Women are much more prone to valgus deformities compared to men because their bodies are more influenced by hormones. The ratio of women to men is often 10:1. Women also have more flexible ligaments, which is also important in this case.
- Life without bones: why do my big toes hurt and how to remove them?
- Regular price
- What is Valgus Deformity of the Foot?
- What changes occur in the joints when a valgus deformity occurs?
- Causes of deformation of the big toe
- Treatment options for toe knots
- rehabilitation
- Complications of valgus foot deformity
- diagnosis
- symptoms
- prevention
- How to treat bumps on feet with medication?
- Physiotherapeutic methods for treating tumors on the legs
- symptoms
- causes
- Old
- Gender
- Sporting activity
- First symptoms of the disease
- Treatment methods for the big toe bone
- External use of medication
- Wearing special shoes, shoe inserts, insoles and toe protectors
Life without bones: why do my big toes hurt and how to remove them?
A crooked big toe, or stump as it is colloquially known, is not only unsightly, but also hinders walking and causes constant pain. This problem mainly affects women, but sometimes men are also affected.
You can get rid of this problem at the Diagnostični Center on V.Gribo Street in Vilnius, Lithuania.
What is a 'bunion'??
What is colloquially referred to as a big toe bunion is, scientifically speaking, a deformity of the hallux valgus or hallux valgus. When the big toe curves inward, it forms an angle with the first metatarsal bone to the other toes. There is actually no 'bump' or 'lump' - it just looks that way. If you do not address the problem immediately, the situation will worsen over time and the 'knuckles' will become more noticeable. Unfortunately, bunions are not only a cosmetic flaw and make choosing footwear difficult, but they also cause many unpleasant sensations and restrictions.
In the initial stages of bunion formation, redness and swelling occur at the base of the big toe. These symptoms do not resolve spontaneously and a visit to the doctor is necessary at this stage of the disease. Without proper treatment and prevention, the disease progresses and the patient suffers from annoying pain that is completely unbearable when walking and, in advanced cases, even at rest.
Stages of valgus formation:
- I – the thumb is displaced by 10-20 degrees, the patient has only aesthetic problems;
- II – the big toe is displaced by 20-30 degrees, the bump is painful only after long walking;
- III – the big toe is displaced by 30-50 degrees, the bump makes walking difficult and can be painful even at rest; choosing shoes is becoming increasingly difficult;
- IV - the big toe is displaced more than 50 degrees, pain and inflammation are constant and the other toes are crooked.
Regular price
Applies to patients who do not have statutory health insurance, who do not have a doctor's referral (except for radiological examinations, for which a referral is always required); if the transfer does not comply with the requirements established by legal acts; if the disease specified in the referral is not included in the list of eligible diseases; when the validity period of the transfer has expired (30 days) and in other cases established in the procedure for the provision and accounting of paid healthcare services to an individual, approved by a regulation of the Minister of Health.
Implants and materials chosen by the patient as well as individually chosen nutrition must be paid for additionally.
How is the price for the service made up?
The price for instrumental examination consists of the cost of the examination and the consumables required for the examination (contrast medium, anesthetics, scans, etc.). Please ask at reception about the price of a specific examination.
Price laboratory tests The price for a blood test consists of the examination fee (according to the price list) and the costs for the blood sample. If it is a swab, an additional fee may apply for the swab collection. Ask the receptionist about the price of a specific test.
In case of a surgical treatment Anesthesia (anesthesia), implants and materials of the patient's choice, as well as individually selected meals are charged additionally.
For dermatological services only the price for the service provided by the doctor is stated. The total price for a dermatological service consists of the costs for the procedure and the materials required for it. The price for a specific service should be inquired at reception and/or from the doctor during the consultation.
The basic price of the service is the minimum price for the service. The specific price is negotiated before the procedure during the consultation, taking into account the scope and complexity of the procedure.
What is Valgus Deformity of the Foot?
Everyone knows what such a deformation looks like - the metatarsal bone protrudes outwards and changes the position of the big toe. These changes can remain as an aesthetic defect, but can also cause osteoarthritis and severe joint pain.
The medical name for this condition is 'alus valgus' (Latin: hallux - big toe, valgus - crooked).
The deformation of the metatarsal bones occurs when flat foot worsens. The uneven load puts more pressure on the front of the foot, which leads to changes in the joint system itself.
The shape of the foot and the ligaments are inherited, so it can be said that they are 90 % hereditary. You can check with your mothers and grandmothers to see if you are prone to these bumps.
According to the statistics of the Vishnev Research Institute of Musculoskeletal Chemistry. Vishnevsky Scientific Research Center, only 30 % of all patients with a bunion on the foot are male and the remaining 70 % are female [1].
What changes occur in the joints when a valgus deformity occurs?
Poorly distributed load on the foot is the cause of bursitis. In people with this problem, the center of gravity usually shifts to the forefoot, causing a joint deformity in which the big toe and then the other toes move to the side. Podiatrists diagnose the severity of the problem by taking x-rays and determining how many degrees the big toe is displaced to the side.
This curvature leads to flattening of the sole and the formation of blisters and calluses on the protruding bone. All of these changes lead to pain and poor circulation.
People get used to flat feet, the support and cushioning functions of the foot are disrupted and the load is transferred to other joints, which can lead to pain in the knee, hip, lumbar spine and even the neck.
If you suddenly have pain in your knee or hip joints, you should see an orthopedist as soon as possible. He or she will prescribe therapeutic insoles to help balance the strain.
Causes of deformation of the big toe
The main causes of the big toe growth process are:
- mechanical damage to the foot
- Metabolic disorder or allergic reaction
- transverse flatfoot
- pathology Bone feet
- Daily effort
Stops or slows growth thickening feet Can you
- with the help of leg splints and orthoses.Stopping or slowing the growth of thickenings on the feet can be achieved with the help of leg splints, orthoses, conventional medicine and medication. It's best to take advantage of the opportunities that holistic medicine offers you. Therapies.
- Troubleshooting surgery .. If the ball begins to grow, it is important to start treatment in a timely manner, because in advanced cases the problem can only go through surgical and long term rehabilitation.
Many people do not seek help from a specialist because they believe that a growing bone does not deserve attention. However, if the joint becomes inflamed, swollen and red and the pain becomes unbearable when walking, the patient goes to one Physician. At this point, the joint is already so deformed that the problem needs to be drastically solved. The aim is surgery is restoration Bone to bring it back into the correct position, restore the function of the foot and correct the accompanying symptoms.
Stages of the operation surgery:
- distance from Salt deposits (excessive Bone)
- Fixing the thumb in its position
- Reconstruction and stabilization of the joint.
osteotomy – is the fixation of the big toe in the correct position in relation to the foot using surgical screws – the most common ones surgical the most popular treatment for valgus deformities. In some cases, limping remains lifelong after an osteotomy. Therefore, it is best not to wait for an exacerbation, but to make an appointment with one Go to an orthopedist to be arranged as soon as the first symptoms appear.
Treatment options for toe knots
For valgus deformities doctors at Doctors usually prescribe comprehensive treatment: PHYSIOTHERAPY, physiotherapyMagneto or laser therapyPhysiotherapy, magnetic or laser therapy, folk remedies (baths, decoctions, etc.), massagesointments and creams, diet.
By the way, saline solution and compresses with animal or poultry bile are effective preventative measures. However, it is unlikely that you will be able to remove an already grown bunion using 'grandma's' methods.
Many people who have ever suffered from a bunion are advised to wear special fixators and correctors, insoles and rollers, splints and orthopedic shoes. All of these tools can be purchased at a regular pharmacy or in an online store. These devices slow and sometimes even stop bone growth. However, before purchasing, a specialist should be consulted to find the most effective option for your specific case.
rehabilitation
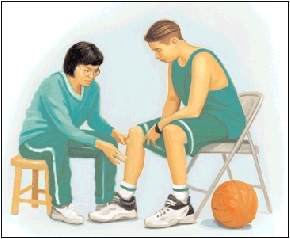
The recovery time after treatment of a valgus deformity of the first toe depends on the type of procedure. During open surgery, it is necessary to wear special shoes that do not compress the forefoot and perform special exercises. While the tissue heals, doctors recommend additional treatments: massages, physiotherapy. Once you have recovered, you can return to your normal lifestyle by limiting as much as possible the wearing of uncomfortable shoes, especially high-heeled models.
None of the folk remedies are effective. In the best case scenario, the foot stays as it is; in the worst case, burns, inflammation and other effects of uncontrolled Internet methods need to be addressed.
Once the tissue has fully healed, the limp will subside. The most important thing is that during the rehabilitation period you strictly follow all the surgeon's recommendations.
Flat valgus foot deformity. Clinical guidelines. 2016
'Traumatology and Orthopedics', eds. by NV Kornilov, GE Gryaznukhin, SP. 'Hippocrates', 2006.
Complications of valgus foot deformity
- Bursitis (inflammation of the synovial joint capsule of the foot);
- Osteoarthritis of the first toe joint (destruction of cartilage, bony hypertrophy, pain);
- deformation of other joints of the foot except the first toe;
- damage to ankles, knees, hips and spine;
- Altered gait, abnormal leg shortening and other complications.
Morton's neuroma also significantly affects the quality of life of patients. Severe pain limits the ability to play sports that require weight bearing on the leg and to lead an active life. Even simply walking becomes torture.
If the neuroma is not treated early, the progression of the disease can have serious consequences that affect the entire body.
diagnosis
Diagnosis of valgus deformity requires an examination by an orthopedist/traumatologist and a medical history. X-rays of the foot are taken in two projections. This way the extent of the disease can be determined.
If a Morton's neuroma is diagnosed, the patient must also be examined by a doctor and the painful area palpated. An ultrasound, X-ray or MRI examination may be ordered.
Additional instrumental and laboratory studies may be performed to detect concomitant pathologies and before surgical treatment.
symptoms
The first symptoms are redness and burning in the area of the first joint of the big toe. This is followed by a thickening on the inside of the foot. This is accompanied by deviation of the big toe towards the adjacent toes, causing additional pain and discomfort. The foot loses its normal shape. The bone hurts when pressure is applied as this causes inflammation in the joint.

Treatment for bunion disease usually begins in advanced cases, when the pain and discomfort are difficult to bear. In the past, surgical treatment to saw off the growth was necessary. Modern medicine is increasingly relying on non-invasive, gentle treatment methods. In the case of bones, shock wave therapy can be very helpful.
Focused high-intensity sound waves break up salt deposits, loosen bony outgrowths and fibrous areas, and increase the intensity of microcirculation in the deformed joint of the big toe. Already after the first session, the pain subsides, and a full course of treatment completely restores normal mobility of the foot and eliminates the thickening.
Due to the widespread nature of the disease, there are many folk methods for treating valgus, which, although they can provide temporary relief, in most cases only make the problem worse and keep coming back to the doctor, making his task more difficult.
Therefore, it is better not to self-medicate, but to seek the advice of a qualified specialist in due course. Bones in the feet do not disappear overnight on their own or with a few compresses; the problem must be addressed comprehensively and systematically.
prevention
Preventing foot bones includes wearing orthopedic shoes, a special diet, physical therapy for the feet and spine, and massages to strengthen the arches of the feet. Massage mats should be used to prevent flat feet. Swimming is recommended to strengthen back muscles and prevent spinal abnormalities. If you do sports that put a lot of strain on your feet, choose high-quality sports shoes.
Oleg Petrovich Tatarinov

Top-class doctor, neurologist, physiotherapist, UWT specialist, leading specialist of the Zdorovye Plus network.
medical experience more than 40 years
How to treat bumps on feet with medication?
Many patients ask themselves: 'How can you treat bumps on your toes with medication?'. As a rule, special ointments and creams are used that have anti-inflammatory, pain-relieving and distracting effects. This includes:

- Indomethacin ointment for external use;
- ValgusStop ointment based on urea, bile and salicylic acid;
- Acacia-based shark oil ointment.
All of the mentioned means are gently rubbed into the area of the protruding bone growth.
Physiotherapeutic methods for treating tumors on the legs
If a person develops a painful lump on the leg, physiotherapy treatments have a good desensitizing effect. The following have a particularly positive effect on the body:

- Magnetic therapy. It reduces pain, relieves swelling and improves blood circulation in the vessels;
- Electrophoresis with novocaine.. The treatment relieves pain and swelling, has a strong anti-inflammatory effect, improves blood circulation and restores muscle tone;
- Phonophoresis. This physiotherapeutic method is based on the use of ultrasound. It accelerates the penetration of medication into the site of inflammation. It provides pain relief and stops degenerative and dystrophic processes in cartilage tissue;
- Paraffin therapy. It reduces inflammation and relaxes muscle spasms;
- Shock wave therapy. Sound waves are specifically applied to the affected connective and bone tissue. This stretches their cell membranes, which improves blood circulation in the blood vessels and accelerates metabolic processes. The regenerative ability of the damaged joints is also improved, inflammation decreases, toxins are quickly removed from the tissue and calcifications and salts are dissolved. This leads to a gradual breakdown of bone formation in the fingers.
symptoms
The main symptoms of Osgood-Schlatter disease include:
- Pain, swelling and pain in the area of the tibial tuberosity, directly under the kneecap
- Pain in the knees that increases after exertion, especially when running, jumping and climbing stairs, and decreases at rest
- Tension in the surrounding muscles, especially the thigh muscles (quadriceps).
The pain varies from person to person. Some people only experience mild pain with certain activities, especially running or jumping. For others, the pain can be constant and debilitating. Osgood-Schlatter disease usually occurs in only one knee, but sometimes in both knees. The symptoms may last from a few weeks to several months and may recur until the child stops growing.
causes
Each long bone in a child (arm or leg) has growth areas made of cartilage at the end of the bone. Cartilage tissue is not as stable as bone tissue and is therefore more susceptible to damage, and excessive stress on the growth areas can cause swelling and pain in the area. During physical activities that involve a lot of running, jumping, and bending (football, basketball, volleyball, ballet), the child's hip muscles stretch the tendon, the quadriceps muscle, that connects the kneecap to the shinbone.
This repetitive strain can cause small tears in the tibial tendon, leading to the swelling and pain characteristic of Osgood-Schlatter disease. In some cases, the child's body tries to close this defect through bone growth, which leads to the formation of a bone lump.
The most important risk factors for the development of Osgood-Schlatter disease are age, gender and physical activity.
Old
Osgood-Schlatter disease occurs during puberty and body growth. The age range is different for boys and girls as puberty begins earlier in girls. Typically, Osgood-Schlatter disease develops in boys aged 13-14 and in girls aged 11-12. The age ranges are different for the genders, as girls reach puberty earlier than boys.
Gender
Osgood-Schlatter disease is more common in boys, but the gender difference is narrowing as more girls play sports.
Sporting activity
Osgood-Schlatter disease occurs in nearly 20 percent of adolescents who participate in sports, compared to only 5 percent of non-athletes. The disease mainly occurs in sports where there is a lot of jumping and running and the trajectory is changed. These include, for example:
First symptoms of the disease
It should be noted that the disease is very difficult to detect in the initial stages, as it has almost no symptoms. However, over time you have to deal with a serious illness.
It is more common for a person to visit a health center when the inflammatory process has already begun. The patient consults the doctor if he complains of persistent pain and swelling of the feet associated with deformities. In such cases, it is important to start treatment as soon as possible and not wait until the disease has reached a serious stage that may require surgery. In the early stages of valgus deformity, hypersensitivity and inflammation of the skin in the big toe area should also be a reason to see a podiatrist.
You don't need to wait for symptoms to determine whether you have developed a valgus deformity. To do this, simply wrap your hand around your big toe and try to pull it to the side. If there are no difficulties with the attempt, there is no problem. If the procedure is accompanied by painful sensations, the help of a specialist may be required.

The symptoms of pathology directly depend on its stage:
- The first stage is rarely accompanied by pain. More often they simply aren't there. At this stage, the big toe is displaced from the line of the foot at an angle of no more than 20°.
- The second stage is characterized by a greater displacement (angle greater than 20°). The first sensations of pain appear, but at this stage they are only mild and short-lived. The pain most often occurs when walking for long periods of time.
- The third stage is characterized by greater displacement (up to 30-50°) and severe pain, especially when putting on shoes. The mobility of the joint is impaired. Severe pain occurs when walking for a long time.
- In the fourth stage, the displacement angle exceeds 50º and severe, persistent pain occurs. The patient constantly suffers from blisters, calluses and inflammation.
- In the absence of physical activity.
Treatment methods for the big toe bone

At the first symptoms that indicate a valgus deformity, a general practitioner, orthopedist or traumatologist should be consulted. If the patient requires surgical treatment, a consultation with a surgeon or rheumatologist is required.
If the first symptoms characteristic of a valgus deformity are detected, a general practitioner, orthopedist or traumatologist should be consulted. If the patient requires surgical treatment, a surgeon or rheumatologist should be consulted.
External use of medication
Medications in the form of creams, ointments and gels are used for
- Fast pain relief;
- Cooling and warming (this effect is due to the ingredients contained in the product);
- softening of the skin;
- preventing the formation of blood clots;
- repair joint tissues;
- Prevention of bone fusions.
Products in the form of creams and ointments have a greasier consistency. They are used for massage or constant rubbing. Preparations in the form of gels are characterized by increased absorption and usually have a cooling effect.
Nonsteroidal anti-inflammatory drugs such as diclofenac gel, indomethacin ointment, or olfen gel are required to relieve pain and inflammation.
A cooling patch containing menthol or peppermint oil can be used to relieve pain.
Herbal preparations, bee or animal products can also be used.
Wearing special shoes, shoe inserts, insoles and toe protectors
Parallel to the external treatment, the alignment of the toe to the foot line should be corrected. This helps speed up the healing process. For this purpose, the podiatrist may prescribe special orthoses, supinators or shoes. These aids help maintain the correct, physiological position of the foot and leg. These aids are selected by the doctor taking into account the patient's individual circumstances.
Read more:- Anterior Tibial Syndrome.
- Legs in adolescent boys.
- shin sprain.
- Child has a bump on his foot.
- flatfoot μb.
- bones of the foot.
- Bones of the human ankle.
- Bandaging the flat foot.
