May result from trauma, previous fracture dislocation or dislocation in the Lisfranc joint, fracture of the sphenoid bones, secondary to diabetic arthropathy (Charcot foot), rheumatoid arthritis. A highly heterogeneous group of disorders involving multiple joints, including the tarsal and metatarsal joints, presenting as arch and instep pain. Conservative treatment relieves pain symptoms by wearing orthopedic shoes, insoles, and painkillers, while radical treatment consists of arthrodesis of the affected joints and corrective osteotomy to restore normal load distribution to the foot. You can read more about osteoarthritis in this article.

- The foot is the second heart of the human body in Moscow
- The most important areas of the foot
- ICD-10
- classification
- diagnosis
- Treatment
- Treatment before hospitalization
- Conservative treatment
- Surgical interventions
- Roman foot - a measure of length
- The Celtic foot - a mix of cultures
- Pain within foot elevation.
- Lisfranc joint injury
- What is a flat foot?
- List of 10 Most Effective Flatfoot Exercises for Adults by KP
- Walking on an uneven surface
- Three points of support
- calf stretch
- Yoga for the toes
- Possible causes of foot pain when walking
- The most common foot diseases
- What diseases cause foot pain?
- Diagnosing the pathology of metatarsal pain when walking
- foot and bunion of the big toe
- How to tell if you have a foot problem
The foot is the second heart of the human body in Moscow
The foot is the second heart of the human body.He is responsible for the life of the body.
The foot is an important part of the human body. It is even called the 'second heart of man'. Because on the arch of the foot there are reflex points for many organs and many important channels. In total there are more than 60 active zones that are responsible for various organs and their functionality.
Thousands of years ago, people realized that those who walk a lot feel good, and longevity - these are mostly mobile people. Ancient doctors lifted the seriously ill to their feet very early, which enabled them to recover more quickly and without complications.
Normal mechanical activity at the soles of the feet activates the whole body: as soon as a person stands up, activation signals flow from the soles of the feet to all corners of the body, but as soon as they sit or lie down, the signals stop.
Doctors have now discovered that there are more than 70,000 nerve endings on the soles of our feet. These connect certain areas of the sole surface with organs, body regions and even with certain body systems.

The most important areas of the foot
Why cold and wet feet lead to colds or respiratory diseases
For this reason, wet feet are the most common cause of colds, which are accompanied by a runny nose and headache. The left paranasal sinuses are on the left fingertips and the right paranasal sinuses are on the right fingertips.
Even walking a little increases visual acuity and intraocular pressure normalizes.
- The inner ear, pharynx and bronchi are located on the front and sole of the foot.
- So when your feet get cold and wet, you can't avoid a cold with a cough, runny nose, and ringing in your ears.
- If you have frostbite. The upper part of the front arch of the foot at the base of the second and third toes freezes and can spread to the lungs.
In adults, whose immune systems are usually strong, cold and wet feet do not always lead to a cold. In children, on the other hand, there is a very close connection between feet and health.
ICD-10

Foot deformities are a group of pathological conditions that affect the appearance of the foot. This group includes a variety of anomalies resulting from trauma, malformations, paralysis, paraparesis, and many diseases. The severity of foot deformities and disabilities can vary widely, ranging from almost complete preservation of function to severe disability. However, even minor foot deformities negatively affect the upper body, causing pain, fatigue when walking, poor posture, premature muscle fatigue in the back and lower limbs, and ultimately increase the risk of developing osteochondrosis and arthrosis in the small and large joints of the lower limbs .
Foot deformities are treated by orthopaedists/traumatologists. Depending on the cause of this pathology, neurologists, neurosurgeons, rheumatologists and other specialists may also be involved in the treatment.

classification
There are the following basic types of foot deformities:
- horseshoe– Accompanied by a sustained plantar flexion (plantar flexion). Active dorsiflexion of 90 degrees or less is not possible or only possible with difficulty. In severe cases, even passive flexion cannot return the foot to its normal position.
- heel foot – Is characterized by sustained dorsiflexion. In severe deformities, the posterior surface of the foot touches the anterior surface of the tibia.
- Hollow foot (rigid, supinating). – This is accompanied by an increase in the curvature of the longitudinal arch. In severe cases, the patient relies only on the heads of the metatarsal bones and the tuberosity of the heel bone, with the metatarsal bones not touching the surface.
- Flatfoot (soft, pronated) – Characteristic is the flattening of the transverse or longitudinal arch. In the case of longitudinal flatfoot, the foot does not lie on the surface with the outer edge, as is normally the case, but with the sole of the foot. Transverse flatfoot is associated with a widening of the forefoot and an increase in the distance between the heads of the metatarsal bones.
In practice, a combination of several types of foot deformities often occurs. In addition to the condition of the bones, joints, tendons and ligaments, the size and type of deformity can be influenced by pathological changes in the upper extremities, especially the ankle.
diagnosis
The neurologist is responsible for determining the cause of the numbness in the foot. Patients with vascular disease are referred to a vascular surgeon. An endocrinologist is involved in examining patients with diabetes. The doctor determines when and under what circumstances the sensory disturbance occurred, how the symptom has changed over time and what side effects there are. The following procedures can help confirm the diagnosis:
- Physical examination. The specialist assesses the appearance of the foot, the color and temperature of the skin, and the pulsation of the arteries. He notes signs of swelling and inflammation, hyperkeratosis, cracks, abrasions, trophic ulcers.
- Neurological examination. The doctor examines the reflexes, determines the limits of abnormal sensitivity, the presence of muscle wasting, neurogenic contractures.
- Examination of the vessels .. The state of the arteries is examined using ultrasound, duplex, reovasography, capillaroscopy, thermography and peripheral arteriography.
- Electrophysiological Methods. Electromyography and electronography are used to differentiate neuropathies and determine the extent and severity of lesions.
- visualization techniques. Soft-tissue ultrasound, spinal X-rays, CT or MRI of the brain, and other investigations may be recommended to clarify the origin of the pathology.
- laboratory tests. Laboratory tests include determining the levels of sugar and cholesterol in the blood. Specific marker tests are performed to determine the nature of the underlying pathology in Raynaud's syndrome.

Treatment
Treatment before hospitalization
Suspected spinal cord injury requires spinal immobilization and immediate transfer to a neurosurgical hospital. First aid measures for nerve injuries depend on the type of injury. Injured with wounds should be dressed with an aseptic dressing. For all leg injuries, especially severe swelling, the limb must be elevated. If you experience numbness or swelling after putting on a cast, you should go to a trauma center immediately to have the cast removed.
Conservative treatment
In neuropathy, the etiological factor is treated as much as possible. Circulatory agents, NSAIDs and B vitamins are prescribed. In the case of pain, therapeutic trigger point blockades are used. The list of non-pharmacological methods includes UVA, diadynamic therapy and UHF. Massage, manual therapy and physical therapy play an important role.
For vascular disorders, anticoagulants, antispasmodics, vitamins, and drugs to reduce red blood cell aggregation are recommended. Severe pain is an indication for analgesics, paravertebral and paranephral blocks. Patients with acute vascular occlusion are treated with thrombolytics and anticoagulants.
Non-medical treatments for vascular pathologies include hyperbaric oxygenation, VLBI, ozone therapy, mud packs, magnetic therapy, UHF, therapeutic electrophoresis, pearl, radon and hydrogen sulfide baths. Bandages and laser therapy are used in patients with trophic ulcers.
Numbness in the feet due to diabetes requires adjustment of the insulin dose or switching the patient to insulin therapy. The pharmacological treatment consists of anticonvulsants, a-lipoic acid and infusion solutions. Bandages and antibiotic therapy are indicated for ulcers.
Surgical interventions
Depending on the etiology, with numbness in the feet, the following operations are performed:
Roman foot - a measure of length
The Romans left footprints throughout Europe and North Africa during their conquests. They invented the 'foot' - a measure of length still used in Britain today.
The Roman foot can be recognized by the three toes of equal length, starting with the first. It is believed to be characteristic of a quarter of the world's population. It is not uncommon in Roman art, although many statues also feature the Greek foot. The Romans often copied the work of Greek sculptors.
It is more difficult for people with this foot shape to find comfortable shoes. Shoes with narrow toes, stilettos and high heels are particularly problematic as they put pressure on the ball of the foot.
The Celtic foot - a mix of cultures
The Celts are associated with Western Europe, particularly Britain, but their exact origins are uncertain. The shape of their feet and toes also suggests a mix of different cultures.
The shape of the Celtic foot is a combination of Germanic and Greek toe shapes. In this type, the second toe is longer than the rest, and the first and third toes are almost the same length. Genetic studies have shed light on the reasons for this combination.
The results show that regions of the UK where Celtic roots are prevalent such as Cornwall, Scotland, Wales and Northern Ireland are genetically distinct. This means that there is no uniform Celtic genetic group.

genetics of origin. haplogroups
The Romans left their mark all over Europe and North Africa at the time of their conquest. They invented the 'foot', a measure of length still used in Britain today.
A study using DNA samples from more than 6,000 Europeans supports this theory. According to the results, European populations have immigrated to modern Britain over the past 10,000 years.
The shape of the Celtic foot is possibly the result of the intermingling of several peoples.
Pain within foot elevation.
As with flatfoot, it is useful to distinguish between a constitutionally high arch and pes cavus, which rarely occurs in isolation. The sole of the foot can be high or low, but it can also simply be an anatomical feature.
With a pes cavus, the arch of the foot is very high and the instep has trouble fitting into the shoe. Most cases of pes cavus have a neurological cause.
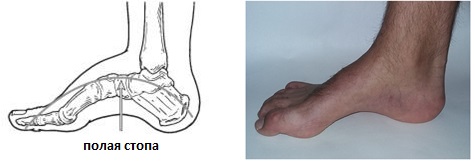
An inherited cause of pes cavus is Charcot-Marie-Tut disease. Hollow foot is the opposite of flatfoot; the arch of the foot can be so high that all of the stress is only distributed over the outside of the foot. It is also associated with a claw-shaped deformity of the toes. For example, in Charcot-Marie-Tooth disease, the extensor muscles of the toes take over from the weakened oculomotor and anterior tibial muscles, preventing the foot from sagging when walking. The constantly high tension of the extensor muscles causes a claw deformity of the toes. Hollow foot also significantly increases the risk of ankle ligament injuries and risk of stress fractures, as it leads to inefficient load distribution and reduced cushioning capacity when running. Learn more about pes cavus in this article.
Lisfranc joint injury
Lisfrancus fractures, lisfrancus joint dislocations and isolated lisfrancus ligament tears, while relatively rare injuries, are extremely important because they are very often missed during initial treatment and the consequences can be tragic. The typical mechanism of injury is a fall from a height or hitting a car pedal in an accident, but low-energy causes such as the foot rolling backwards are also possible. Immediately after the injury, there is pain and swelling on the sole of the foot, as well as bruising on the inside of the sole surface in the middle third. High-energy injuries can cause significant foot deformity and swelling, and support is impossible; in the case of isolated Lisfranc ligament injuries, the support function can be retained.

In all cases of Lisfranc ligament injuries, except grade 1-2 isolated ligament injuries, surgical treatment is indicated, otherwise painful osteoarthritis will develop in the tarsal joints and the longitudinal arch of the foot may collapse. If you had any of the above injury mechanisms and were diagnosed with a bruise or dislocation at first touch, but your foot has been in pain for a month or more, you should see a specialist. Read this article to learn more about Lisfranc joint injuries.
What is a flat foot?
With a flat foot, the normal arch of the foot is low or absent on the inside. The foot therefore appears flat and all or most of the sole is in contact with the ground. The support function of the foot - cushioning and balance - is impaired by the deformity of the foot.
A flat foot is unable to support the body in the correct position and absorb impact loads when walking and running. While harmless at first glance, flat feet often lead to disorders of the joints, spine and internal organs 3 .
The most common symptoms of flat feet:
- Changes in foot shape: flat feet, appearance of a 'bony' on the big toe, foot too wide;
- clubfoot when walking ;
- changes in posture and gait;
- Pain in feet, knees and hips 1 .
The most common cause of flat feet is muscle weakness. Less commonly, foot deformities are caused by congenital malformations, nervous system disorders, trauma, or excessive fatigue from prolonged standing. It is important to note that most children have physiological flat feet by age 5, which resolves with age with normal foot development 2 .

There are 2 main types of flat feet: flexible (movable) and rigid (rigid). In flexible flatfoot, the foot retains the ability to form an arch but flattens out when standing. The flexible flat foot is much more common and in many cases can be corrected, including with therapeutic exercises.
With a rigid flatfoot, the foot cannot form an arch. This is usually a result of the shape of the foot bones. This condition is rare and is unlikely to change with exercise 1 .
A distinction is also made between longitudinal and transverse flatfoot. In longitudinal flatfoot, the foot touches the ground with almost its entire surface and therefore increases in length. In transverse flatfoot, the foot is shorter and wider due to the fan-shaped extension of the metatarsal bones 1 .
List of 10 Most Effective Flatfoot Exercises for Adults by KP
our expert, Doctor of Physiotherapy and Sports Medicine, osteopath Yulia Tolmacheva has compiled 10 effective flatfoot exercises for adults. You can do these therapeutic exercises at home anytime. You don't need any special equipment for the training, you can do it with things that you always have on hand.
Walking on an uneven surface
This exercise requires minimal effort: you can just go barefoot. Uneven surfaces at home can be designed with special mats that imitate pebbles, cones, tree roots or spikes. Lay out the mat where you walk most often, e.g. B. in front of the kitchen. Irritation of the foot by an uneven surface causes a protective reflex and contraction of the foot muscles.
Three points of support
Starting position: sitting or standing, feet in line, knees facing forward. Place your feet so that you can feel the three points of support: middle of the heel, base of the little toe, base of the big toe. The balance between these points gives stability to the foot. Keep this balance for as long as possible.
calf stretch
Stand facing a wall and support yourself with both hands on the wall. Lay the leg to be stretched back with the knee straight and toes pointing forward.
Keep the back leg straight and press the heel firmly to the floor. Lean forward slightly until you feel a stretch in the calf of the back leg. Hold this stretch for 30-60 seconds. Repeat this 4 times for each leg.
For the stretch to be effective, don't let your foot sink inward. This exercise increases ankle flexibility and promotes proper foot placement.
Yoga for the toes
Lift the big toe up while pressing the other four toes against the floor. Hold the foot in this position for 5 seconds. Push the big toe down while lifting the other four toes. Hold this position for 5 seconds. Repeat the exercise 10 times for each foot.
Possible causes of foot pain when walking
Foot pain can be caused by many factors. The most dangerous are injuries and chronic diseases, which develop slowly but, if left untreated, lead to sensory disturbances and restricted movement.
When a person suffers from foot pain, it can be caused by diseases from the following groups:
Unfortunately, many foot diseases develop all three types of abnormalities over time, making diagnosis and treatment difficult. For example, joint diseases can lead to complications from nerve and vascular diseases: compression of nerve roots, vasoconstriction, poor blood circulation and other disorders. In such cases, a comprehensive diagnosis is required to determine the cause of the pain.
Pain in the ankles when walking can be aggravated by the following factors
- smoking (causes poor circulation);
- hypothermia;
- Frequent trauma;
- infections;
- uncomfortable footwear;
- Excessive exercise;
- Obesity;
- dehydration.
Wounds are most commonly caused by wearing improper footwear for long periods of time. Flat-soled sneakers and ballet shoes are just as damaging to the foot as heels that are too high. Flat-soled shoes deform the foot over time, which often leads to flat feet. High-heeled shoes can deform the toes and arch of the foot. With timely medical treatment, however, the chances of correcting the deformation are high: acquired diseases in the early stages can be successfully treated conservatively with physiotherapy and massage.
Note: If trauma is the cause of foot and gait pain, treatment by a trauma surgeon is essential, no matter how minor the injury may appear. Neglected injuries lead to various chronic diseases and a gradual deterioration of the ligament-bone system.
The most common foot diseases
The most common reason why the foot hurts when stepping on it after a long period of rest is fasciitis, an inflammation of the connective tissue that can be accompanied by severe swelling. It is not uncommon for this disease to lead to complications such as heel spurs.
If the pain comes on suddenly (usually at night) and is accompanied by cramps, increasing swelling, and fever, the cause of the pain is probably gout. In this disease, excessive amounts of uric acid build up in the body, first in the joints and tophi under the skin, and then in the internal organs.
Infectious arthritis shows a similar clinical picture. The inflammation usually occurs when the infection enters the joint through a wound or after an illness such as a sore throat or food poisoning.
If the pain occurs regularly, osteoarthritis or non-infectious arthritis can be the cause. These cartilage abnormalities are characterized by the following features
- cracking or grinding when moving fingers or walking;
- Constant discomfort, which turns into pain with fatigue or prolonged exertion;
- limited mobility;
- Frequent swelling.
Connective tissue diseases can be controlled with comprehensive therapy and even completely eliminated in the early stages. However, osteoarthritis and arthritis, if not treated properly, lead to severe foot deformities, constant pain and reduced mobility.
What diseases cause foot pain?
Doctors know a number of diseases of different etiologies that cause pain. This includes:
- Arthritis;
- heel spur;
- ligament inflammation;
- Osteoporosis;
- Gout;
- flat feet;
- obliterating endarteritis;
- tendonitis;
- erythromelalgia.
1. Flat feet. If the foot hurts in the middle on the inside, a deformity may be the cause. Weak ligaments and muscles, heavy loads, pregnancy - all of these affect the arch of the foot. No one is immune to this pathology at any age.
There are different types of flat feet:
Swelling, cramps and tired legs are the most harmless consequences of flat feet. The disease damages the spine because the load is not properly distributed, so the entire musculoskeletal system suffers. Especially the longitudinal arch of the foot hurts.
To remedy this, those affected are advised to wear insoles and take painkillers. It is necessary to undergo physical therapy, take vitamin complexes and perform therapeutic exercises. Early detection of the pathology allows for faster and easier treatment.
2. The heel spur, as the disease is popularly known, is called 'plantar fasciitis' in medical practice. It begins with inflammation of the connective tissue, and the affected person feels pain in the foot between the heel and toes. It is more common in people who have to stand on their feet for a long time. Over time, the heel bone deforms and the spur grows. This, in turn, traumatizes the surrounding tissue and further aggravates the disease.
As a rule, special shoes and various physiotherapeutic treatments are prescribed to eliminate the growth. In extreme cases, surgeons are involved in the treatment process. Rehabilitation after surgery is long and difficult, and the patient cannot walk for some time. Therefore, attempts are made to use conservative methods.
Diagnosing the pathology of metatarsal pain when walking
The first specialist who visits a person with discomfort in the foot is a therapist. It is he who examines the limbs, identifies painful areas and makes referrals to specialized specialists.
The visual examination gives an impression of:
- the topography of the foot;
- swelling
- the mobility of the foot
- the gait;
- range of motion of the joint;
- skin condition;
- the position of the toes.
To determine the internal condition of the entire foot, the patient is examined:
The doctor may recommend urine tests, blood tests, and synovial fluid sampling.
foot and bunion of the big toe
The outflow of blood and lymph is disturbed when there is a disorder at one of the levels through which it flows: lower leg muscles, hamstrings, thigh muscles, small pelvis, abdominal organs, thoracolumbar diaphragm. A drainage disorder in these areas is manifested by swelling of the tissue surrounding the heel nerve. If the swelling persists for a long period of time, the thumb muscle weakens and a 'bone' forms.

Mechanical causes include prolapse of the arch of the foot and loss of thumb extension function. The foot is forced to seek an area of support when the big toe is not functioning. Bone tissue begins to build up to give stability to the stride.
Unfortunately, if you have surgery and don't change your lifestyle, the bone can grow back. Remember that any surgery is an injury to the body, which it compensates by putting stress on other areas. This can lead to lower back or hip pain.
How to tell if you have a foot problem
Examine the foot visually. Stand on one foot and put your body weight on it. Turn left and right. Notice how your body weight shifts to the outer and inner edges of the foot every now and then. What happens to the knee at this point? And with the femur.
I think you felt them all move in response to the movement of the foot. That's because that's where the chain reaction starts. The connection between the foot, knee and hip joint is obvious - they are connected by a limb. And what is invisible to the eye is in the deep line.
- heel or toe pain;
- flat feet;
- the ball of the foot hurts and grows;
- the little toe does not touch the ground;
- the big toe shows a 'fig'.
- postural problems;
- knee and hip pain;
- Can't pump up my glutes despite blogger's snazzy pop-up classes;
- Headache;
- bite changes and more
First, much of the motor work of the foot depends on proprioception - the sensitivity of this area. The nervous system collects as much information as possible and sends it to the cerebellum. There the information is processed and the right strategic decisions are made: how the movement should now be executed. How hard you can use your muscles to create the optimal movement with the minimum expenditure of energy. The signals to the brain must be clear.
Second, the biomechanics of the stride itself. Where is the main load in the stride when you throw off the brace? Ideally in the area between the first and second toe. How do we run and what is the first point of contact with the surface? If it's the heel, then this method isn't quite right. Try walking barefoot on gravel in the park. I'm sure it will feel different. Optimal for the biomechanics of this movement.
Read more:- Treatment of the hollow foot.
- arched foot.
- Equinos pes cavus.
- flatfoot μb.
- Longitudinal and transverse arches of the foot.
- flat feet (valgus foot).
- Foot.
- Which ligaments strengthen the transverse arch of the foot?.
