After a period of time, the nodules flatten out and form flat structures with different structures. The infiltration area can have a diameter of up to 20 centimeters. The spots are not clearly demarcated and the inflammation at the skin surface increases towards the center.
- species
- Osteogenic sarcoma of the lower leg
- symptoms and development
- Soft tissue sarcoma of the lower leg
- symptoms and development
- diagnosis
- Dark spots in both men and women
- Influence of external factors
- Forms of illness, symptoms
- diagnosis
- preparation for the intervention
- Examples of lower leg fracture treatment.
- Clinical examples of the treatment of intra-articular fractures of the tibia
- examinations and diagnostics
- What a CT scan of the lower leg shows
- CT scan of the tibia with contrast medium
- Indications for a CT scan
- CT scan of the tibia to clarify the diagnosis.
- What is liposarcoma?
- Liposarcoma – causes and types
- Diseases related to the lower leg, their symptoms and causes
- Complications of the disease, possible consequences
species
Osteogenic sarcoma of the lower leg
symptoms and development
If the tumor is diagnosed on the back of the lower leg, it may not be visible for a long time because it is covered by the calf muscle.
If the tumor is on the front of the tibia, its development and enlargement can be seen fairly easily by looking at the skin lesion overlying the tumor. It stretches and changes color.
The sarcoma can then spread from the tibia to the fibula and tibia. The tumor can destroy the tissue between the bones, leading to frequent fractures.
In the early stages, the disease does not cause pain. Only when the tumor spreads does it put pressure on nearby nerves and blood vessels, causing pain. Pain spreads to the foot and toes, swelling occurs, and trophic skin changes may appear.
Soft tissue sarcoma of the lower leg
There are two types of lower limb soft tissue sarcomas:
symptoms and development
The first type of soft tissue tumors of the lower limbs can be diagnosed at an early stage. The second type can be almost symptom-free. You may complain of throbbing or pulling pain in your lower leg.
As the disease progresses, the symptoms worsen. The most important include:
- weakness for no particular reason;
- anemia;
- Strong weight loss;
- Nausea;
- loss of appetite;
- Fever.
Then, as the sarcoma grows, it puts pressure on the blood vessels and nerves in the foot. This leads to swelling of the feet, trophic ulcers, tenderness in the toes and restricted movement.

diagnosis
Osteogenic tibial cancer is easily diagnosed on the front of the tibia. However, if it is on the back, the diagnosis is much more difficult because of the calf muscle that hides the tumor.
Superficial soft-tissue cancer of the lower leg is also much easier to diagnose than asymptomatic deep soft-tissue cancer of the lower leg.
If lower leg cancer is suspected, laboratory tests, CT scans, lower leg X-rays, and MRI scans are done.
A biopsy is taken to confirm lower leg cancer. A biopsy is then taken to determine if the shin cancer has metastasized to other organs.
Dark spots in both men and women
The causes of dark spots on the legs can be different in men and women. Dark, almost black spots with well-defined borders can indicate the development of an osteoma.

It is a pathology associated with excessive accumulation of melanin in one area of the skin, leading to hyperpigmentation.
Chloasma occurs only in women – spots can appear not only on the lower legs, but also on the breasts in the nipple area, abdomen and face.
Skin pigmentation in men can be caused by Becker's melanosis. Most often, these spots appear at a young age and look like normal liver spots. The dark spots accelerate hair growth. The exact cause of Becker's melanosis is not known.

The lesions are initially light beige to pink in color. As they progress, they take on a deep brown, almost black color. The blackening of the skin indicates the beginning of tissue necrosis. In such cases, urgent surgical intervention is required, otherwise gangrene may develop.
Influence of external factors
If a dark spot appears on the lower leg, then it can be caused by completely natural, harmless factors.
- Wearing uncomfortable, tight shoes;
- Tight, constricting clothing that causes discomfort;
- improper waxing or shaving;
- Allergic reactions to cosmetics, medicines and hygiene products;
- tanning in a sunbed;


Spots can be simple freckles and can appear at any age, in both adults and children. They do not require medication and are not a cause for concern.
The appearance of beige-brown rashes on the skin of the legs or other parts of the body as a result of hormonal 'restructuring' in the body. They do not require any special treatment and disappear spontaneously after delivery.

Forms of illness, symptoms
The clinical picture of erythema nodosum depends on its form, which can be acute or chronic.
The first symptoms of acute erythema are as follows:
- The appearance of fever;
- Fever;
- Headache;
- swelling of the legs;
- the formation of bright red nodules on the lower limbs.
At the same time, patients have enlarged inguinal lymph nodes and pain when walking or moving their legs.
After two to three weeks, the nodules will gradually disappear and change color from purplish-blue to greenish to yellowish (like a dissolving bruise).
Erythema nodosum can occur at different depths under the skin and can affect both the middle and deep layers of the dermis as well as the subcutaneous fat, and allergic vasculitis can be diagnosed. The nodules enlarge within a few hours and then usually stop growing.
The chronic form of erythema nodosum is called nodular vasculitis. This condition is more common in female patients, elderly patients, and patients with comorbidities due to recurrent chronic infections.
Aggravation of secondary epithelial erythema nodosum (recurrence of the inflammatory process) occurs in the autumn or spring months, the climatic transition period.
Dense, painful, bluish lumps the size of a walnut develop under the skin of the lower leg. The dermatological symptoms are most common on the lower legs along the main vessels, but in some cases they can also be found on the thighs. The legs are severely swollen and the patient has difficulty walking.
Characteristic of the subacute form of the disease, called Vilanova-Pignol migrans hypodermitis, is the acute onset of inflammation and the appearance of multiple solitary nodules in the subcutaneous fatty tissue of the legs.
diagnosis
When making the initial diagnosis of erythema nodosum, doctors at the Yusupov Hospital take into account the patient's complaints, his medical history and the results of the objective examination. To confirm or refute the diagnosis, a number of additional laboratory and instrumental tests are performed:
- Clinical blood test – to detect signs of an inflammatory process;
- Rheumatological blood test – to detect rheumatoid factor;
- Bacteriological examination of the nose and throat – to detect a streptococcal infection;
- tuberculin test – if tuberculosis is suspected;
- Bacteriological examination of the stool – if yersinosis is suspected;
- Biopsy of nodules with subsequent microscopic examination of the biomaterial;
- rhinoscopy and pharyngoscopy for chronic infections;
- X-ray of the chest;
- CT examination of the chest;
- Ultrasound of the veins and revascularization of the lower limbs to determine the patency and the severity of the inflammation;
- Consultation with related specialists – infectious diseases specialists, otolaryngologists, pulmonologists, phlebologists, etc.
The diagnostic scheme is selected individually for each patient by the highly qualified specialists of the Yusupov Hospital, taking into account the clinical picture of the disease and other important data.

preparation for the intervention
No special preparatory measures are required for the patient. It is enough to tell the doctor before the visit if there are any metal objects in the area of the lower leg, such as B. Support pins. And all moving metal objects must be removed so that they do not distort the later result.
A single scan is usually not enough for a full investigation. In this case, the doctors ask for an image in several different projections, varying the posture of the injured person. The key to a good result is to keep the subject completely still, which is not difficult to do with only a few seconds of direct imaging.
For added safety, the radiographer may be asked for a lead apron to protect other parts of the body from unnecessary radiation. This protection is of particular importance for the person to be examined:
The issued apron serves to reliably shield the fetus from increased exposure to radiation, which is acceptable only for adults.
To get a reliable result, the patient is placed on the doctor's couch. If a straight projection is required, he is asked to turn on his back. If lateral projection is required, the subject turns toward the affected lower limb so that the sound leg does not obstruct the view. To do this, the leg is bent at the knee and hip joints.
The X-ray technician can help you position yourself correctly, give you a lead shield and tell you when the results can be taken.
More current and relevant health information on our Telegram channel. Subscribe: https://t.me/foodandhealthru
Specialties: General Practitioner, Radiologist, Nutritionist .
Place of work: LLC 'SL Medical Group' Maikop .
Education: 1990-1996, North Ossetia State Medical Academy.
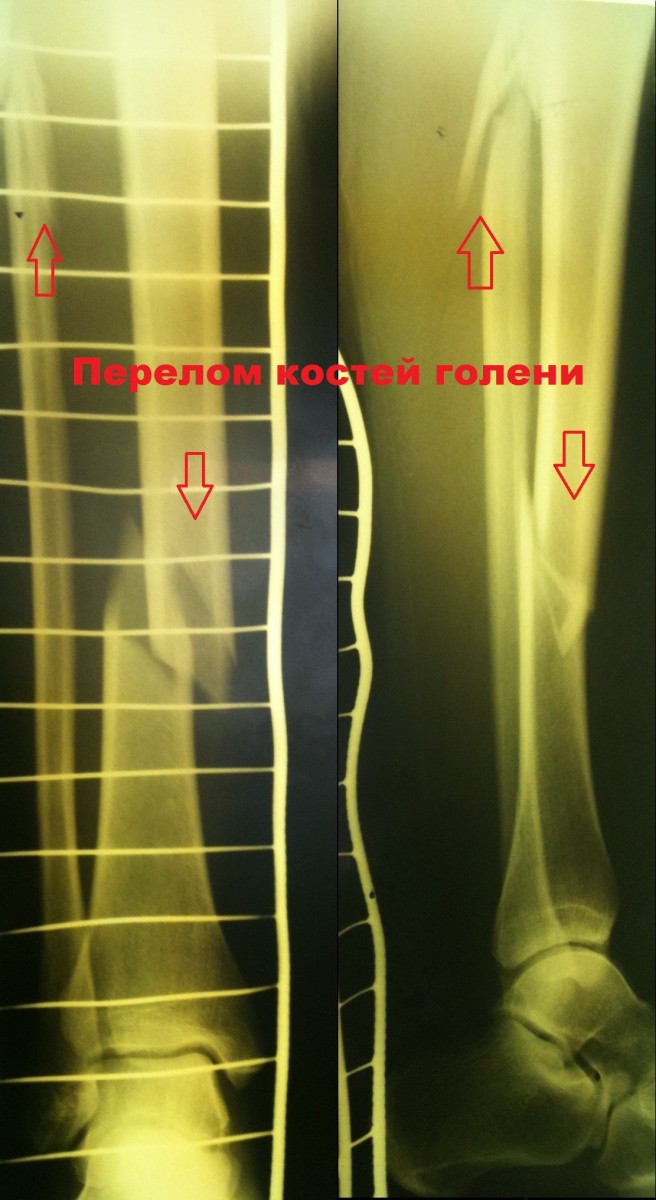
Examples of lower leg fracture treatment.
Patient R., 41 years: injury from a fall while skating. He was admitted to the hospital admissions ward.
On examination, 4 hours after admission, he was treated with Metal osteosynthesis with locking pin.
The postoperative course was unremarkable. The patient was mobilized and discharged from the hospital on day 5.
Patient C. 50 years old. Injured in a car accident (passenger). Diagnosed with. Fragmentary fracture of the tibia..
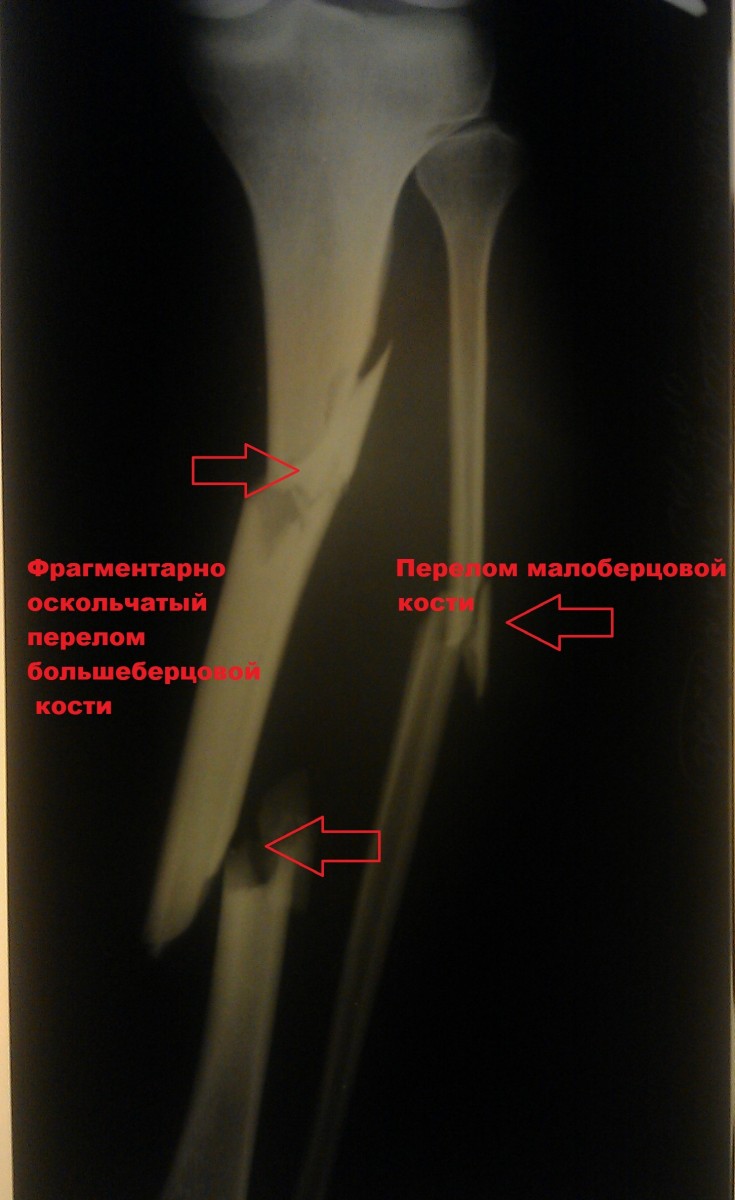
A closed reduction was performed Osteosynthesis of the tibia with locking bar.

Patient K., 42 years. The patient was injured in a traffic accident (pedestrian). The diagnosis is. Isolated fracture of the tibia..

A was performed. Surgery to immobilize the fracture..

Clinical examples of the treatment of intra-articular fractures of the tibia
Patient L. 37 years old. Injury resulting from a traffic accident.. Surgical treatment was performed.

At the follow-up examinations, the location of the fractures was satisfactory. The wounds healed with primary tension, the sutures were removed on the 14th day.

Patient M., 35 years old. The injury was caused by a fall on the street..
A closed reduction of the fracture was performed with a special device. In the second phase, the fracture was fixed with a plate and screws through minimal incisions. Importantly, the fracture site itself was not opened, ie the blood supply and soft tissue relationship were not compromised. The incidence of postoperative complications is extremely low with this surgical technique.
examinations and diagnostics
When diagnosing phlegm, ultrasound is used. Differential diagnosis is carried out at keratitis, deep arterial thrombosis/venous vessels, osteitis.
How should phlegm be treated? Regardless of the localization of the pathological process, bed rest is indicated for the patient. In the serous-infiltrative stage: conservative treatment with antimicrobial drugs.
Topically: semi-alcoholic poultices with a solution of dimexide solutionBandages on the affected area with ointment Levomecol. In cases of severe poisoning, detoxification therapy is carried out. If necessary, immunomodulating drugs, vitamins, general tonics and symptomatic treatment are administered.
If the mucus is confined to an extremity (foot, hand, hip, lower leg, etc.), immobilization of the extremity is indicated. If the process becomes purulent and necrotic, it is indicated to open the mucus under general anesthesia and empty the cellular spaces.
What a CT scan of the lower leg shows
Computed tomography of the lower extremity includes examination of the fibula, tibia, ligaments, muscles, and ankle. An additional examination is required to analyze the condition of the knee joint, since the articular surfaces are not always visible with this procedure.
Computed tomography provides clear information about the condition of the compact tissue and is therefore used in the diagnosis of pathological changes in cartilage and bones. With the CT scanner, the doctor receives slices in layers that show the condition of the bones and cartilage in detail. Using a 3D model of the tibia, the structure and homogeneity of the dense elements are analyzed.
- The presence of cracks and fractures in the shin;
- areas with destructive changes;
- foci of bone sclerosis;
- tumors;
- the condition of the periosteum and the connection to the surrounding soft tissues;
- Degree of mineralization and density of bone and cartilage.
CT scan of the tibia with contrast medium
In order to detect pathological changes in the soft tissues of the lower leg and the blood vessels, the doctor orders a CT scan with a contrast medium. For this purpose, the patient is injected with an iodine-containing substance using the native method, which provides a radioactive contrast and makes the vascular network and soft tissues clearly visible. The examination is then repeated.
The preparation has practically no pathological effects on the human body and is completely broken down 1-2 days after the procedure. Contraindications for contrast-enhanced CT are:
Contrast-enhanced CT helps diagnose tumors and destructive lesions in the lower leg bones, and the images are clearer and more meaningful. However, an MRI examination is more suitable for examining the soft tissue in layers.
Indications for a CT scan
There are a number of indications for which a specialist doctor recommends additional examination. A CT scan of the bones of the lower limbs is recommended in the following cases:
CT scan of the tibia to clarify the diagnosis.
In some cases, a CT scan of the tibia is crucial for the differential diagnosis. A CT scan is indicated to clarify the following diagnoses:
- Breaks and fractures of the fibula and tibia;
- ankle dislocations and subluxations;
- Ligament injuries (sprains, strains);
- Inflammatory and dystrophic changes in bone structure (osteomyelitis, osteoporosis);
- arthritis and osteoarthritis of the ankle;
- Cysts, benign and malignant tumors.
The CT scan of the tibia is used to check the bone fracture, to assess the reduction of the bone fragments and the condition of the fracture line.
This procedure is recommended when the results of other investigations can be clarified. With the classic X-ray examination, the result depends on the right angle, otherwise it is difficult to read the image and make a clear judgment. If the analysis of the x-ray is difficult or there are doubts about the diagnosis, the doctor prescribes a CT scan of the lower leg. This method, thanks to the fact that the images are taken in different projections, provides more accurate information and allows differential diagnosis of the pathology of the bone tissue.
What is liposarcoma?
Liposarcoma is a neoplasm of soft tissue. Liposarcomas account for about 20 % of all soft tissue sarcomas occurring in adults.
The lesion can develop at different ages. A liposarcoma in childhood is very rare, but possible. Most often, this type of cancer occurs in people aged 50-60 years.
Both men and women can get liposarcoma, but women are more likely to be affected.
Liposarcoma – causes and types
A liposarcoma occurs when certain mutations cause uncontrolled growth of fat cells. However, the exact causes of this type of genetic disease have not yet been elucidated.
- Localized sarcoma. The most common type of tumor is the well-differentiated liposarcoma, which is characterized by local malignancy. This means that the tumor can invade nearby healthy tissues, but generally has little tendency to metastasize distantly. Among its most distinctive features is the fact that it is very prone to relapse.
- mucosal liposarcoma. Another type is mucosal liposarcoma, which is associated with round cell liposarcoma tumors. This soft tissue sarcoma, on the other hand, is known to frequently lead to distant metastases.
In addition, the liposarcoma multiforma, also called polymorphic liposarcoma, is differentiated. This is a fairly rare type of sarcoma known to form large metastases. And the liposarcoma is indeterminate, since it has characteristics of all the previously mentioned types of liposarcoma.
Diseases related to the lower leg, their symptoms and causes
The human lower leg (photos are included in the article for illustration) consists of bones, blood vessels, muscles and connective tissue. They are important for movement and standing. A leg injury can occur during sports, running, a fall or an accident. The most common injuries include sprains, dislocated joints and broken bones. These can affect the whole leg or just the foot, ankle, knee or hip.
Some medical conditions can also lead to foot problems. For example, osteoarthritis of the knee, which is common in older people, can cause pain and limit movement. Vein problems lead to varicose veins or deep vein thrombosis. 

Clumsy foot landing after a fall.
Direct trauma to the front or inside of the shin or ankle.
Inability to walk and pain when walking.
The patient can no longer bear weight on the leg.
Medical treatment can help with broken bones, leg cramps, blood clots, or nerve problems. In other cases, wraps, foot braces, and wearing appropriate footwear are recommended.
Complications of the disease, possible consequences
The most common complications occur after injuries or broken bones:
- Pain in your knees or ankles.
- Infection of the bone (osteomyelitis).
- Damage to a nerve or blood vessel.
- Compartment syndrome or neuromuscular disease.
- Arthritis in the joints.
- Unequal leg length. A child's long bones grow at the ends of the bones in softer areas called growth plates. When a fracture goes through a growth plate, that limb may be shorter or longer than the other.
Deep vein thrombosis can lead to a serious condition called pulmonary embolism, when a blood clot breaks off and travels to the lungs.
The legs are the backbone of the entire body; humans use them for active movement. In order to be able to withstand great loads and be more resistant to injuries, lower legs and ankles must be trained. The images show the main muscles that keep the body in shape and enable walking.
Read more:- Description of the human foot bone.
- Outer malleolus of the right tibia.
- foot pattern.
- Ankle strap at heel.
- Anterior shin muscle (tibialis anterior).
- Anterior fibula ligament tear in the ankle.
- Root nodules in children.
- Photo of a teenager's leg.