This type of injury is also one of the typical injuries suffered by runners. However, in contrast to the 'runner's knee', its mechanism is slightly different. The Achilles tendon connects the calf muscle, located at the back of the shinbone, to the heel bone. It is heavily used when walking and running as it cushions the foot and coordinates the movement between the muscles.

- Foot injuries (ankle, foot, toe)
- Acute leg injuries
- Symptoms of a fracture of the heel bone
- Treatment of heel bone fractures
- Systemic diseases
- heel spur
- Injury to the heel
- heel injury
- Treatment of extra-articular fractures of the calcaneus
- Possible consequences of a bruise
- Treatment of a heel bruise
- When is a doctor's visit necessary?
- The longer you leave heel pain untreated, the harder it will be to get rid of it!
- Causes, symptoms, diagnosis and treatment of heel pain
- causes of pain
- Diagnosis of acute heel pain
- Foot and heel injuries
- Other types of muscle, joint and bone injuries
Foot injuries (ankle, foot, toe)
Almost everyone suffers from minor injuries to their toes, feet, or ankles at some point that cause pain or swelling.
Ankle, foot or toe injuries most commonly occur during sports:
In children, foot injuriesIn children, injuries to the legs, feet and ankles are most often the result of falls or sports. Toe injuries often occur in sports such as diving, soccer or basketball that require faster and sharper changes of direction. Leg injuries in children require special attention because injuries to the bones surrounding the joint can affect physical development during the child's growth period.
The risk of broken legs, ankle and foot injuries increases in older people. As a result of natural aging, bone strength weakens and muscle mass is lost. The risk of injury also increases due to loss of vision and the ability to maintain balance.
Most minor injuries to the ankle, foot, or toe are not serious and will heal on their own. Treating the injury at home can help relieve leg pain and other unpleasant symptoms until they go away.
Acute leg injuries
Acute leg injuries and trauma can result from a direct blow, a penetrating wound, or a fall, as well as from twisting, dislocation, entrapment, or abnormal flexion of the limb. The leg pain in this case can be severe and stabbing. Bruising and swelling may occur shortly after the injury. Acute leg injuries can vary greatly:
- bruises . After an ankle injury, the bruise can spread to the toes due to gravity.
- Puncture wounds. Puncture wounds on the leg can come from sharp objects - nails, buttons, knives, needles, animal teeth. A puncture wound to the leg poses an increased risk of infection because it is difficult to clean and the wound emits heat and high moisture - conditions that promote the growth of bacteria. A common possibility for infection is a foot wound where the puncture occurs through the sole of a shoe.
- Ligament injuries They support the joints;
- tendon injuries, of which rupture of the Achilles tendon is the most common;
- joint injuries, joint dislocations;
- Muscle strains. Muscles in the foot and ankle can be painful due to sprains. A severe strain can lead to a torn muscle fiber;
- Broken bones. The most common is a fracture of the toe or ankle;
- Dislocation of a boneA dislocation is a condition in which a bone moves out of its normal position in relation to other bones. This can occur in the joints of the kneecap, hip, finger, elbow, or shoulder;
- severe traumaA severe trauma resulting in compression syndrome.
Symptoms of a fracture of the heel bone
With an open fracture, the tissue is severely damaged, the wound bleeds, and sometimes bone fragments are visible. A closed fracture of the heel bone is characterized by the following symptoms:
These symptoms are also characteristic of severe bruises, so the patient may not initially notice the fracture, which can later lead to serious complications. Therefore, if the heel area is badly bruised and the symptoms described above appear, an urgent visit to the doctor and an X-ray examination is required. In some cases, a computer tomography is also carried out to clarify the diagnosis.
Treatment of heel bone fractures

First, the patient needs local anesthesia to relieve the pain. Then the doctor manually inserts the deformed bone fragments if the fracture is displaced. As soon as the initial swelling has subsided, a plaster cast is applied to the injury site up to the knee. You can walk with crutches, but you should not put any weight on your forefoot for more than four weeks. The cast is usually removed after a month and a half and allows for a rehabilitation period that should not last too long otherwise you may lose the ability to move your limbs normally.
Systemic diseases
In some cases, the heel strike is painful because there is a disease in the body. This includes:
- Epiphysitis (inflammation of the base of the heel bone). This condition can occur in both adults and children. Epiphysitis usually occurs between the ages of nine and 14 in children who are active in sports. The pain is worse when walking quickly, after running.
- Rheumatoid arthritis. This joint disease is associated with limited mobility of the joints, especially the foot.
- Ankylosing spondylitis .. One of the first symptoms of this disease is pain in the heels, which makes it difficult to stand on hard surfaces.

To eliminate painful symptoms in the heels, you need to focus on treating the underlying disease. To find out the cause, blood and urine tests should be done. If the cause is gout, the amount of acid in the urine is increased. Serological tests, x-rays and a puncture biopsy may also be helpful.

heel spur
A common cause of unbearable heel pain is heel spurs. Every year about two million people are registered with this disease. Those affected suffer from severe pain in the heel, which increases with exertion. The symptoms occur in the morning and the affected person feels pain at this time of day.
Severe heel pain leads to a specific gait in which patients lean on the outside of the foot or walk on their toes. In severe cases, patients rely on crutches or a cane.

The presence of a heel spur can be detected by an x-ray. Treatment after diagnosis is mainly conservative. Patients are advised:
Heel spurs can also be treated with physical therapy; In particular, paraffin and ozokerite applications are used.

Injury to the heel
There are 28 bones and 57 joints in the foot. broken bones in the foot Foot fractures are common and account for 10 % of all fractures. The foot can theoretically be divided into three parts: the posterior part (talus and heel bone), the middle part (scaphoid, sphenoid and cuboid bone) and the front part (metatarsal bone). In the figure, the bones of the foot, including the typical sesamoid bones, are shown in medial and lateral projection.
The foot has a big one Section normal movements, including flexion, extension, inversion and pronation. Supination, which is a combination of adduction and inversion, and pronation, which consists of adduction and pronation, are also part of normal movements. The foot contains two arches: a longitudinal arch (metatarsal) and a transverse arch (forefoot). The pressure of the body weight is usually evenly distributed between the forefoot and heel.
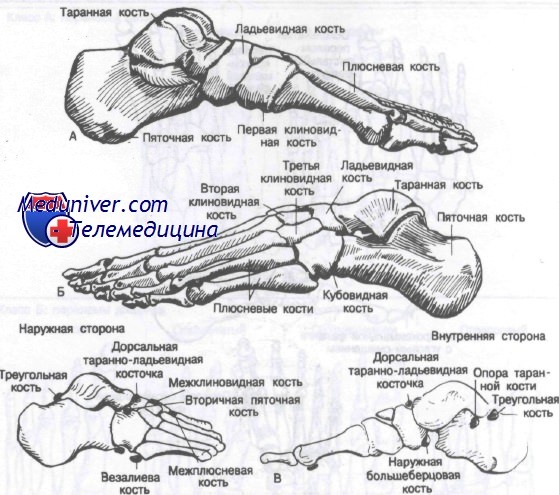
The pressure on the forefoot is distributed evenly between the forefoot and heel. The pressure on the heads of the metatarsal bones is uneven because the head of the first metatarsal is subjected to twice as much stress as the other four bones. The load on the foot is greatest during the push-off phase when walking and running.
broken bones bones of the footFractures of the foot bones generally result from three main injury mechanisms: direct trauma mechanisms, indirect trauma mechanisms, and overloads. The radiographic diagnosis of foot fractures is often complicated by the presence of secondary ossification centers and sesamoid bones. The most common sesamoid bones are the os trigonum, the os tibiale externum, the os peroineum and the os vesalcanum. They can be distinguished from a fracture by the smooth, dense outlines of the bones.
The classificationis different from the classification used in the other articles on this site. Since dislocations of the bones of the foot (except for the interphalangeal joints) are almost always associated with fractures, the authors included them in the article on fractures.
heel injury
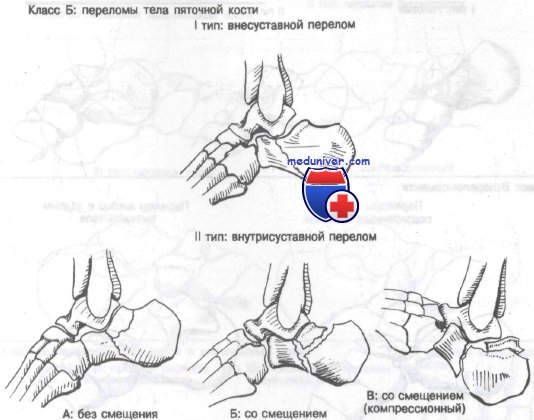
Class B: Type I extra-articular fractures of the calcaneal shaft. This fracture is atypical and does not pass through the subtalar joint. The characteristic mechanism is a fall with landing on the heel in an inversion or eversion position.
The patient complains about Painsand swelling and the inability to stand on one's foot. If the swelling on the inside or outside goes untreated for 8 hours or longer, blisters may form on the skin in that area. Pain increases with inversion, eversion, flexion or extension.
To recognize this fractureNormal projections of the heel bone are usually sufficient.
Described by fractures may be associated with entrapment of the calf nerve, in addition to any of the other complications described in the section on Class A, Type I injuries.
Treatment of extra-articular fractures of the calcaneus
Emergency treatment This includes ice packs, elevating the limb, immobilization with a thick bandage and urgent referral to a specialist. Nondisplacement fractures can be treated with immobilization, hydrotherapy, and active exercise for at least 8-12 weeks before beginning walking. These fractures are treated with a tight Jones bandage that allows weight bearing on the limb after the first 2 days.
Some orthopedic surgeons recommend a partial load of 10-20 % of the patient's weight and a 100 % load after 2 to 4 weeks of treatment. Excellent results were achieved in 75 % patients, which is comparable to most other treatments. Fractures with displacement are discussed in detail in the section on the treatment of Class B, Type II fractures. Early application of ice and elevation of the limbs are necessary to prevent blistering of the skin.
In addition to the complicationsdescribed in the section on Class A, Type I injuries, these fractures can be complicated by the formation of blisters and subsequent skin breakdown or infection.
Possible consequences of a bruise
In most cases, the bruise does not have serious consequences and the pain, bruising and swelling resolve within a few weeks. In more serious cases, complications such as nerve inflammation, periarthritis, traumatic synovitis, mobility problems, etc. may occur.
If you are concerned about a heel bruise, a medical examination can help determine the nature of the injury. Patients usually come to this decision some time after the injury when it is clear that the painful symptoms will not go away.
Treatment of a heel bruise
Many people try to treat the effects of a bruise themselves. In such cases the following steps will be taken:
- The load on the foot is minimized and the foot is protected as completely as possible;
- the leg is elevated so that the blood can drain away
- a cold compress should be placed on the bruised area;
- if it is certain that there is no break, a pressure bandage can be applied;
- After a few days, warm compresses will help dissolve the bruise.
If it becomes necessary to visit a health center, the doctor should first make a diagnosis: question and examine the patient and refer him for an X-ray.
Even if nothing serious is found, the specialist will prescribe medications and procedures that can help quickly relieve the pain and swelling. Physiotherapy (UHF, electrophoresis), for example, is very effective in such situations and requires regular visits to the health center.
As for pharmacological treatment, painkillers and various ointments are prescribed to reduce the size of the hematoma.
When is a doctor's visit necessary?
A specialist should be consulted immediately if you experience severe, acute pain in your heel while walking or if the pain does not go away or worsens over several weeks. We also recommend that you see a specialist immediately if you experience a 'fright' or morning pain. When pain is ignored and patients avoid treatment, pain symptoms usually become significantly worse and can hinder treatment and affect lifestyle.
The longer you leave heel pain untreated, the harder it will be to get rid of it!
Causes, symptoms, diagnosis and treatment of heel pain
To make a correct diagnosis and find the true cause of why your heel hurts Your doctor will need to know details about the type of pain, your medical history and your lifestyle habits, including:
- Whether the pain gets worse at certain times of the day or after certain activities.
- Your medical and orthopedic history, particularly whether you have diabetes, arthritis, or various foot injuries.
- Your age and your profession.
- Your physical activity, including sports and exercise programs.
- The type of footwear you normally wear.
- Your doctor will examine you, among other things:
- Assessment of your gait. Your doctor will ask you to walk a few steps to assess how you walk.

Neurological assessment
The type of heel pain usually depends on the specific cause.
- An inflammation of the plantar fascia usually causes severe pain at the foot of the leg when taking the first steps after getting up in the morning. This pain often disappears or lessens throughout the day, but can also occur during the day or in the evening.
- heel spurX-ray data shows that approximately 10% of the population suffers from heel spurs, with many people experiencing no pain at all. Others, however, suffer from heel spurs, which cause severe pain and increase in intensity over time.
- Inflammation of the heel spur (apophysitis) In children and adults, this condition causes pain in the back of the heel. The affected heel often feels inflamed but is not obviously swollen.
- bursitiscan cause pain in the middle and back of the heel. A characteristic feature of bursitis is that the pain increases when the foot is flexed and not when the load is increased.
- Achilles tendinitis. This condition causes pain in the back of the heel, where the Achilles tendon attaches. The pain tends to increase with movement and immobility, and the Achilles tendon swells slightly.
- A pinched nerve can cause pain, numbness, or tingling in various parts of the foot, including the heel. In addition, other symptoms often occur: swelling and discoloration if the pinched nerve was caused by a sprain, fracture, or other trauma.
causes of pain
There are several factors that can cause foot problems. Some problems are biochemical in nature and only occur during intense physical exertion. Acute heel pain is also caused by:
- plantar fasciitis.
- heel spur.
- Temporary fatigue.
- Tendon injuries.
- Reactive arthritis.
- Gout.
- Tendonitis of the heel.
It is noteworthy that patients most often complain of fasciitis. This is an inflammation or tear of the connective tissue that covers the entire surface of the foot. The pathology is accompanied by a 'needle prick in the heel'. People who are overweight or have back problems are also at risk. Poor diet and stress can also affect calcium metabolism and lead to fasciitis.
Diagnosis of acute heel pain
In order to identify the true cause of foot problems, it is important to see a doctor. He or she will perform an examination and then recommend additional laboratory or instrumental tests if necessary. This includes:
| How to diagnose | Time |
|---|---|
| X-ray of the ankle | 10 mins |
| electromyography | 300 minutes |
| Ultrasound examination of the ankle | 30 minutes |
| Clinical blood test | 10 mins |
| Magnetic resonance imaging of the ankle joint | 20 minutes |
Foot and heel injuries

Heel and foot injuries are also quite common among runners. However, in most cases they can be avoided with the right training approach. The main cause of foot and heel injuries that occur while running is the wrong footwear. This point is often overlooked, but is just as important as an individual training plan, load calculation and an obligatory warm-up before running and a 'warm-up' after running.
If you walk in shoes that are not designed for this purpose, you will put additional strain on your feet. Running in flat-soled sneakers, for example, overstretched the tendons in the foot. Running on uneven ground, uphill, on a country road, or on rocky surfaces is another risk factor for injury.
It is not uncommon for runners to develop plantar fasciitis, an inflammation of the tendons of the foot muscles. An additional risk factor is flat feet. Anyone who has this anatomical defect should consult a sports doctor before running training to determine the right training program, the right shoes and other specifics of running. Flat feet are by no means a reason to give up running, but it must be done correctly.
In addition to plantar fasciitis, other injuries specific to runner's feet and heels can also occur. For example, strain on the forefoot (if you are used to walking on your toes) can cause significant pain on the top of the foot, between the toes and sometimes even on the inner ankle.
Other types of muscle, joint and bone injuries

In addition to these three specific types of injuries to runners, other injuries can also occur in all sports. These include sprains and tears of tendons or muscles (most commonly the calf muscle, medial malleolus, or lateral malleolus), subluxations or dislocations of the knee or ankle, meniscal tears, fractures, and breaks of the bones of the lower limbs. In the event of a fall, injuries can occur anywhere else.
Pain from any sport is not uncommon. They usually subside as exercise continues. However, the athlete must pay attention to his well-being and consult a doctor in a timely manner if an injury is suspected.
Read more:- tibia and fibula.
- Fracture of the 5th metatarsal.
- The bones of the human heel.
- Dislocation of a bone in a joint.
- Fractures of the tarsal bones.
- Rupture of the radial-clavicular joint.
- Fracture of the lateral condyle.
- Bone structure of the navicular foot.
