Important: Regardless of the type of fracture, it must be treated in the hospital by doctors, since the success and avoidance of complications depend on the timing of treatment, the competence of the doctor and the correct treatment.

- Treatment of a fracture of the humerus bone
- Anatomy of the elbow joint.
- The symptoms are characteristic of the injury
- Treatment
- Diagnosis of a fracture of the humeral head
- Complications of fractures of the lateral humeral condyle
- causes of injuries
- How do you diagnose a femoral condyle fracture?
- diagnosis of pathology
- What are the characteristics of femoral condyle fractures?
- diagnosis
- ICD-10
- causes
- diagnosis
- Treatment of a fracture of the tibial condyle
- Conservative treatment
- surgical treatment
- Fracture of the tibial condyle
- Treatment
Treatment of a fracture of the humerus bone
A fracture of the elbow joint is not a medical term, rather it can be a sprain or torn ligament, and the bones that make up the joint are, in the case of the elbow joint, the lower end of the humerus or the upper ends of the radius and ulna.
In this article we will consider one of the most serious fractures in this anatomical area - a fracture of the lower third of the humerus, its condyles, which are involved in the formation of the elbow joint.
Fractures of the lower third of the humerus, which are involved in the formation of the elbow joint, or fractures of the humeral condyles are a serious injury that requires a considered surgical approach and is characterized by a difficult rehabilitation period and often unsatisfactory treatment results.
Fractures of the distal humerus are extremely serious, often extending to the articular surface and consisting of many small fragments. In the vast majority of cases, surgical treatment is required, otherwise there is a high risk of non-union, false joint, malalignment, post-traumatic arthritis and contractures of the elbow joint.
Anatomy of the elbow joint.
The elbow joint consists of 3 bones: the humerus, the radius and the ulna. Flexion and extension of the elbow joint is achieved by the movement of the ulna around the humerus. The head of the radius bone also rotates in the elbow joint, and the radius itself crosses the elbow and the forearm rotates.
The elbow joint itself is formed by the lower end of the humerus and the upper ends of the ulna and radius.

The elbow joint is held in its physiological position by the architecture of the partial bones, the joint capsule, which surrounds the ends of the joint like a sack, and numerous ligaments. Fractures of the lower end of the humerus involving the joint capsule are characterized by a large number of small fragments.
These fractures are called amputation fractures or multifragment fractures. In most cases these fragments are displaced relative to each other.
The symptoms are characteristic of the injury
Symptoms appear almost immediately after the fracture and help determine the nature and complexity of the injury:
- Presence of a characteristic pain syndrome limited to the joint and hip;
- Instability, excessive mobility of the kneecap;
- A feeling of instability, a wobble in the knee;
- When palpated, pressure on the fractured condyle of the knee joint causes severe, stabbing pain
- Restriction of movement and severe pain in the joint;
- Crunching or crepitus on palpation caused by displaced bone fragments;
- There is swelling and swelling in the knee area, as well as an effusion in the joint cavity, which flattens the joint contour.
Often, patients can move independently despite a fracture and do not immediately seek medical attention because the knee does not hurt after the injury or fracture.
Important: If a fracture is suspected and there are symptoms that precede the injury, it is important to seek medical attention immediately as sometimes pain is not present. Failure to seek medical attention in a timely manner may require surgical intervention, which can be avoided if the fracture is recent.
Based on the external examination and the X-ray findings in the appropriate projections, the doctor will determine the severity of the fracture and further treatment.
Treatment
The treatment process is fundamentally different for patients with and without a complicated fracture.
The first step in treating a nondisplaced fracture is excision to clear the joint cavity of exudate and blood. A small amount of novocaine solution is then injected into the joint cavity and the joint is immobilized with a plaster cast. After the knee joint is flexed by 5-10 degrees, the limb is immobilized with a plaster cast.
The duration of the plaster cast is about 2-3 months, after which physical therapy is required as a rehabilitation measure. During the rehabilitation period, it is important to start training the thigh muscles. This happens just 2-3 days after the plaster cast is applied by elevating the limb. Later, after about 7-10 days, crutches can be used, but the joint must not be put under any strain.
Treatment measures for fractures with displaced bone fragments may vary, but initially reduction is required, that is, the displaced structures must be returned to their normal anatomical position:
- After determining the severity and type of fracture, the specialist performs a manual reduction under anesthesia, immobilizing the upper limb and manipulating the lower one. An immobilizing plaster cast is then applied for the required period of time.
- If the fracture is displaced by more than 3 mm, the doctor may also apply permanent traction. The fracture is slowly reduced by applying a special splint and using a weight system. After a few weeks, if the reduction is successful, the traction system is replaced with a plaster cast.
If the conservative method does not bring the desired result or the fracture is very complex, surgery is performed. The displaced fragments of the fracture are fixed with screws during the operation, and permanent healing of the fracture also occurs, followed by the removal of the screws.
Diagnosis of a fracture of the humeral head
The diagnosis of a condyle fracture is only certain for the traumatologist if the condyle is displaced by more than 4 mm. The fracture is diagnosed after a thorough examination by a trauma surgeon and an x-ray. The severity and type of fracture can be clearly seen on the x-rays.
A fracture of the tibial condyle is a fairly serious injury that requires mandatory hospitalization after initial care. Complete healing and recovery of the condyle takes 5-6 months after injury.
Treatment for a condylar fracture depends on whether there is displacement. For fractures without displacement, a puncture is performed to remove blood and fluid. The entire leg from the buttocks to the toes is then put in a cast to stabilize it.
If the fracture is found to be dislocated, the trauma surgeon will perform repositioning and remove the dislocation, followed by skeletal traction for up to six weeks. Many bone fractures require surgical repair in which the bone fragments are held together with screws, pins, staples, or steel plates.
For any type of fracture, it is strongly recommended to gradually increase the load on the joint 4-6 weeks after the injury. Doctors recommend therapeutic exercises in which the patient moves the knee joint under the close supervision of a medical professional. Massages and heat treatments are also indicated for the patient.
Complications of fractures of the lateral humeral condyle
Type I and II lateral humerus fractures The following complications may occur:
1) Valgus deformity of the elbow joint;
2) external displacement of the forearm;
3) arthritis due to rupture of the joint capsule;
(4) late ulnar nerve palsy;
(5) bony hypertrophy with subsequent development of varus deformity of the elbow joint in children.
Publisher: Iskander Milewski. Release update date: 3/18/2021
The information contained on this website requires consultation with a doctor and is not a substitute for direct consultation with a doctor.
Please refer to the User Agreement for further details.
causes of injuries
In a car accident, the impact of the legs against the front seat or dashboard is significant. If the legs are bent at the knee joint, the joint heads are more likely to break. In severe impacts, the direction of the force also plays a role - this injury is characterized by a direct impact on the lateral protrusion of the knee.
Low-energy injuries occur from a slight impact or a simple fall. The main role is played by a disorder of the bone structure, such as occurs in osteoporosis or as a result of age-related changes.
If there is an isolated fracture of the lateral condyle, it is likely that the tibia will be forcibly deflected outward. If it moves medially, the fracture is in the medial structure.
How do you diagnose a femoral condyle fracture?
- The main syndrome with this injury is pain. The pain is localized in the knee joint, which becomes flattened and loses its usual contours;
- Internal bleeding causes tissue bulging, swelling, and pain on palpation;
- When you press on the kneecap, you can feel its abnormal position and how it 'bounces' under the pressure of the blood that has pooled in the joint;
- If the condyle is displaced, this is reflected in a deviation of the tibia to the side;
- The patient cannot perform active movements, and passive movements cause acute pain.
Such symptoms occur with fractures of the kneecap and tibial condyle, as well as with sprains of the knee ligaments and meniscus injuries. For this reason, additional diagnostics are required for an accurate diagnosis. Fractures of the femoral condyles differ from fractures of the femoral condyles of the lower leg in that in the latter the pain occurs above the joint space of the knee, while in the latter it lies below it.
diagnosis of pathology
The diagnosis is made based on the clinical data and the methods of additional examinations. Diagnosis begins with an interview and examination of the patient. The doctor pays attention to the visual signs of fractures that are characteristic of condylar injuries. When taking an anamnesis, attention must be paid to the type of injury, i.e. the patient must describe it in detail when talking to the doctor.
- The 'gold standard' is to have an X-ray taken. The X-ray image is made in two projections - straight and lateral. There are other examination methods, but they are used less frequently.
- If the X-ray results are inconclusive or there are doubts, a computer tomography is performed.
- MRI does not provide the necessary information about the condition of the bone - this method is used when there is a risk of soft tissue injury and trauma must be ruled out.
What are the characteristics of femoral condyle fractures?
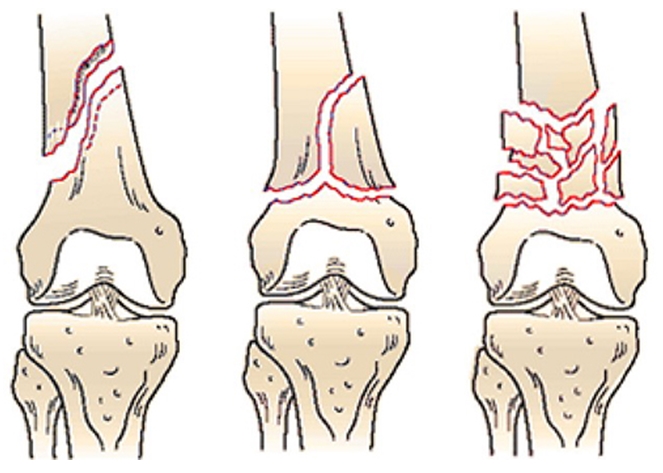
If the fracture line touches the articular surface of the femur, it is called an intra-articular fracture, and if the fracture line does not 'penetrate' the knee joint, it is called an extra-articular fracture. There are several variations of the classic fracture line, which can be seen in the illustrations.
Extra-articular fractures of the distal (lower) part of the femur. These fractures are sometimes referred to as supracondylar fractures of the femur or distal femoral metapophysis fractures. In none of the three cases shown does the fracture line extend to the articular surface of the femoral condyles, which is why they are referred to as extra-articular fractures.
Intra-articular fractures of a single condyle. In this case, there is a fracture of only one of the condyles (external or internal). They are a fracture of the external condyle on the left side, a fracture of the internal condyle in the middle, and a fracture of the posterior edge of the external condyle on the right side.
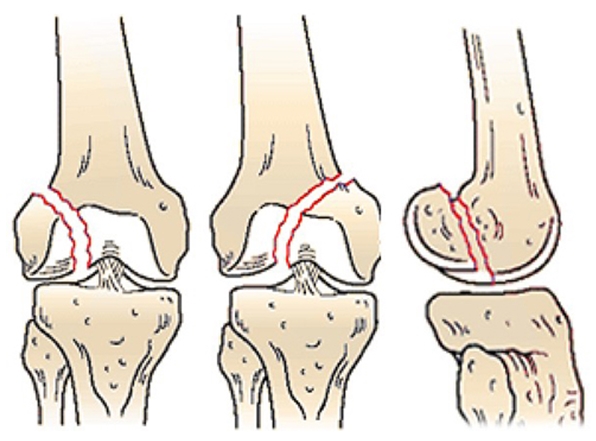
Transcondylar intra-articular fractures: Fracture of both the internal and external condyles. On the left a Y-shaped fracture, in the middle both condyles and the metaepiphysis (supraarticular zone) are affected. Right: severe fracture of both condyles.
Injuries can damage not only the bones, but also the soft tissues (skin, muscles, ligaments, blood vessels, nerves). If the continuity of the skin is broken, the break is considered an open fracture. Damage to blood vessels, especially the popliteal artery, is very dangerous in femoral condylar fractures as it can lead to catastrophic bleeding of the lower limbs and eventually even amputation. This is why it is so important to see a doctor as soon as possible if you have a fracture.
Most femoral condyle fractures require surgery - osteosynthesis, in which the fragments are repositioned and the broken bone is fixed with screws or a plate and screws. In some cases, a locking pin, an intramedullary rod with screws, is used. In intra-articular fractures, it is important to restore the articular surface as accurately as possible, to the millimeter, to avoid displacement of the fragments. This reduces the risk of knee osteoarthritis, which can lead to complications such as post-traumatic arthritis.
diagnosis

The diagnosis of a distal femur fracture is based on examination and x-ray findings. During the examination, the doctor will ask you about the circumstances of your injury. Try to describe the incident in as much detail but also as succinctly as possible. Don't forget to include any symptoms you previously described (numbness, etc.).
The type of fracture can be determined using X-ray images taken in two projections - straight and lateral. Sometimes additional projections are required, e.g. B. oblique, etc. Additional x-rays will be determined by the doctor and may be necessary if the nature of the fracture is difficult to determine from standard x-rays.
However, in some cases it is not possible to accurately determine the nature of the fracture from X-ray images and a CT scan (or multi-slice computed tomography - MSCT) is performed. It is not always advisable to do a CT scan before a simple x-ray.
MRI is less informative than CT when it comes to diagnosing the type of fracture. However, it is often used when conventional x-rays do not reveal a fracture in knee injuries and the doctor is looking for ligaments, menisci and other soft tissue structures. At this point, a fracture of the posterior femoral condyle must be mentioned, the so-called Goff fracture. It is often not visible on conventional x-rays, but it is clearly visible on MRI images.
ICD-10


An intra-articular fracture is an injury to the bone within the joint capsule. It is a complex injury that requires increased attention from the trauma surgeon and specific treatment, since the extent of movement depends on how accurately the articular surfaces have been restored. It can occur in any joint, large or small. Intra-articular fractures of the large joints of the limbs are of greatest clinical importance because of the possible long-term consequences.

causes
Causes can include accidents at home, while playing sports (fall, twisting of limbs, indirect or direct impact), traffic accidents, falls from heights, natural disasters or accidents at work. In all cases, with the exception of domestic and sports injuries, there is a high probability of combined or combined injuries. Intra-articular fractures can be combined with other limb fractures, blunt abdominal trauma, cranial trauma, pelvic fractures, genitourinary trauma and thoracic trauma.
Fractures of the humeral neck and head usually occur in older people and are the result of a fall on the retracted arm, shoulder or elbow. An injury to the elbow joint can occur at any age, but is more common in children and young patients with an active lifestyle. The cause is usually a fall with an outstretched arm or bent elbow. Wrist fractures can also occur in people of all ages, but the vast majority of patients are children and the elderly. The typical mechanism of injury is a fall onto an upright arm with support in the hand.
Fractures of the femoral neck and head are common in older people and result from falls. Knee injuries are more common in athletes and working-age people, and the mechanism of injury can range from a fall on the knee to a fall and direct impact. Ankle fractures occur in patients of all ages and are usually due to a fall.
diagnosis
The diagnosis of a tibial condyle fracture is made by a traumatologist based on the history, external examination and additional tests. The following procedures are applied:
- Objective investigation.. Fractures of the epiphysis and metaphysis of the tibia are manifested by acute pain, aggravated by pressure on the injured condyle, typical abnormalities in the configuration of the injured area, and rapid significant hemarthrosis. The creping of the fragments is uncharacteristic.
- X-ray of the knee joint. It is an essential part of instrumental diagnostics. The x-rays are taken in two projections. In the vast majority of cases, not only the presence of a condylar fracture, but also the type of fracture displacement can be reliably determined in this way.
- Other imaging procedures. If the X-ray image is not informative, the patient is referred for a CT scan of the knee joint. If there is suspicion of accompanying soft tissue damage (ligaments or meniscus), an MRI examination of the knee joint is indicated.
If there is evidence of neurovascular damage, a vascular surgeon and a neurosurgeon should be consulted.
CT scan of the knee joint. Fragmentary fracture of the lateral condyle with displacement.
Treatment of a fracture of the tibial condyle
First aid consists of immobilizing the limb with a splint from the foot to the upper third of the thigh and emergency transport to a medical facility. The illness is treated in the trauma ward. Upon admission, the trauma surgeon performs an LP of the knee joint and injects Novocaine to anesthetize the fracture. Further treatment depends on the characteristics of the injury.
Conservative treatment
For incomplete fractures, tibia fractures and marginal fractures without dislocation, the treatment plan is a plaster cast for 6-8 weeks. The patient is recommended to take painkillers, use crutches and elevate the limb during rest periods. The patient should be referred for NFZ and physiotherapy. After immobilization is completed, the patient is recommended to use crutches and not support the limb for 3 months from the day of injury.
For fractures with displacement, treatment includes one-stage manual reduction followed by traction or traction without prior reduction, depending on the type of tibial injury. For minor displacements, adhesive traction is acceptable. Fracture of one or both condyles with significant displacement, fracture of one condyle with subluxation, or dislocation of the other condyle results in skeletal traction.
Traction is typically maintained for 6 weeks, during which physical therapy is performed. Traction is then removed and the patient is instructed to walk on crutches without supporting the leg. In intermetatarsal fractures of the upper tibia, healing is usually delayed, so that light weight bearing on the leg is possible after 2 months and complete relief after 4-6 months.
surgical treatment
Indications for surgical treatment are unsuccessful attempts at reanastomosis, severe compression of the fragment, impingement in the joint cavity, entrapment of vessels or nerves and fracture of the intercondylar atrium with displacement when closed reduction is ineffective. The operation is routinely performed a few days after admission to the hospital.
Fracture of the tibial condyle
- SECTION MENU
- Allergology-Immunology
- Allergic rhinoconjunctivitis
- Allergy to grass pollen
- Allergic dermatitis
- Allergy to pets
- Allergy to house dust and its components
- Allergy to insects
- Allergy to pollen
- Allergy to tree pollen
- Allergy to grass pollen
- Eczema and other immune-mediated dermatoses
- Allergy to insect bites
- angioedema and Quincke's edema
- Atopic dermatitis
- immune disorders
- Allergy to drugs
- Acute and chronic urticaria
- Early signs of allergy
- Allergic alveolitis
- Why do my ovaries hurt and what can I do about it?
- Dysplasia of the cervix
- How to prepare for a visit to the gynecologist?
- Causes of abdominal pain
- ovarian apoplexy
- Bartholin's inflammation, cyst or abscess
- Ectopic pregnancy
- Hematometer
- hydrosalpinx
- Hyperplastic endometrial processes (hyperplasia, polyps)
- Cervical leukoplakia
- endometritis
- Uterine fibroids
- menstrual disorders
- Ovarian tumors (cysts and cysts)
- Prolapse and prolapse of the uterus and vagina
- Polycystic ovaries
- cervical polyps
- Spontaneous termination of pregnancy
- endometriosis
- Cervical erosion and ectropion
- Current approaches to the diagnosis of cervical abnormalities
- sinus infection
- Chronic rhinitis
- Nasal furunculosis
- pharyngitis
- inflammation of the tonsils
- Polypoid stomatitis
- otitis media
- acute rhinitis
- nosebleeds
- laryngitis
- Distorted nasal septum
- ENT diagnosis
- Repair of a peri-tonsillar abscess
Treatment
A fracture of the condyle is treated as an inpatient. If a sprain has occurred, a puncture is made to drain accumulated blood into the joint. In the next phase, the joint is immobilized with a plaster cast from the buttocks to the toes. A state of rest is a prerequisite for successful treatment.
When treating such fractures, an individual approach is taken and the injured joint is put under early strain if necessary. The treatment algorithm depends on the severity of the injury.
A condylar fracture requires immediate treatment by a surgeon. The earlier the patient is treated, the better the result. Inadequate treatment or failure to follow medical advice can lead to complications, including joint instability.
- Мыщелка берцовой.
- tibia and fibula.
- Bones of the tarsal bone of the hand.
- Fracture of the 5th metatarsal.
- Fracture of the heel bone.
- metatarsal and metacarpal bones.
- Fracture of the calcaneus of the foot.
- Bone structure of the navicular foot.
