If Achilles tendon injuries or diseases are not treated in a timely manner, there is a high risk of complications. Left untreated, Achilles tendon injuries or diseases can lead to permanent impairment of the foot.

- Anatomy and basic damage to the Achilles tendon
- The most important diseases of the Achilles tendon and their treatment
- tendonitis
- anatomy
- Caused
- Calcaneus (heel)
- Where does it hurt?
- symptoms
- diagnosis
- normal values
- X-ray: signs of illness
- Clinically Relevant Anatomy
- mechanism of injury
- symptoms
- Causes of heel pain in the morning after sleep
- causes
- Why SM Clinic?
Anatomy and basic damage to the Achilles tendon
The foot is the most important part of the lower limbs and carries most of the load. It contains the area of the Achilles tendon. He can take a lot of pressure, but is often affected by injuries and illnesses. Structure of the Achilles tendon and symptoms and treatment of tendinitis and other disorders of this ligament.
The Achilles tendon is also known as the heel tendon because it is located on the back of the heel, just above it. This area is home to the calf and calf muscles, which originate from the thigh area.
In the heel area, they unite to form the aponeurosis, which consists of elastic and collagen fibers and attaches to the heel bone. The muscle tissue connects in the heel area to form an Achilles tendon.
- Thanks to the anatomical structure of the foot, it helps maintain an upright posture when walking.
- Cushions the foot during physical activity.
- Minimizes the risk of foot injuries during normal movement.
- Allows active movement by stretching the tendons and providing stability to the foot.
- Responsible for the supination.
Although the ligament is very strong, it is often prone to injury and abnormalities. In such cases, it is important to consult a doctor in a timely manner.
The most important diseases of the Achilles tendon and their treatment
In most cases, the Achilles tendon is prone to inflammatory diseases.
tendonitis
Achilles tendonitis is an inflammatory process in the tissue.
Left untreated, it can lead to degenerative changes in the affected area.
The disease is most common in the elderly and athletes. The latter constantly subject their legs to excessive physical stress, sudden movements, jumps and other activities that lead to injuries and inflammation.
Older people develop Achilles tendonitis because of the cartilage's reduced strength and ability to stretch. Any careless movement can cause damage and provoke an inflammatory process.
There can be other causes of tendinosis.
- infectious diseases.
- Flat feet, heel spurs.
- Wearing uncomfortable shoes.
- Obstruction.
- The appearance of a bone in the foot.
Achilles tendonitis is accompanied by discomfort. In the acute form, there is pain in the affected area, which occurs only with physical activity and subsides with rest.
In the chronic form, pain in the Achilles tendon gradually increases and occurs independently of physical activity. In addition to pain, patients also complain of the following symptoms:
- reddening of the skin;
- crunching in the ankle that occurs when walking;
- thickening of the damaged tendon;
- swelling of the foot;
- restriction of mobility.
Acute and chronic Achilles tendonitis are treated conservatively. Surgical intervention is indicated only when the condition cannot be treated by other means.
anatomy
The disease, which manifests itself as exertional pain, is delimited by an examination with possible fractures or ruptures of the heel bone and tears in the connective tissue in the musculoskeletal system of the foot.
In order to make a correct diagnosis, the compact component of the synovial membrane of the foot is carefully palpated. It's essentially a muscular formation that lies between the heads of the metatarsal bones and the base of the heel bone. Their job is to shape the longitudinal arch of the foot, which allows the body to cushion as it moves.
Because there is also a transverse arch and the heel bone has a natural apex, the greatest pressure is at the point of attachment.
In traumatic situations, with overload and metabolic disorders, this leads to overgrowth of the bone on the surface of the perineal tubercle and causes pain. This is known as a 'heel spur', which looks like a sharp spike in this area on X-ray.
Caused
This distortion of natural anatomy is usually caused by degenerative changes throughout the body. Due to the disruption of internal homeostasis, 'plantar fasciitis' is most common in the elderly.
In young and middle-aged people, it can be a result of physical overload, e.g. B. through high-performance athletic training, competitions or the type of workplace with long standing or heavy lifting.
Uncomfortable, tight, high-heeled shoes, traumatic ligament damage from falls, sprains or severe bruises, and obesity can also contribute to the symptoms of the condition. In people with an intact immune system, the body is usually able to activate compensatory mechanisms itself in order to heal micro-injuries.
With age and degeneration-related changes in the metabolic processes, there is a hypertrophic reaction of the specific heel bone callus at the tip of the bone head, which leads to an excruciating pain syndrome due to the increased irritation of the nerve bundles.
Calcaneus (heel)
All iLive content is reviewed by medical experts to ensure it is as accurate and factual as possible.
We have strict rules for selecting information sources and only cite reputable websites, academic research institutes and, when possible, peer-reviewed medical studies. Please note that the numbers in brackets ([1], [2] etc.) are interactive links to such studies.
If you think any of our material is inaccurate, out of date or otherwise questionable, please highlight it and press Ctrl + Enter.
The calcaneus (heel bone) is the largest bone in the foot. It is located below the talus and protrudes significantly below it. The tuber calcanei is visible on the back of the heel bone. There are three articular surfaces on the top of the heel bone: the anterior, medial and posterior articular surfaces of the talus (faciei articulares talaris anterior, media et posterior). These surfaces correspond to the articular surfaces of the heel bone. Between the medial and posterior articular surfaces, the calcaneal sulcus can be seen, which together with the same sulcus on the talus bone, forms the sinus tarsi. The entrance to this sinus is on the dorsum of the foot on its lateral side. From the anterior superior edge of the heel bone on the medial side, a short and thick process called the talus support (sustentdculum tali) emerges. The sulcus tendinis m.peronei longi runs along the lateral surface of the heel bone. At the distal (front) end of the heel bone is the articular surface of the cuboid bone (facies articularis cuboidea), which connects to the cuboid bone.
Where does it hurt?
The iLive portal does not provide medical advice, diagnosis or treatment.
The information published on the portal is for guidance only and should not be used without consulting a specialist.
Please read the site rules and policies carefully. You can also contact us!
Copyright © 2011 – 2023 iLive. All rights reserved.
Simply click the 'Send Inquiry' button to send us information. You can also add a comment.
symptoms
The clinical symptoms depend on the location, size and extent of the growth. The first stages are painless, with occasional slight discomfort in the heel area, usually upon waking. When the patient walks, these complaints disappear.
As the exostosis increases, the pain sensations become more frequent and longer lasting. The foot begins to hurt during physical exertion and long walks. The intensity of the pain varies depending on the size of the bone and its location. Severe pain can occur when the ankle is firmly supported, e.g. B. when getting out of bed or climbing stairs.
- A tingling and warm feeling in the heel and sole in general;
- reddening of the skin on the affected area;
- roughness of the skin on the foot;
- increased pain when walking, even for short distances;
- a reduction in mobility of the foot to the point of being unable to move.

Without timely medical attention, the pain persists, and as a result, the gait changes: the patient places the foot so that the main support is on the toes or on the outside of the foot, and not on the heel. This often leads to a transverse flat foot, which aggravates the course of the disease. In advanced cases, the patient is dependent on crutches or even a wheelchair as walking becomes impossible due to the unbearable pain.
The visit lasts 60 minutes and includes diagnosis, analysis of your MRI scan and a treatment plan, both in person and online.
diagnosis
During your first visit to the orthopedist, your complaints and your medical history will be recorded. The doctor determines the duration, intensity and characteristics of the pain, as well as the type of treatment (medication, physiotherapy or massage). A heel spur is suspected when the pain with walking and exercise lasts six months or longer. The orthopaedist asks the patient about their professional activity, their sporting activities, injuries, chronic and hereditary diseases. The podiatrist examines the foot and feels it. Redness and swelling of the heel skin can be seen visually, while palpation reveals pain and localized fever. In rare cases, the pain increases when bending the big toe. This specific symptom helps to suspect a heel spur.
This is the main way to diagnose heel spurs. The bony prominences, their shape, location and size can be clearly seen on the x-ray. The orthopedist shows the patient what the heel spur looks like on the X-ray and explains its characteristics in detail. In 90 % of the cases, a spur can be seen in the center of the calcaneus tubercle on the x-ray. It is usually claw-, wedge- or splinter-shaped. It can be straight or curved. It is usually 2mm to 4mm thick when there are no symptoms and 6mm to 10mm thick when pain is present.
normal values
An X-ray can show the internal structure of the heel bone, cartilage and joints, analyze the shape and spaces and detect abnormalities - fractures, dislocations, degenerative and inflammatory changes.
An X-ray of a healthy heel will show intact, flat, and compact portions of the heel bone—the shaft and cusp—with clear contours with no bumps or patterns. An X-ray of the heel usually does not show darkening, displacement of the articular surfaces and bony growths (osteophytes, nodules) that cause an irregular contour of the heel bone. The cartilage pads are of normal thickness and the bones are not deformed.
X-ray: signs of illness
If you complain of heel pain, an X-ray diagnosis is always ordered. The pain does not necessarily have to be due to an injury, but is always an indication of a disease. The X-ray is the most common and most informative method that provides information about the condition of the bone.
A common cause of pain is plantar fasciitis, or heel spurs. The sharp, wedge-shaped growth causes severe pain that occurs when stepping on the heel, hypersensitivity, and a hard, pale spot on the skin.
The heel spur is clearly visible on a lateral x-ray as it is a bony mass. It looks like a wedge-shaped or claw-like growth on the underside of the calcaneus, usually near the center. The size of the growth is usually small, because with a spur larger than 5 mm, the patient can no longer walk due to severe pain. However, osteophytes of up to 20 mm in size can also occur. X-rays can often reveal the cause of the growth. The most common cause is a flat foot, but spurs can also be caused by trauma or a tumor.
X-rays are recommended after an injury so that a heel fracture is not overlooked. If a heel fracture is found, the location of the injury and its severity are determined.
A fresh injury is accompanied by severe pain and swelling in the heel area. X-rays are taken in two projections; the fracture lines appear as dark, uneven lines on white bone. The contours of the bone can be preserved (non-displaced fracture - fracture) or displaced from each other. There is also a displaced fracture (comminuted fracture), where the bone breaks into several small pieces. All of these species are usually clearly visible on an X-ray.
There are cases when a fracture is not visible on the X-ray, but the symptoms indicate a fracture. The angle of the belair is then determined using a lateral x-ray. We draw two straight lines. One goes through the top points of the ankle and heel joint. The other line goes through the top points of the ankle and the anterior calcaneus process. Measure the acute angle at the intersection of these lines. If the acute angle is less than 20°, a fracture is suspected and a CT scan is recommended to confirm it.
Clinically Relevant Anatomy
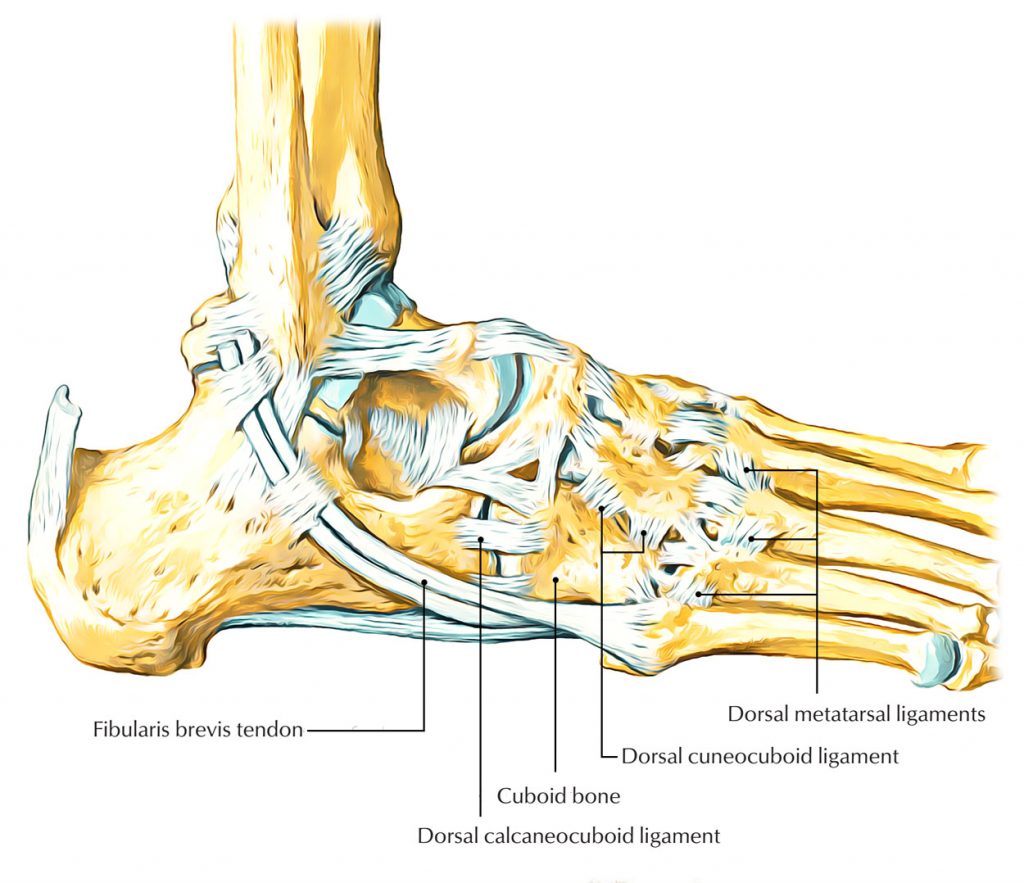
The elbow bone is a pyramidal, short, six-sided bone on the lateral side of the foot. It meets anteriorly with the 4th and 5th metatarsals, medially with the lateral talus and calcaneus, and posteriorly with the calcaneus. The function of the fetlock joint depends on the mechanics of the transverse tarsal joint, since the heel bone and the elbow bone move together when walking. The mechanics of the ankle are very diverse. The primary movement in the ankle is medial-lateral rotation about the anteroposterior axis, using the tuber of the calcaneus as the fulcrum. In inversion/reversion, the elbow bone rotates 25° about an axis running from the posterior to the antero-posterior aspect of the tarsal bone, with a movement of approximately 52° (43° to 72°) relative to the base. In addition to the inversion/inversion, this is an indication that the ankle is also stretched backwards and forwards when walking.
The ankle-foot joint is essentially unchanged in terms of the integrity of its articular surfaces and tendon attachments. When standing, the ankle and heel joints are radiologically consistent for the most part. The posterior and supportive ankle-foot ligaments and wedge-shaped fibrocartilage tendon sheaths at the calf-foot and ankle-foot joints contribute to stabilization and balance. The long fibular tendon, which wraps around the elbow bone medial and lateral to the junction with the first metatarsal and medial talar bone, also helps stabilize the ankle. The elbow bone is the pulley for the tendon of the long fibula muscle; the contraction of this muscle during the metatarsal gait cycle causes eversion of the elbow bone. Eversion of the elbow by the tendon of the long fibular muscle can facilitate load transfer to the forefoot during position changes.
mechanism of injury
Two mechanisms of injury have been proposed:
- Ankle Flexion and Inversion Injuries: Rapid foot flexion and inversion (a mechanism of transverse ankle ligament dislocation) results in a strong reflexive contraction of the long fibular muscle. The ankle acts as a fulcrum and the tendon transfers the load to the ankle, resulting in inferior medial displacement, i.e. ankle subluxation.
- Overuse syndrome: This mechanism is poorly characterized and rarely observed, but there is evidence that ankle subluxation occurs as a result of repeated microtrauma (when returning to intense activity).
- instability of the joint of the tarsal bones to each other;
- excessive weight bearing;
- inadequate or poorly designed orthotics or shoes;
- physical activity (intensity, duration, frequency);
- movement on uneven ground;
- dislocations of the foot or ankle;
- Ankle syndrome can be prevalent in patients with foot pronation due to the increased strength of the long fibula muscle arm.
symptoms
Heel pain is difficult to endure as it affects the sufferer's ability to walk properly. When walking, he tries not to step on the part of the foot that is in his way, resulting in a limp. This condition severely limits dexterity and mobility. Heel pain when walking in the morning is usually associated with plantar fasciitis. This condition can also be recognized by the following symptoms:
- Pain appears, which is strongest immediately after falling asleep and subsides after a few steps;
- The symptoms reappear during the day when we put heavy weight on the foot;
- the feet get tired quickly;
- the ankles and hocks swell.
The disease is accompanied by an excruciating pain that increases over time. Sometimes it can also spread to other parts of the foot. The following causes of this condition: obesity, uncomfortable shoes, high arches. It is quite common in people who play sports, especially running, long jumping, or high jumping. In addition, plantar fasciitis is quite common in soldiers due to the fact that they have to spend a lot of time standing.
Causes of heel pain in the morning after sleep
However, the occurrence of this symptom cannot only be triggered by plantar fasciitis. If a person has heel pain in the morning after sleeping and it is very painful to step on it, the causes may be:
- rupture of tendon;
- inflammation of the bursa (posterior bursitis);
- Gout;
- reactive or rheumatoid arthritis;
- paratendinitis;
- Osteoporosis;
- tendinitis.
People with diabetes sometimes experience severe heel pain when walking in the morning. With this disease, the symptoms are stinging and burning. In addition, the patient also develops such symptoms as peeling skin, numbness in the limbs, and the appearance of trophic ulcers. Sometimes it is this symptom that prompts people who are unaware of their diabetes to seek medical attention.
If you often have severe heel pain after sleeping, you should get checked out as soon as possible. Don't count on the problem to go away on its own or try to solve it yourself. Such measures can lead to an aggravation of the condition and encourage the development of complications.
causes
A calcaneus fracture most commonly occurs as a result of catatrauma, which is a fall from a height with the body resting on the foot. In some cases, the bone can also be damaged by an explosion. In older patients with an age-related decrease in bone mineral density, heel fractures can occur with even slight mechanical pressure, such as twisting the foot.
These injuries are called pathologic fractures (caused by osteoporosis).
Why SM Clinic?
Diagnosis is based on objective examination and an X-ray. On the x-ray, we can clearly see what a traumatic bone injury looks like, where the bone fragments are directed, and what other features the injury has.
In complex clinical cases, computed tomography (CT) can help make the diagnosis and detect reliable signs of a fracture. With this method, the images are taken layer by layer with minimal steps, allowing the doctor to determine the condition of the tissue in detail.

Severe intra-articular fractures of the heel bone can result in permanent disability or disability.
With the rarest of exceptions, it is an impact or high-energy load of the heel on the arch of the foot. fall. A wrong jump. Therefore, heel bone fractures are often combined with spinal fractures. Eventually, the power is transmitted through the lower limbs to the spine. And the greater the energy of the injury, the greater the likelihood that the spine will also be damaged.
The patient usually feels severe pain. Shortly after the injury, there is swelling and later bruising, which can also affect the finger joints and knee joints. X-rays should of course be taken. Computed tomography (CT) is performed in the following cases: in the case of insufficiently clear X-ray images, when fractures are suspected in certain areas of the heel, for precise planning of the operation (if surgical intervention is indicated).
First of all, all fractures of the heel bone are divided into intra-articular and extra-articular fractures. Surgery is more indicated for intra-articular fractures. In other cases, the prognosis for rehabilitation is worse than for extra-articular injuries. There is also a 'duckbill fracture' (this is what the heel looks like on an X-ray seen from the side with this type of fracture). In this type of fracture, the strong Achilles tendon pulls part of the calcaneus shaft up past the insertion area. As a result, the heel splits in two, and an image resembling an open duckbill appears on the x-ray. Duckbill fractures are one of the few situations in which emergency heel fracture surgery may be indicated. Because the Achilles tendon pulls and displaces the broken part of the heel so much that it presses very hard on the skin from the inside, which can lead to necrosis.
Read more:- Anatomy of the heel bone x-ray.
- heel bone injury.
- heel bone flexion angle.
- Fracture of the heel bone.
- Heel bone human anatomy photo and description.
- Displacement fracture of the heel bone.
- Fracture of the calcaneus of the foot.
- Fracture of the articular process of the heel bone.
