Treatment depends on the broken bone and the type of fracture, but usually involves wearing a splint or special shoes to protect the foot.
- fractures of the foot
- species
- Epidemiology / Etiology
- Clinical Manifestations
- symptoms
- signs of a fracture
- classification
- Symptoms of a heel bone fracture
- pathogenesis
- Symptoms of osteoma of the bones
- broken bones in the foot
- Diagnosis of fractures of the foot bones
- Symptoms and diagnosis of an elbow fracture
- Conservative treatment of a fracture of the elbow
- Classification of hand bone fractures
- wrist fractures
- Fractures of the navicular bones
- Surgery for fractures of the leg bones
- rehabilitation
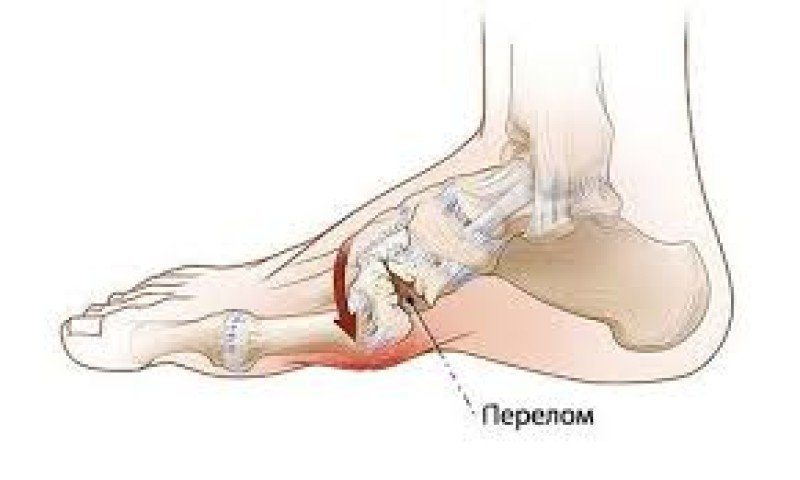
fractures of the foot
A foot fracture is a condition where one or more bones of the human foot are broken. This injury is very common, accounting for a tenth of all fractures.
The causes of a disorder of the foot anatomy can be divided into two groups - direct and indirect impact, with the following factors also being possible
- foot compression from tight footwear;
- crushing the foot with a heavy object or a sharp blow to the foot;
- rolling up the foot;
- Improper landing after a fall or jump;
- injuries at home;
- crushing of the toes (e.g. from a hard kick on the foot);
- disasters (fall from a bicycle, car accident, unsuccessful parachute jump, etc.);
- Bone diseases that destroy bone structure and reduce bone strength;
- bone tumors.
species
The following types of this disease are distinguished:
- open;
- closed;
- solitary;
- multiple;
- with or without displacement of bone fragments;
- dislocations of fractures.
The fractures of these bones are distinguished according to their location:
Regardless of the type of lesion, the consequences should not be underestimated, since the foot is the support for the entire body, and any anomaly can lead to disruption - the development of flat feet or secondary arthritis.
Epidemiology / Etiology
It is estimated that 15-20 % of traumatic fractures are stress fractures. This type of fracture is associated with physical activity that involves sustained exertion (such as running or walking). About 50 % of stress fractures occur in the tibia; however, a stress fracture can occur anywhere. The foot (especially the second metatarsal) is another common site for stress fractures. It has been found that women are 1.5 to 12 times more likely to develop stress fractures than men.
Georgy Temichev's seminar 'Diagnosis and Therapy of Lower Limb Problems'. Gait and run analysis'. Learn more…
Stress fractures can occur due to a number of factors including activity level, bone strength, anti-inflammatory medications, radiation, nutritional status, osteoporosis, endocrine disorders, lack of sleep, and collagen abnormalities. The recurrence rate of stress fractures depends on bone chemistry, adjacent muscle attachments, vascular network, systemic factors, and exercise. Other possible risk factors include age, gender, footwear, and exercise regime. Female athletes are particularly vulnerable to the athletic 'triad' (amenorrhea, eating disorders and osteoporosis), but male endurance athletes with abnormally low sex hormone levels are also at risk of stress fractures.
From a biomechanical perspective, stress fractures can be caused by muscle fatigue that overloads the bone. In addition, it has been suggested that the position of the lower limbs influences the risk of stress fractures. In addition, early studies have shown that low tibial thickness, excessive external rotation of the thigh, ankle varus and metatarsal alignment, ankle hyperpronation, pes cavus, and leg length discrepancy may increase the risk of stress fractures in athletes (the data for some factors are inconclusive).
Clinical Manifestations
The clinical picture can vary from patient to patient, so a complete medical history should be taken to determine the likelihood of a stress fracture. A person may describe a worsening of symptoms during activity and not specify the nature of the injury. The pain may initially appear with activity but then become constant. The patient may not provide the physiotherapist with important information about an increase or change in activity. The patient may have slight swelling and redness at the site of pain, focal or point tenderness (touchable with a finger), leg length discrepancy, and increased pain when standing on the leg, provoking antalgic gait. Testing with a tuning fork along the painful area should produce a strong sensation of pain in the event of a fracture. Track and field athletes and military personnel commonly suffer from stress fractures. Patients are at greater risk if they do not get enough rest between training or competitions. Young female athletes (in this sample) are more prone to stress fractures due to the triad of bone mass damage.
Depending on the location of the pain, different diagnoses are made. Other possible diagnoses include infection, tumor, compartment syndrome, arthritis, nerve compression lesion, medial tibial stress syndrome, and other soft tissue injuries.
Compartment syndrome is caused by compression within the muscular sheaths (compartments) of the lower leg, which are separated by layers of fascia. The compression in the sleeves can be caused by an increased demand for oxygen and the associated increased blood flow into the tight muscle. Patients may experience calf cramps, muscle tension, severe pain, hanging feet, and foot paraesthesia. An acute attack of compression syndrome is an emergency, and surgical fasciotomy is the primary treatment option.
symptoms
All types of broken bones share some common symptoms:
- Pains. It is strong and stabbing at the time of injury and becomes dull thereafter. The pain increases with axial loading.
- Deformity. When the fractures shift against each other, the leg or arm takes on an unnatural shape.
- Swelling. The swelling begins to increase immediately after the injury.
- Subcutaneous hemorrhages - hematomas. Sharp bones crush small blood vessels, causing blood to pool under the skin.
- functional impairment. When asked to move the injured leg or arm, the injured person is unable to do so due to severe pain, muscle strain, and ligament damage.
The most serious fractures involve skull bones, vertebrae, ribs and pelvic bones. These can cause damage to internal organs and the nervous system. Multiple fractures, which can lead to shock, are also dangerous.
signs of a fracture
There are relative and absolute signs of a fracture. Relative signs include:
- Hematomas due to internal bleeding as a result of vascular injuries. A swelling and large hematoma at the fracture site, causing severe pain when touched.
- Stinging and unbearable pain at the injured site. In rare cases, those affected lose consciousness due to the pain shock.
- Inability to move the limb (complete loss of motor function).
- Swelling of the soft tissues indicate a fracture or dislocation.
- In open fractures, fragments are clearly visible, while in closed fractures, curvature of the bone and unnatural alignment (no soft tissue fracture) are seen.
- Popping and crunching, and excessive mobility in the affected area.
- Loss of motor function (the person cannot move the limb and is in acute pain). Often the symptoms resemble a serious bruise or sprain, so a differential diagnosis is required.
classification
Heel bone fractures can be compression fractures, isolated fractures and marginal fractures, with and without displacement of the fragments. Modern traumatology and orthopedics distinguish two main groups of injuries:
- intra-articular – Intra-articular fractures account for 80 % of all calcaneus injuries and include fractures that extend to the ankle.
- extra-articular – Extra-articular fractures include fractures of the calcaneus and tuberosity, which account for 20 % of all calcaneus fractures.
In turn, nodular fractures are divided into four groups:
Computed tomography of the foot (3D reconstruction). Fragmentary fracture of the calcaneus with multidirectional displacement of the fragments.
Symptoms of a heel bone fracture
The patient complains of pain in the heel area. Examination reveals swelling in the heel area that rapidly spreads to the Achilles tendon, flattening and widening of the heel, and midsole hematoma. The contours of the Achilles heel are flattened. The height of the foot decreases and the width at the back increases. Bruising sometimes occurs on the lateral surfaces of the foot (below the ankles) a few hours after the injury.
Supporting the foot is not possible. The mobility of the ankle is preserved. Palpation of the heel is painful. When the heel area is compressed laterally, the pain increases and becomes unbearable. In compression fractures and injuries without fracture displacement, crepitation is imperceptible. In other cases, the presence of bone cartilage is a variable symptom.
pathogenesis
Until relatively recently, osteochondrosis was considered one of the manifestations of chronic sclerosing osteitis and was not treated as an independent pathology. The first osteoid osteoma to be recognized as a distinct disease was osteoid osteoma of bone. This tumor develops in tubular structures and appears as a small, diffuse fragment of bone tissue up to 20 mm in diameter. On closer imaging, a clear sclerotic reaction can be seen at the edge of the tumor. These osteomas can be cortical or cellular. Histological examination shows numerous osteoblasts and osteoclasts.
Microscopic examination of the pathology reveals clear contours delineating diffuse tissue permeated with blood vessels. In the central part of the osteoma are osteoid trabeculae and cords that are fused together. The altered tissue contains large osteoblasts with a large cell nucleus.
No hemocytoblasts or lipid tissues are present in the osteoma structure. Osteoclasts can be identified in isolated areas, arranged singly or in groups. When the integrity of the bone at the site of the osteoma is compromised, cartilaginous tissue can be seen within the osteoma, which also occurs in masses that develop beneath the articular cartilage. This is the structure of the central part of the tumor. Fibrous connective tissue is present at the periphery, which has the appearance of bands up to two millimeters wide. Then a thin layer of cortex can be seen – but this is not always the case.
[32], [33], [34], [35], [36], [37], [38]
Symptoms of osteoma of the bones
Osteomas usually develop slowly and without clear signs or symptoms. Osteomas mainly occur on the outer surface of the bone. The tumor can occur in any part of the skeletal system (exception: sternum). It is most commonly found on the bony surfaces of the appendix, cranial bones, shoulder, and hip.
The osteoma usually appears as a hard and smooth protuberance on the outer part of the bone that is immobile and painless. If the mass develops on the inside of the skull, the first symptoms are particularly pronounced and take the form of headaches, increased intracranial pressure, memory problems and seizures. If the osteoma develops in the region of the Turk's saddle, it can manifest itself as endocrine disorders.
Osteoma of the paranasal sinuses is often accompanied by these symptoms:
If the osteoma is located in the spinal region, the patient complains of pain. Compression of the spinal cord and deformity of the spine are diagnosed.
[39], [40], [41]
broken bones in the foot
Bone fractures of the foot also include toe fractures Toe fractures can occur in any toe and any part of the toe. Typically, the broken toe will be painful, swollen, and sore to palpation, and the nail may be discolored. Common. Read more and metatarsal fractures (metatarsal fractures) Metatarsal fractures can occur in the long bones of the metatarsal (metatarsal) bones. There are several types of metatarsal fractures, including stress fractures, Lisfranc fractures with. Read more ), the two small round bones at the base of the first toe (sesamoids) Sesamoid fractures can occur in the two small round bones at the base of the first toe (sesamoids). These sesamoids can be broken during running, hiking, and sports activities. Read more ), or bones in the back of the foot, including calcaneal fractures Calcaneal fractures occur in the heel bone, which is located in the back of the foot. Calcaneal fractures are usually caused by a high force and are therefore often associated with trauma. Read more .
Fractures in the bones of the feet can result from falling, tipping, or striking your foot directly with a hard object.
Fractured feet are very painful, and the pain often increases when you try to put weight on the foot.
Diagnosis of fractures of the foot bones
X-rays are usually required to diagnose fractures of the foot bones, with the exception of some toe fractures. In rare cases, computed tomography (CT) or magnetic resonance imaging (MRI) may be required.
Treatment of foot fractures depends on the broken bone and the type of fracture, but usually involves placing a splint (and possibly a cast) on the foot and ankle, or wearing a custom-made or open-toe shoe with Velcro and tightening Sole to avoid further injury.
The patient is often advised not to put weight on the foot for a period of time. The duration of this measure depends on the injury and can last up to several weeks. Doctors often advise patients to move their foot and ankle until the pain becomes bearable.
Therapeutic exercises are often required. This includes specific exercises to improve the flexibility and mobility of the injured foot and to strengthen the supporting muscles.
Copyright © 2023 Merck & Co, Inc, Rahway, NJ, USA and its subsidiaries. All rights reserved.
Symptoms and diagnosis of an elbow fracture
The main symptoms of a cubital fracture are:
- severe pain, which increases when pressing the 4th and 5th metatarsals and trying to move the foot;
- swelling at the site of injury;
- subcutaneous bleeding;
- Altered foot contour (displacement, displacement or subluxation of the bones);
- Abnormalities in the range of motion of the foot.

To make a diagnosis, the doctor (traumatologist, surgeon) palpates the injury site and examines the degree of restriction of movement of the foot. The differentiation of the injury is based on the X-ray image.
Conservative treatment of a fracture of the elbow
If the fracture of the elbow is classified as moderate, the treatment consists of a plaster cast for 3-6 weeks. This allows for proper adhesion and bone marrow formation. Also, medications are prescribed to eliminate pain and inflammation, dull swelling and speed up the healing process.

As an additional therapy, a complex of vitamins and minerals, calcium supplements and a special diet rich in protein, calcium, magnesium and fiber are prescribed. The duration of treatment depends on the characteristics of the fracture and the individual characteristics of the body.
Classification of hand bone fractures
Depending on the presence or absence of skin damage over the fracture, a distinction is made between:
- closed fractures - the integrity of the skin is intact;
- open fractures – there is a wound at the site of injury, which can be defined by bone fragments.
- No displacement – the fractured bone maintains its position and the fragments are closely aligned along the fracture line;
- displaced – the bone fragments move apart and cannot reconnect along the fracture line without being reconnected – repositioning.
By involving articular structures in the fracture:
- Extra-articular fractures – the fracture line is outside the articular cavity;
- Intra-articular fractures – the fracture line runs inside the joint cavity;
- Fracture dislocations - disruption of bone integrity associated with dislocation of an adjacent joint.
Hand fractures can also be classified by the number of fragments, the degree of displacement, and the presence of infection. The etiology of the fracture is also important - whether it is traumatic or pathological, i.e. caused by bone disease. All these factors affect the choice of treatment tactics for the fracture and, ultimately, the ability to fully restore the function of the injured wrist.
wrist fractures
The bones of the wrist are rarely fractured because of their shape, structure, and location. The scaphoid, the large bone at the base of the thumb, is most prone to fracture. The crescent and pea bones of the wrist are also commonly damaged. The triangular bone and the bones of the distal row - polygonal, trapezoidal, parietal and hooked bone - are extremely rare and are usually associated with dislocations of the corresponding joints.
Fractures of the navicular bones
Caused by a flexed-hand fall, a punch, or direct trauma to the wrist. Possible variants are:
- Intra-articular fracture of the scaphoid – the fracture line is within the joint cavity of the wrist;
- Extra-articular fracture – a tear in the navicular bone;
- De Kerwen fracture – simultaneous fracture of the navicular bone and displacement of its proximal fragment and crescent bone from the carpal joint.
Symptoms include pain and swelling at the base of the thumb, an inability to move the hand in the wrist, and make a fist. The diagnosis is made based on the patient's symptoms, the nature of the injury, examination, and X-rays of the carpal bones. If there is no displacement of the fragments, sometimes the line of fracture cannot be determined by all the signs. In this case, immobilization is maintained, and X-rays are repeated after 7-10 days, when the fracture line becomes clearly visible due to the activation of the regenerative processes.
Treatment consists of immobilization in a cast for 4 weeks, followed by follow-up assessment and prolongation of immobilization if fracture consolidation is insufficient. If the fracture is displaced and spread, closed fixation is ineffective and fixation of the navicular fracture with a spoke is indicated. Fractures of the ankle are often complicated by the formation of a false joint or by the lysis of bone fragments due to damage to the blood vessels that supply them during the injury. That is why it is so important to follow all the doctor's instructions and take x-rays in a timely manner in order to avoid complications and deterioration in the functioning of the wrist. After repair of the scaphoid, physiotherapy and physical therapy are indicated to restore wrist function.
Surgery for fractures of the leg bones
Conservative treatment is possible only for closed, simple injuries that are not displaced and where there is no risk of dislocation and possible blood loss. In this case, complete immobilization of the limb with a plaster cast is performed.
In all other cases, surgical treatment is indicated. Different types of surgical interventions are used in traumatology, depending on the type of leg fracture and the likely negative consequences for general health.
- osteosynthesis. This technique is aimed at restoring the integrity of the bone structures by assembling the fragments using special fixators – plates, spokes, pins.
- bone graft. A surgical method of treatment in which damaged areas are replaced with other materials: autologous or donor bone, biosynthetic analogues.
- repositioning. A surgery in which the anatomically correct position of bony structures is restored in an open or closed position and then secured by external fixation with a cast or splint.
In complex cases with multiple diseases, especially in elderly patients, an endoprosthesis is used.
rehabilitation
The length of inpatient treatment ranges from 1 to 5 days, depending on the complexity of the fracture and the treatment procedure. During this period, antimicrobial and anti-inflammatory treatment is carried out, as well as measures to prevent thrombosis and edema.
After discharge from the hospital, basic recommendations must be followed:
- do not put weight on the injured limb;
- Move only with aids (crutches, canes or other aids);
- take prescribed medication;
- Visit the doctor regularly to monitor the healing of the injury;
- Physiotherapeutic treatments must not be neglected.
The length of rehabilitation depends on several factors, the main one being the severity of the fracture. On average, it is between 1.5 and 7 months.
First, call emergency services: Only a qualified doctor can determine what type of leg injury the patient has suffered and how severe the fracture is, based on the characteristic symptoms. Do not move or turn the injured person yourself, do not give him personal medication, and do not try to fuse the edges of the wound if the fracture is open. Just immobilize the limb and cover the wound with a clean cloth to prevent foreign objects from entering.
No. There are cases when after falls, bruises and traffic accidents, the patient did not experience swelling or pain, but an actual fracture was detected. Sometimes in such cases the symptomatology does not develop immediately, but only 1-2 days after the injury.
Kornilov, NV Traumatology and orthopedics: a textbook / edited by NV Kornilov, AK Dulaeva. – 4th revised and updated edition – Moscow: GEOTAR Media, 2020.
Rudy TP, Buckley RE, Moran KG. – AO – Principles of fracture management, 2nd edition, 2013.
Read more:- Bone structure of the navicular foot.
- tibia and fibula.
- fracture of the ankle.
- Fracture of the lateral condyle.
- Displacement fracture of the heel bone.
- Bones of the tarsal bone of the hand.
- Fracture of the calcaneus of the foot.
- Cracked metatarsal.
