In flexible valgus deformity, the flexor tendon of the long toe is transplanted to the navicular bone with subtalar arthroeresis (grade II).

- In children: valgus deformity
- Causes of deformities
- causes and symptoms
- Causes of deformities
- signs
- Inverted foot in a child
- signs
- What is a metatarsal adduction?
- Normal or pathological
- Flat foot pathology as a change in shape
- Reasons for the deformity
- Treatment
- Conservative treatment
- surgical treatment
- Clinical example #1
- Diagnosis of valgus in a 1 and 2 year old child
- What the treatment includes
- What to do and how to treat – remedies
- medication
- Symptoms of valgus foot
- diagnosis
- forecast
- signs
- Classification and stages of valgus deformity
- Advice and guidance from an orthopedist at the Perseus Orthopedic Center. Tel. 8 (495) 469-99-05
- Treatment of flat feet
- Orthopedic insoles (orthoses)
- How do you treat grade 3 valgus? Consultation with an orthopedist/traumatologist:
In children: valgus deformity
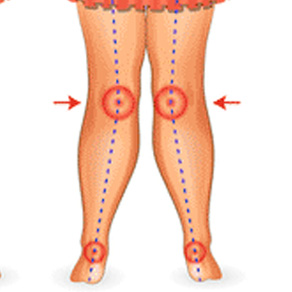
One of the most common orthopedic diseases in children is flat valgus deformity, which is characterized by a lowering of the arch of the foot and an X-shaped deformation of the foot axis. These changes are accompanied by an unsteady gait, rapid fatigue when walking, and muscle and joint pain in the lower limbs. Diagnosis, correction and prevention of valgus deformity in children are treated by pediatric orthopedists and traumatologists.
It is an axial deviation of the lower limbs in which the foot is turned outwards, the heel is displaced and a large gap is created between the ankles. A child with this condition places their feet in a cross shape when walking and rotates the forefoot in opposite directions. If the foot flattens, it is called a flat foot deformity.
The pressure exerted on the feet and spine when walking is abnormally distributed and shifts to the inside of the foot, causing pain after standing or walking for a short time. In children, the likely consequences of valgus deformity also include curvature of the spine, impairment of motor coordination and, if the condition is severe, disability with subsequent limitation of the ability to work. In addition, schoolchildren and adolescents with foot deformities are often psychologically impaired because they do not look the same as their peers due to a cosmetic defect.
Causes of deformities
Experts differentiate between congenital and acquired forms of the disease. Congenital valgus in children can be caused by
- underweight at birth;
- infectious or inflammatory diseases in the mother or fetus;
- Severe prematurity associated with underdevelopment of major body systems;
- Congenital connective tissue and bone abnormalities;
- Neuromuscular and genetic diseases (cerebral palsy, polyneuropathy)
- Congenital dislocations and dysplasia of the hip joint;
- Inherited features of the foot structure.
Factors that can promote foot deformity throughout a child's life include:
- Acute infections affecting connective tissue structures;
- Excessive physical exertion;
- Obesity;
- Rickets;
- Frequently recurring respiratory diseases with complications;
- Various injuries to the lower limbs with damage to muscles, ligaments, cartilage and bones;
- Inappropriate choice of footwear made from soft, ill-fitting materials.
In some cases, parents or close relatives unknowingly provoke X-shaped deformities of the lower limbs themselves by putting the child on his feet early and using a walker when the toddler is not even sitting.
causes and symptoms
Think about what is causing and making the problem worse.
Causes of deformities
- Injuries and damage to the cervical spine and vertebrae.
- Shortening of the lower limbs.
- Poliomyelitis and cerebral palsy.
- Tears of muscles, tendons and joints.
- Consequences of a stroke.
- Development of flat feet.
- Poor metabolism.
- Obesity.
- Inappropriate footwear.
- Innate genetic predisposition.
- Weak immune system after an infection.
- Improper use of plaster casts.
- Arthritis.
- CEREBRAL PALSY.
- Other serious illnesses.
These symptoms are easy to diagnose if properly treated by the treating doctor. They can be corrected, especially if the problem occurred before the age of one. The treating orthopedic surgeon will detect the difficulties using ultrasound or MRI scans or by visual inspection.
So how should parents identify a problem? Pay attention to the following points.
signs
- Unsteady, wobbly gait. The child walks slowly, does not walk fully, and tries to stand only on tiptoes.
- Crying and unwillingness to leave.
- The child begins to limp on one leg.
- It doesn't want to run, it just wants to walk or crawl.
- It compresses the inside of his arch.
If you experience any of these symptoms, consult a podiatrist at your health center to prevent further damage.

Inverted foot in a child
This is a congenital, uniform deformity that is classified as a type of clubfoot. It occurs in the first year of life when the child learns to walk. In half of the cases it resolves spontaneously before the age of three. However, this is not a reason not to consult a doctor.
signs
The body weight is placed unevenly on this area and the arches do not cushion the child's weight. To identify this defect, the doctor pays attention to the following signs
- Heel rotation – outward;
- Inward deviation of the metatarsal bones;
- an increase in the distance between the toes;
- appearance of calluses;
- swelling, redness;
- discomfort when walking;
- The big toe is turned inwards.
It is not advisable for parents to carry out the examination themselves. It is better to make the diagnosis in the hospital. The disease manifests itself as follows:
In this case, the child stands on his heel, but crooked, leaning on the outer part. The child starts walking from the inside edge and falls to the outside edge. The steps are wobbly and shallow.
What is a metatarsal adduction?
It is mostly seen in infants and disappears before the first year of life. The front part of the arch of the foot faces inward. The middle and back parts remain in the same position, and the child does not yet try to walk on tiptoes.
However, the condition does not go away on its own. It is important to see a doctor to prevent it from developing into flat feet or arches.
Normal or pathological
When making a diagnosis, you should remember that such a condition can affect anyone. And it is considered normal. But a lack of treatment will deprive your children of a normal life and a long healthy life. Therefore, do not give up treatment. Further development of the disease can be prevented by orthopedic shoes, which you can find in our catalog.

Flat foot pathology as a change in shape
This disease belongs to the orthopedic type, that is, it is a curvature of the foot in which the dependence on the inside of the foot predominates and the toes arch outwards. Many parents notice a flat foot deformity in their child as early as 1 year old. What should be done during initial treatment? Experts recommend starting by wearing special shoes.
In general, the problem is often not diagnosed until after the age of four, when the body is more mature and the abnormal arch formation is clearly visible. This pathology is a rare condition that, if left untreated, can cause flat feet and many other related problems up to the age of six.
As the disease progresses, the heel and toes may become crooked and the middle part of the foot bends inward. A valgus deformity is easy to recognize in a child - you can put the feet next to each other, and if they look like an X or close to it, it is an adverse change.

Reasons for the deformity
The main and most common causes of valgus deformity are parents' attempts to put the child on his feet and the relatively early start of walking - at the age of 8-10 months. The child must be ready to go, overcome fears and have the strength to do so. Forcing it too early puts unnecessary pressure on an immature body, leading to undesirable consequences.

In addition, there are other symptoms, factors and causes that lead to:
- Complications after rickets;
- Postnatal injuries most commonly affecting the hip joint;
- Increased body weight, which puts a lot of strain on the lower limbs;
- Injuries to the musculoskeletal system and legs;
- Poliomyelitis;
- Poor muscle development.
It is very important to choose appropriate, comfortable orthopedic footwear to ensure softness and freedom of movement. Flat soles should be avoided and a special bend for the heel is important. Orthopanda offers a large selection of high-quality products, where you will be amazed by the good prices as well as the good selection.

Treatment
Conservative treatment
- Choosing sensible footwear, wearing orthopedic shoes.
- Avoiding heavy foot strain and long walking.
- Wearing orthopedic insoles.
- Physical therapy.
- Massage, physical therapy.
- NSAID tablets, ointments and injections.
If treatment is neglected, the deformity may progress and other foot deformities and complications may arise:
- Constant pain in the foot.
- Swelling of the ankles and metatarsals.
- Deformation of the first toe, deformation of the other toes.
- 'Nodule' at base of first toe.
- Pain in ankle, knee and hip joints.
- Osteoarthritis of the foot, ankle arthritis, knee arthritis.
- Diseases of the spine.
surgical treatment
When choosing surgical treatment, the following factors are taken into account
- Degree of dysfunction of the tibialis posterior muscle tendon (TPMS).
- Mobility of the foot (deformity).
- Radiological features of longitudinal flatfoot.
- Presence of osteoarthritis of the metatarsal and tarsometatarsal joints.
For reversible flexible flatfoot deformity, arthrodesis of the subtalar joint (grade I) is performed.
During this surgery, an implant is inserted into the talar sinus, which limits the range of motion of the subtalar joint. If necessary in combination with tenotraplasty and achilloplasty.


Clinical example #1
Patient B., 22 years old, diagnosed with a flexible, hypermobile left foot.
The patient underwent an isolated subtalar arthrodesis of the left foot. 

Flexible flatfoot before and after surgery
Diagnosis of valgus in a 1 and 2 year old child
It is difficult to make an independent diagnosis. An examination by an orthopedic surgeon is required. He or she will visually view the arches of the feet, perform computerized plantography and podometry. If the doctor does not do this and limits himself to a cursory examination, another doctor should be sought and a neurologist should be consulted to rule out other problems.
Depending on the etiology, the traumatologist can distinguish between:
- static – due to poor posture;
- structural – caused by a congenital malposition of the talus;
- compensatory – caused by a short Achilles tendon and a crooked tibia;
- Corrective pathology – if the child has not been treated for clubfoot;
- traumatic.

What the treatment includes
A child's foot is shaped and corrected between the ages of 6 and 12. Therefore, many problems are identified and treated at this age.
Dr. Komarovsky advises that therapy should be aimed at strengthening the ligaments and shaping the arch of the foot. The orthopedist should recommend massage, bath therapy, magnetic therapy, swimming, electrophoresis and physical therapy.
Only if results are not achieved is the patient referred for surgery.

Prevention consists of walking on pebbles, grass, rolling a ball or roller. Physical activity – cycling, swimming, running – is also recommended.
Failure to follow the above measures can lead to disability, joint problems, musculoskeletal disorders, wear and tear on the knees and discs in the spine.
What to do and how to treat – remedies
To relieve pain and correct the anatomical shape of the bones, it is necessary to eliminate progressive diseases such as obesity or rickets, purchase orthopedic shoes and walk barefoot more often.

- Bandages are splints that are worn permanently or overnight. They are made from silicone or plastic. The bandage applies pressure to the protruding bone, relieving pain, making walking easier and preventing further curvature.
- Sinusoidally modulated currents. In this method, the electrodes are attached to the lower leg with elastic bandages. The painless and safe charge travels along the ligaments and stimulates the nerve endings.
- Bandage – ensures immobility of the joint. There are non-weight-bearing bandages that are only worn while sleeping and functional bandages that are intended for physical activities. They are made individually based on an impression of the arch of the foot.
- Baths with salt, iodine, pine needles and chamomile.
- Massage of the lower limbs – 10-20 sessions, repeated every two months.
- Finger exercises – rolling, grasping small objects with your fingers, walking on tiptoes.
- Orthoses and supinators.

medication
Orthopedic surgeons prescribe a variety of medications—injections, ointments, gels, and tablets—to relieve pain and tension during nonsurgical treatment. To relieve pain, the doctor prescribes the following medications, among others:
Non-steroidal drugs such as flurbiprofen, piroxicam, ketoprofen, amidopyrine, aspirin are prescribed to relieve inflammation. Prescribed gels include Diclofenac, Voltaren and Valgus Stop.

Symptoms of valgus foot
The patient feels pain when walking or under static stress, especially with unsuitable footwear. Stiffness, muscle pain in the lower leg and gait disturbances may also occur. In severe cases, the pain syndrome becomes almost permanent. The external examination reveals a number of typical changes: The patient does not stand with the outer edge of the foot on the ground, but with the entire surface of the foot; there is a dorsiflexion of the forefoot in relation to the rear foot.
Below the medial malleolus there is a bulge caused by displacement of the talar head. In some cases there is a protrusion of the corner of the navicular bone under this projection. The forefoot is adducted relative to the rear foot. The long axis of the foot is curved. The heel is tilted outward and rests on the ground with the inner edge rather than the medial part. The outer malleolus is flattened, the inner malleolus protrudes.
When the feet are together, the heels are spread. The stirrup, which originates from the medial part of the calf muscle, is located on the inside of the heel. Palpation reveals painful points on the inner edge of the plantar aponeurosis, below the scaphoid, and just above the outer apex of the ankle. Diffuse pain in the lower leg muscles is also not uncommon, particularly on the posterior surface of the shinbone above the heel (lower part of the calf muscle), on the inner surface of the shinbone, and near the anterior tibial plateau. The muscle pain is caused by increased stress and constant tension due to dysfunction of the foot.
The pathology usually occurs in childhood. If left untreated or inadequately treated, the deformity persists throughout life, but patients do not seek medical attention until functional impairment occurs. A relapse can occur at any age. In teenagers and young adults, valgus deformity may worsen with the onset of pain.
In more mature and elderly patients, the morphological changes usually do not worsen and functional impairments predominate. Valgus pain syndrome in adulthood is more likely to occur against the background of increased stress and changes in the general condition: in the last months of pregnancy, with rapid weight gain, during menopause and after prolonged hypodynamia due to a change in living conditions or bedrest due to a serious illness.
diagnosis
The diagnosis of valgus deformity is made based on external symptoms and instrumental findings. During the external examination, the doctor notices a flattening of the arch of the foot, a bulging of the inner ankle and a flattening of the outer ankle as well as an outward tilt of the heel. To confirm the diagnosis and determine the extent of the deformity, plantography, x-rays of the feet and podometrium are performed.
The x-rays show a reduction in the height of the arch, forefoot, metatarsal and hindfoot displacement as well as individual bones in the tarsal joints. Podometry is used to assess the distribution of stress on the foot. Computer plantography is used to calculate angles, parameters and indices to determine the presence and type of flat foot.
Patients with spastic and paralytic deformities are referred to a neurologist or neurosurgeon for consultation. If an endocrine disease is suspected, an endocrinologist must be consulted. If osteoporosis is suspected, densitometry, dual x-ray absorptiometry or photon absorptiometry is required. If the osteoporosis is due to menopause, the patient should see a gynecologist.
forecast
Valgus deformity in children can reach severe levels and can be not only a serious cosmetic defect, but also lead to functional impairment of the limb and even disability at a young age. If the degree of deformity is small and treated early enough, complete recovery of foot function is possible.
To prevent the development of valgus deformity in children, loading the child's lower limbs should be avoided until the age of 7-8 months. A good hardening diet, gymnastics, preventive massages, appropriate nutrition, adequate sleep and walks should be observed. It is important to prevent rickets and take vitamin D and micronutrients.
Regular visits to the pediatrician are necessary, as are preventive examinations by specialists in various disciplines (including pediatric surgeons and orthopedists). Attention should be paid to the correct choice of shoes for the child: they must be the right size (neither too small nor too large), made of high-quality natural materials, well padded and have a rigid back and sidewall.
signs
- Bulging at the base of the big toe
- Swelling, redness of the skin, soreness when touching the skin of the metatarsophalangeal joint of the big toe
- Persistent or temporary pain in the thumb area that may worsen when walking or wearing shoes
- limited mobility of the thumb
- Calluses in the friction zone between the 1st and 2nd.
The following factors play a role in the development of a valgus deformity:
- Presence of a congenital foot deformity (flat foot)
- Systemic diseases (rheumatoid arthritis)
- High pressure load on the foot, which can be associated with professional activities or professional sports
- Genetic predisposition (ligament and muscle weakness)
- Wearing unsuitable, tight footwear.
Classification and stages of valgus deformity
Valgus deformity is divided into stages as follows:
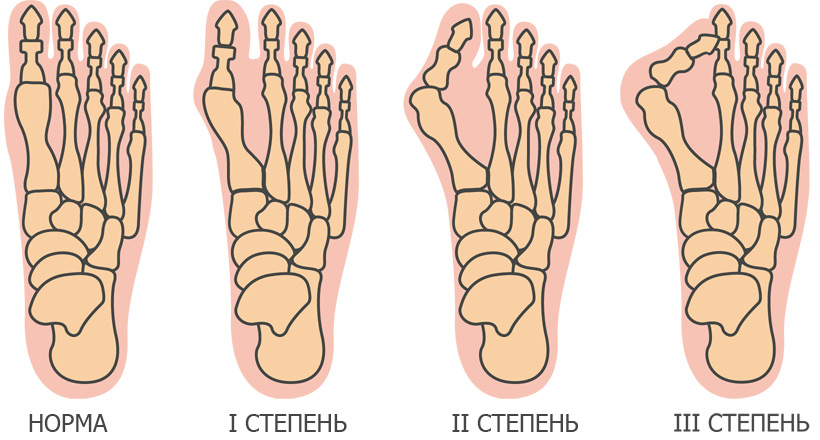
- Degree 1 – the angle of deviation of the big toe is less than 20°.
- Degree 2 – deviation angle between 25° and 35°.
- Degree 3 – deviation greater than 35°.
The stage is determined by the position of the heel in relation to the tibial axis:
- Level 1 – the foot is flat, the deviation is up to 15˚.
- Level 2 – the deviation angle is between 15˚ and 20˚.
- Level 3 – Angle 20˚-30˚, correctable
- Level 4 – Feet flat, slope over 30˚
Advice and guidance from an orthopedist at the Perseus Orthopedic Center. Tel. 8 (495) 469-99-05
- Orthopedic Surgery
- Consultation with a podiatrist
- online consultation
- Visit a specialist
- Manufacture of footwear
- Orthotics, traction insoles
- Orthoses and braces for the lower limbs
- Stabilization in cerebral palsy
- Insoles for clubfoot.
- With reinforced arch support
- For the dynamic rail
- For children
- teenagers
- Adult
- Home
- Supportive footwear for prostheses and aids
- For diabetics
- Tactical shoes, military shoes, outdoor and hiking shoes
- Custom insoles
Causes, diagnosis and modern treatment methods for flat feet. Treatment methods for flat feet. 12
1 Orthopedic flat or composite footwear with a standard fit.
orthopedic insoles

Orthopedic skeletal insoles

Silicone orthopedic insoles

Orthopedic frame insoles for model shoes

Orthopedic silicone insoles
Massage, manual therapy
Schedule an appointmentTreatment of flat feet

Flat foot is a deformity that involves loss of the longitudinal arch and an outward tilt of the back of the foot. clubfoot occurs in 20 % of adults. Almost all children are born with flat feet. As the child grows, the arch of the foot develops. If the connective tissue is weak and the growth process is disturbed, the flattening of the foot becomes permanent and requires orthopedic care.
Flat feet are characterized by a change in the shape of the foot. There is a prolapse of the arch of the foot, both longitudinally and transversely. In some cases, two types of flat feet can occur at the same time.
Transverse flatfoot It is a flattening of the transverse vault. The forefoot rests on the heads of the 5th metatarsal bone. At the same time, the foot reduces its length. Longitudinal flatfoot is characterized by a flattening of the longitudinal arch. The sole of the foot more or less touches the ground and is also longer.
The treatment of flat feet in adults and children is only effective if detected at an early stage. In these circumstances, comprehensive treatment can produce satisfactory results. Treatment of flat feet is most effective when using orthopedic shoes and physical therapy. A complex of measures makes the treatment most effective. At our center you will receive the necessary advice and treatment.


Orthopedic insoles (orthoses)
Effective for rational distribution of static load on the foot, cushioning in various types of foot deformities. For flat feet with functional insufficiency, in addition to massages, mandatory daily physiotherapy and physiotherapy, it is advisable to use individual insoles to properly support the foot.
Taking into account the international and national experiences, the materials and the impression technologies used in insoles, Schumacher insoles, etc. They often do not provide adequate correction, they cause discomfort when patients wear the shoes constantly, and the products are labor-intensive and time-consuming to manufacture. The latter is particularly important given the child's continuous growth.
In recent years, orthopedic techniques for correcting the foot have undergone significant developments.
The use of orthoses allows the orthopedist to create an individual orthosis that takes into account the anatomical-physiological and static-dynamic characteristics of the child's foot and, when viewed dynamically, offers the possibility of remodeling the material in the future in order to adapt the insole once formed . molded insole.

The finished insole has a thickness of 2 to 3 mm, which makes it easy to use in all children's shoes. A prefabricated insole is used in children's shoes, which offers the possibility of a inner and outer femoral beams to correct valgus foot deformity..
The forefoot and rear foot are made of soft material to ensure the correct sequence of step elements: heel strike, roll-off and toe strike, dynamic correction. For hallux valgus, a metatarsal corrector can be made to expose the transverse arch and stop the idiopathic deformity.
How do you treat grade 3 valgus? Consultation with an orthopedist/traumatologist:
If your child suffers from grade 3 valgus, it is advisable to only walk barefoot on a massage mat as part of the treatment and the rest of the time in special fall-proof footwear, which must be equipped with the following insoles individual orthopedic insoles.
The child has connective tissue weakness syndrome. The ligaments and tendons are not sufficiently strengthened (they are delayed).
The aim is to keep the feet in the correct, physiological position until the ligaments have achieved the necessary strength. This will inevitably happen, but the timing is different for each person.
The normal age is up to the age of 5, in some at the age of 10, in others only at the end of skeletal growth at the age of 16-18. If orthotics and proper footwear can support a normal arch, the ligaments will repair it. When flat feet develop, the ligaments stretch and, as they become stronger, permanently fix the foot in a flat foot position.Recommended treatments are:
- 1. individual orthopedic insoles.
- 2. Orthopedic anti-collision shoes with a Thomas heel, high ankle boots or a heel set back by 1 cm. These are referred to as 'antivalgus'. – Google it. Wear them at home too.
- 3. Children under 5 years old should not do exercise therapy because they are still small and do not understand what you want from them. Try to do it in the form of a game.
- 4. Massage of the lower limbs with emphasis on the shins and feet 4 times a year for 10 sessions.
- 5. SMT stimulation on the lower legs and feet 4 times per year for 10 sessions.
- 6. Paraffin ozokerite on shins and feet 4 times a year for 10 treatments.
If flat valgus foot position is a problem, anti-valgus shoes should fit within a week.
- Shallow valgus deformity in children.
- Shallow valgus deformity in adolescents.
- Orthopedic shoes for women with valgus deformity.
- flatfoot μb.
- Flat clubfoot deformity.
- Flat shoes are harmful.
- Massage for flat feet.
- Bandaging the flat foot.
