable to make a clear decision, he may recommend the following X-ray examination or magnetic resonance imaging (MRI). The problem with diagnosing a foot neuroma is that the symptoms are very similar to other conditions such as arthritis, fractures and osteoarthritis.
An anesthetic is administered to locate the neuroma.
When should you see a doctor?
If the pain appears for the first time, bothers you a little and then subsides, it is not necessary to consult a specialist, but you should monitor your own well-being. If the pain recurs, it is better to get examined and not postpone the visit to the clinic. Acute conditions require urgent diagnosis: when a person experiences severe pain and has difficulty walking.
In our clinic you can undergo a professional examination to determine the cause and receive comprehensive treatment. In the early stages the prognosis is often favorable.
Causes of heel pain when pedaling and walking
The heels receive a lot of wear and tear, so painful sensations in this area are not uncommon at any age. Sports injuries are the most common cause of pain in young people. In older people, pain is usually due to loss of elasticity and brittle tissue.
Heel pain after walking for a long time usually has the following causes:
- Unusual stress on the feet against the background of normal physical inactivity;
- wearing uncomfortable footwear;
- Unusual stress (e.g. walking up stairs or uphill for long periods of time).
Mild foot fatigue or mild pain after an unusually long walk is normal. You should be concerned if your heel hurts a lot, if it hurts when you walk, if it is very swollen or bruised, and if your foot is hot.
Diseases that cause pain in the heel area can be divided into several groups:
- Degenerative;
- Degenerative-dystrophic;
- Traumatic;
- inflammatory;
- systemic;
- vascular;
- dermatological.
Flat feet and other types of foot deformities can cause pain in any part of the foot, including the heel. Deformities of the spine, hips or knees can also cause problems in the feet. This is because the anatomical abnormalities incorrectly distribute the load on the body and damage the connective tissue, muscles and joints of the foot.
Injuries in the heel area can be varied: fractures and breaks, sprains, ligament and tendon tears and sprains, soft tissue bruises, skin injuries.
- Increasing swelling;
- multiple petechiae, hematomas;
- Unnatural position of the foot;
- Inability to put foot on.
What can I do if my heel hurts when I walk?
To find out why your heel hurts, hurts when walking and, most importantly, how to treat it, you should visit an orthopedist and traumatologist for a comprehensive diagnosis.
Emergency treatment is required if the pain and fever are unbearable, or if a fracture is suspected. In other cases, painkillers may be taken and a cold compress may be placed on the foot to relieve the pain. The legs should rest and only be moved with support, ideally only when absolutely necessary.
To prevent pain, you should
- Avoid cold feet;
- do sports regularly;
- control body weight;
- Choose shoes with heels 1-2 cm high;
- Pay attention to foot hygiene.
Inflammatory diseases
Various types of inflammation are one of the most common causes of painful heels. For example, inflammation of the fascia or pathology of the ligaments leads to the formation of a spur. This bony outgrowth constantly irritates the fascia during movement and worsens the inflammatory process.
In bursitis the joint capsule is affected, in periostitis the periosteum and in tendinitis the Achilles tendon. Osteochondropathy leads to sterile necrosis of the spongy substance.
In addition to pain, swelling, fever, congestion and skin ulcers are also observed in various diseases. All of this requires close attention and medical attention as quickly as possible.
The question of what to do if the heel hurts constantly is topical for many people. In addition to pain, various diseases also cause swelling, fever, hypersensitivity and skin ulcers. All this requires the attention of doctors and the rapid provision of the necessary help.
How to diagnose and treat heel pain
Since the causes of pain syndrome are very diverse, a comprehensive diagnosis is required.
First, the doctor will carefully question and examine the patient and palpate the painful area. This is followed by a series of examinations, including:
- Blood tests for tumor markers, biochemistry, white blood cell count;
- X-ray or ultrasound examination of the ankle joint;
- densitometry (bone density);
- CT examination;
- Bone scintigraphy (to detect necrosis, metastases and fistulas).
This will shed light on why heels hurt and determine the appropriate treatment, which depends on the cause and specific condition.
Non-steroidal anti-inflammatory drugs are prescribed to relieve pain. There are many different forms and names, but the doctor will decide which drug has the greatest effect on a particular patient. If the pain is very severe, corticosteroids or a block may be necessary. At home, ice can be placed on the ankle to temporarily relieve the pain. However, no matter how effective anesthesia is, it only provides temporary relief and does not treat the underlying disease. Without appropriate treatment, the person will not be 'freed' from the pathology and the heel will continue to hurt and the disease will worsen.
Surgery may be necessary to remove the spur or the affected part of the heel bone.
If conservative treatment is possible, e.g. B. in the case of inflammation or systemic diseases, uricosurics, cytostatics and chondroprotectors are prescribed. In the case of infectious diseases, a suitable antibiotic is prescribed. The need for drainage to drain purulent contents is not excluded. To eliminate the consequences of the injury, a plaster cast or orthosis is applied.
- Morton's Neuroma Ointment.
- metatarsal bones.
- median soleus nerve.
- metatarsalgia.
- Morton shoe inserts.
- is to stand on one's heels.
- If your soles and heels hurt.
- Structure of the human heel.
