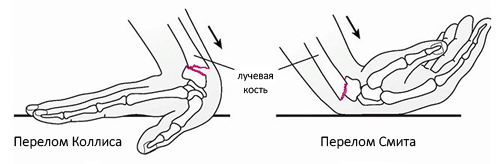
Depending on the fracture ratio of the radius bone, a distinction is made between:
- DUPUYTREN'S FRACTURE
- clinical picture
- Anatomical Features
- mechanism of injury
- causes
- classification
- Treatment
- What complications can arise from an untreated ankle bone fracture that does not heal properly?
- diagnostic procedures
- Investigation
- Treatment of radius fractures
- material and methods
- Results and discussion
- What are leg bone cysts and what types of cysts are there?
- signs
- Symptoms of a fracture of the foot (metatarsal bone)
- Symptoms of a fracture of the foot (metatarsal)
DUPUYTREN'S FRACTURE
Dupuytren's fracture (G. Dupuytren, French surgeon, 1777-1835) is a fracture of the medial malleolus and fibula in the lower third with a tear of the syndesmotic ligaments between the tibia. This fracture often results in an outward subluxation of the foot. The Dupuytren fracture is widespread and was described by H. Dupuytren in 1819.
The mechanism of this fracture is a pronation-abduction fracture. The foot has a natural valgus position of 10° and is therefore more likely to be turned outwards in the event of trauma. Due to the strength of the medial (deltoid) ligament, the medial malleolus is hyperextended and the talus is valgus. The talus binds against the lateral malleolus and the ankle fractures with a tear of the anterior ligament or, more commonly, both ligaments.
clinical picture
Dupuytren's fractures are usually accompanied by swelling of the ankle joint. When the foot is subluxated outward, an abnormal valgus position of the foot occurs, which is particularly evident in the dorsal view. Palpation reveals acute tenderness of the medial malleolus, talus, and intercondylar syndesmosis. Active and passive movements of the joint are extremely painful and restricted.

Figure 1: Anteroposterior radiograph of the ankle: 1 – normal (for comparison); 2 – with Dupuytren fracture (fractures of the fibula and medial malleolus, tear of the inferior intercondylar syndesmosis).

Fig. 2: X-ray of the ankle joint in Dupuytren fracture: 1 - in the direct projection (both ankle fractures - indicated by arrows, subluxation of the foot outwards); 2 – in the lateral projection (arrow points to the fracture gap of the lateral malleolus).
The x-ray image in direct projection shows the ankle fracture. The fracture line of the medial malleolus is clearly visible, usually at the level of the joint space, and that of the lateral malleolus is at or above the joint space. At the same time, a clear displacement of the fragments and possible diastasis, i.e. articular fork separation, are visible (Figures 1 and 2). Of great importance for the diagnosis of a tear of the lower intercondylar condyle is the examination of comparative anteroposterior images (on the same film) of both ankle joints in normal position or with symmetrical 27° internal rotation.
Anatomical Features
The talus is small and lies between the shinbone and the heel bone.

About 60 % of its surface is of hyaline cartilage than Os talus is involved in three joints at the same time:
- The ankle, the block ostalus with the shinbone (tibia).
- Talus and Calcaneus – its posterior articulation with the calcaneus.
- Talaneo-femoral – the head of the talus bone with the navicular bone, part of the Chopara joint.
The hyaline cartilage plexus causes osteochondral fractures of the talus (approximately 4 % of injuries), which often lead to arthritis and disruption of foot biomechanics.
The talus is covered by strong and dense ligaments that provide stability to the mentioned joints and thus prevent its ruptures:
When walking and running, am os talus 100 % of body weight when walking and running, giving it a considerable, though not unlimited, margin of safety.
mechanism of injury
A talus fracture is usually caused by three different pathological processes:
- Compression between the shin and heel bone. These injuries result in compression fractures of the shaft of the Ostalus.
- Hyperextension of the foot leading to fractures of the head and neck of the talus.
- Excessive flexion resulting in a fracture of the posterior process of the ostalus.
These injuries result from high-energy impacts: traffic accidents, sporting events, falls from heights, etc.
Often injuries Wasps talus Often, injuries to the os talus are combined with a fracture of the calcaneus, damage to the integrity of the other bones of the tarsus, metatarsal and distal tibia.
causes
A fracture of the heel bone is almost always caused by a fall while standing. The integrity of the bone is compromised by the impact of the heel on the ground. Very rarely, injuries are caused by an impact on the sole from below (e.g. in an explosion). The height, surface condition and strength properties of the heel bone determine the severity of the fracture. In older patients with osteoporosis, the injury may be caused by a slight impact, such as B. if your foot slips on a step or falls off a chair.
The heel bone is the largest bone in the foot and carries most of the load when standing and walking. The heel bone consists of two main parts: the body and the posterior bulb. The heel bone is connected to the talus bone at the top and to the elbow bone at the front. The heel bone acts as a connecting link between the heel bone and the tibia bone. When you fall on your heel, the gravity of the entire body is transferred through the lower leg bones to the ankle bone, which wedges into the heel bone and separates it.
The nature of the fracture of the heel bone and the direction of displacement of its fragments depend on the height of the fall and the position of the foot at the time of impact with the ground. Due to the action of the traumatic force and pull of the triceps muscle, the posterior parts of the bone are displaced upward, resulting in a flattening of the longitudinal arch. If there is no repositioning or residual deformity, this can lead to impaired posture and walking after the bone fragments have healed.
classification
Heel fractures can be compression fractures, isolated fractures and marginal fractures with or without displacement. In modern traumatology and orthopedics, two large groups of injuries are distinguished:
- intra-articular – Intra-articular fractures account for 80 % of all calcaneal injuries and include fractures extending into the ankle joint.
- extra-articular – Extra-articular fractures include fractures of the calcaneus and tuberosity, which account for 20 % of all calcaneus fractures.
In turn, nodular fractures are divided into four groups:

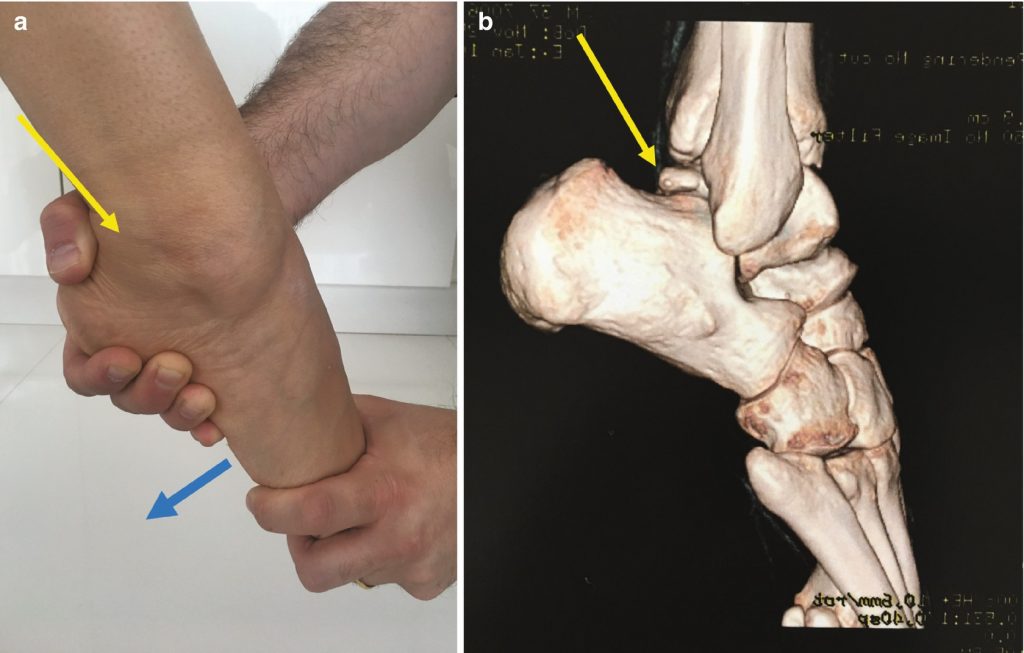
Computed tomography of the foot (3D reconstruction). Fragmented fracture of the calcaneus with multidirectional displacement of the fragments.
Treatment
Treatment for a heel bone fracture depends on the type of fracture and the severity of the injury. First, a splint is applied to protect the foot and ankle from movement. If the fracture is stable and the joints are well aligned, surgery may not be necessary. The attending physician may recommend:
- Immobilization. A cast holds the bones of the foot and ankle together while they heal. As a rule, the patient has to wear a cast for 6-8 weeks and is only allowed to put minimal weight on the leg.
- Rehabilitation. Once the cast is removed, the patient will receive physical therapy to restore strength and function to the foot and ankle.
Ankle surgery is recommended for most talus fractures. If the bones are displaced, the surgeon will perform surgery to repair them.
If the bone is broken into several pieces, the surgeon can perform open reduction and internal fixation. During this surgery, the bone fragments are put back into place and held together with a metal plate and/or screws until the bone heals.
If the swelling is too great, the surgeon may use an external fixator. With an external fixator, the surgeon inserts large pins into the bone to hold it in place. The pins are visible on the outside of the skin and are held together by special rods.
What complications can arise from an untreated ankle bone fracture that does not heal properly?
A broken ankle bone can cause serious complications if left untreated or not healed properly:
- Post-traumatic arthritis. When the ankle bone is injured, the surrounding cartilage is also damaged. The deformation of the cartilage can lead to signs of wear and tear in the joint. This can lead to osteoarthritis.
- Malunion. An abnormal anastomosis can lead to long-term problems such as difficulty walking
- Incompetence. Broken bones that do not heal after a long period of time
- Valve necrosis or osteonecrosis. The blood supply to the ankle bone can be interrupted by a fracture. Without an adequate blood supply, the bone cells die. This can lead to bone destruction.
diagnostic procedures
- X-ray examination in side projection; with loaded foot, foot in sole flexion.
- Computed Tomography.
- Magnetic resonance imaging (MRI) is the preferred method to determine the presence and extent of ossifications, associated pathologies, and soft tissue and bone injuries. The MRI during flexion/extension provides information about the mobility of the triangular bone.
- Bone scintigraphy with technetium shows increased uptake in the area of the triangular bone.

Investigation
Palpation between the Achilles tendon and the long fibula tendon may reveal pain and swelling.
Perform a passive and forced plantar flexion test with repeated rapid passive flexion in neutral position and with internal and external rotation at the site of maximum plantar flexion. In triangular bone syndrome, there is strong friction between the shin and heel.
Treatment of radius fractures
The main goals of fracture treatment are to restore the anatomical shape of the bone, ensure the stability of its attachment, prevent complications and carry out comprehensive rehabilitation and reconstructive treatment. Depending on the location/character of the fracture, treatment for a fracture of the radius bone can be conservative or surgical. Let us briefly consider the treatment of a fracture of the radius bone in the typical position (distal metaepiphysis of the radius bone). To date, the most common treatment for fractures in this area is closed manual reduction, followed by immobilization with a plaster splint applied for a few days until the swelling subsides, after which a plaster cast is applied for 4-5 weeks.

The disadvantage of this method is the difficulty of precisely repositioning the bone fragment, since in the event of a displacement, even minimal displacement of the articular surfaces/shortening of the radius bone (2 mm) occurs arthrosis. In practice, a large proportion of fractures do not respond well to closed manual reduction in the typical location and remain stable upon subsequent immobilization with plaster casts, that is, they are unstable and prone to secondary displacement, requiring surgical treatment.
In some cases, percutaneous spoke fixation (closed spoke osteosynthesis) with subsequent X-rays is performed to better immobilize the bone fragments. The duration of healing of a radial humerus fracture depends on several factors: the accuracy of repositioning the bone fragments, the individual characteristics of the body and is on average 4-5 weeks. In case of unsuccessful reduction, a second reduction is performed, which prolongs the bone healing time.
material and methods
The generalizations proposed in this article are based on the experience of using the method of periosteal fixation according to the developed technique in the treatment of patients with central comminuted fractures and dislocations of femoral fractures. Between 2004 and 2009, 23 patients with central comminuted fractures and dislocations of 25 talus fractures were operated on in the clinics of the Research Institute of Traumatology and Orthopedics of the Donetsk National Medical University.
In our opinion, the best classification in terms of treatment tactics and prognosis is that of L. Hawkins [5] with the addition of Canale and Kelly [4], which divides ankle bone injuries into 4 types. The treatment tactics for fractures of type I (periarticular, marginal and arch block fractures) and type II (central fractures with neck or shaft displacement up to 1 mm) are well described in the literature and are generally not controversial. Type III and type IV fractures as well as talar fractures (central amputation fractures and multijoint fractures of the neck or shaft with or without displacement of the fragments) usually pose the greatest treatment and prognosis problems.
The distribution of injuries by fracture type in our study was as follows: type III in 16 (64 %) cases, type IV in 7 (28 %), and 2 patients had complete isolated plate displacement, defined as a separate type V by Nikitin [1]. The lesions were open in 14 (56 %) cases and closed in 11 (44 %). The women's group consisted of 5 and the men's group included 18.
All injuries were the result of a high-energy impact: a fall from height in 8 (32 %) cases and 17 (68 %) as a result of a traffic accident. In 12 (48 %) cases, fractures of the calcaneus were combined with fractures of other parts of the foot (4 cases, 16 %) and ankle (8 cases, 32 %). In addition, 4 (16 %) patients had concurrent and multiple injuries to the spine and, in one case, the hip joint.
Results and discussion
Given the peculiarities of the structure (large articular surface) and blood supply to the heel bone, anatomical repositioning of the fragments with stable fixation is a mandatory requirement to ensure favorable treatment results. This prescription allows the use of stable functional osteosynthesis with compression screws, including minimally invasive techniques such as cannulated screws. This technique makes it possible to avoid external immobilization in the postoperative period, but the supporting function of the injured limb remains impossible for a long period of time and the auto-myocompression factor of the injured talar bone is not eliminated. This prevents revascularization and promotes aseptic necrosis and bone collapse [6]. These unfavorable factors can be eliminated by using transepiphyseal osteosynthesis procedures.
Subchondral bone dislocations were reduced in a closed manner. In four cases, surgical access to the talus was achieved through an existing medial malleolus fracture with subsequent osteosynthesis using a CITO screw or a screwdriver. In all other cases, open lateral repositioning or through an existing wound was performed. The tendons of the eye muscles were crossed for better visualization of the fragments. The fragments were fixed with Kirschner needles or thin screws.
The surgical treatment method developed by us includes open anatomical repositioning of talar bone fragments, osteosynthesis of fractures with screws or spokes (both with their removal on the skin and in a submerged version) and transperiosteal osteosynthesis with a wire-spike device. The peculiarity of the latter is that the external structure consists of two modules on the lower leg and the foot. In the early postoperative period, the modules were rigidly fixed with threaded rods, which allowed us to control the amount of distraction at the ankle and subtalar joints and ensure the support function of the limb in the device. At week 4-5, rigid fixation between the AVF modules was replaced with articulated fixation while maintaining moderate distraction. The joints were centered in the axis of rotation of the ankle joint to allow the patient active and passive movements in the ankle joint. This movement was made possible by a rubber strap and a rigid insole with a supinator that shapes the arch of the foot.
What are leg bone cysts and what types of cysts are there?
Cysts are cavities inside the bone that are filled with fluid. However, a leg bone cyst is not uncommon. Such tumors most often form in the long bones: femur, tibia or fibula. The foot is a rare location for bone cysts.
Among the bones that make up the foot, such tumors occur more commonly in the heel bone and less commonly in the talus bone. The heel bone, together with the shin bone, forms the ankle joint and plays an important role in walking. During movement, it supports almost the entire body weight and transfers the load to the heel and midfoot. This makes it, like the heel bone, very susceptible to the formation of cysts and subsequent fractures.
A calcaneal cyst most commonly forms in the shaft of the heel bone. It was first described in the late 19th century. However, it is still confused with bursitis, so patients do not receive the necessary treatment and risk complications. This pathology accounts for only 1-1.5 % of all cases of bone cysts.
The tarsal bones are five small long bones that are articulated to the tarsal bone and together form the arch of the foot. They serve to cushion static loads and walking. Although the metatarsals are tubular, cysts are rare. They form primarily in the 1st and 2nd metatarsals.
Cysts of the heel bone and other structures of the foot are most commonly found in children. In adults, especially athletes, they can form as a result of constant traumatic factors.
Solitary and aneurysmal cysts are most common in the foot. The former are unilocular tumors filled with serous fluid. They can form in early childhood, but usually only become visible in adolescence. Arterial cysts are more aggressive and manifest quickly. They are multi-chambered masses that contain blood inside.
signs
When a leg bone cyst begins to form and grow, there are no symptoms. They only appear when the cyst has reached a sufficient size. In children, a completely asymptomatic course is sometimes observed, and the neoplasm disappears spontaneously with the completion of skeletal formation.
However, the cyst can also be characterized by aggressive growth. In this case, clinical symptoms appear, the localization of which depends on the location of the defect. The following symptoms are characteristic of a foot bone cyst
– Pain that occurs and worsens with walking, running, jumping and other exertions;
– Dense swelling in the heel, ankle and metatarsal area that can be felt;
– Discomfort when wearing tight shoes and high heels.
A talar cyst can cause pain and other symptoms in the heel and metatarsal area because it is closely attached to these bones.
Often the first symptom of a bone cyst is a pathological fracture. This is accompanied by swelling of the foot, heel, a pronounced restriction of movement and even pain during strain, which occurs against the background of maintaining the normal range of motion of the ankle joint.
A fracture of the talus bone, which forms the ankle joint, is particularly dangerous due to its specific structure. This bone is characterized by an intensive blood supply, which is acutely interrupted in the event of a pathological fracture. This can lead to avascular necrosis and even disability.
Uncomplicated fractures of the metatarsals that are caused by a cyst usually heal without sequelae. The cyst cavity is closed. This is especially true for children.
Symptoms of a fracture of the foot (metatarsal bone)
May be caused by violent trauma with a severe foreign body or a crush. Rarely, the injury occurs indirectly - through active excessive flexion of the sole of the foot. These fractures usually occur in connection with injuries to the navicular bone, and possibly also with a fracture of the hyoid bone. The fracture of the navicular bone begins to move inward and backward. There will be slight swelling and pain. Walking is painful, but the injury does not limit movement. The symptom is a palpable bulge at the site of injury and a typical preference to walk only on the heel. The diagnosis is clarified by an X-ray examination.
The symptoms of this type of foot fracture are difficult to diagnose and are very similar to those of a navicular bone injury. The difference may be that the pain occurs on the outside of the foot with an elbow injury and on the inside of the foot with a sphenoid fracture. It is also necessary to distinguish a sesamoid fracture from the fragments of the elbow and sphenoid bones visible on the X-ray.
Symptoms of a fracture of the foot (metatarsal)
This is the most common form of foot fracture, with the 1st and 4th ankle bones most commonly affected. Fractures of the pollices can be diagnosed with direct trauma (car accident, dropping a heavy object), that is, with injuries to all metatarsals. Symptoms of a foot fracture depend on the severity of the injury and may include multiple swellings, severe pain, and inability to walk. X-rays are taken from two sides - oblique pronation at 50° and dorsiflexion and plantar flexion.
As with metatarsal trauma, the phalanges are directly injured. The proximal phalanges are most susceptible to fractures; the distal phalanges are less commonly affected. The rarest case is a fracture of the middle phalanx of the foot. The symptoms of a foot fracture are typical of small fractures, the pain is tolerable, and there is little or no swelling. The diagnosis is confirmed by an x-ray.
The symptoms of a foot fracture are very diverse and can be differentiated through a thorough examination by a surgeon, an X-ray examination and, of course, timely medical attention.
Read more:- Fracture of the calcaneus of the foot.
- Fracture of the articular process of the heel bone.
- pelvic subluxation.
- heel bone injury.
- Displacement fracture of the heel bone.
- Fracture of the lateral condyle.
- Anatomy of the heel bone x-ray.
- tibia and fibula.
